(HEPA) Filters in the Era of COVID-19: Function 2 and Efficacy 3 4 5 David Christopherson1, William C
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

How to Comply with CDC Guidelines
1101 W. 13th St, Riviera Beach, Florida Phone: 561.848.1826 https://www.rgf.com/rgf-biocontrols How to comply with CDC Guidelines OVERVIEW Sections of text are extracted directly from the Federal Register Vol. 59, No. 208, 10/28194, to compile this pamphlet. This is not meant to be a substitute for the Guidelines, but a general overview of specific sections relevant to RGF BioControls and its products. Click here for a link: https://www.cdc.gov/mmwr/preview/mmwrhtml/rr5417a1.htm OUR MISSION We believe, once you understand the new CDC guidelines, you’ll understand why our products offer you the best means of compliance. This is based upon a design philosophy that each piece of equipment is designed to satisfy a particular problem and each problem can be satisfied by an individual or combination of products that complement each other. CDC ON NEGATIVE PRESSURE "To control the direction of airflow between the room and adjacent areas, thereby preventing contaminated air from escaping from the room into other areas of the facility. The direction of air flow is controlled by creating a lower (negative) pressure in the area into which the flow of air is desired. For air to flow from one area to another, the air pressure in the two areas must be different. Air will flow from a higher pressure area to a lower pressure area. " HOW RGF BIOCONTROLS CREATES NEGATIVE PRESSURE Our MICROCON ® ExC7 utilizes HEPA filtration and UV light (option) for various room exhaust options. Wall, window or ceiling mounted, they direct air to either outside, back to return air system or corridor. -

Automatically Detects and Cleans the Air You Breathe
Automatically Detects and Cleans the Air you Breathe FAMILY BUSINESS S I N C E 1917 WHAT’S IN THE AIR? Indoor air can be up to 5x more polluted than outdoor air. Bacteria / Viruses Odors Allergens VOCs (Pollen & Ragweed, Mold, Pet Dander, (Volatile Organic Compounds, $2650Dust Mites) Cigarette Smoke, Smog) BAD$60 AIR IMPACTS$2650 THE BOTTOM LINE BILLION $220 BILLION DOLLARS THE AVERAGE COST OF ONE evaporates from the $60 EMPLOYEE SICK DAY IS BILLION economy every year in lost $2,650 8 productivity from sick days.6 PRODUCTIVITY In fact the EPA estimates that SickPRODUCTIVITY Building Syndrome alone is responsible for $60 BILLION IN LOST REVENUE.7 $2650 $60 THE BENEFITS OF CLEANER AIR BILLION BREATHE EASIER 99.97% of harmful germs, allergens and particulates are removed safely and easily.* PRODUCTIVITY INCREASED PRODUCTIVITY 9 Improved indoor air quality improves mental tasks, like concentration and recall, and can reduce absenteeism due to illness. REDUCED ODORS A chemical-free approach to removing odors and VOCs that can trigger allergies and headaches. *as small as 0.3 microns HOSPITAL-TYPE FILTRATION AeraMax® Air Purifiers feature a 4-Stage Purification 4 system similar to those used in hospitals to effectively 3 2 reduce the presence of airborne germs, allergens 1 and odors in the office environment. 1 CARBON FILTER 3 AERASAFE™ Removes odors and ANTIMICROBIAL captures large airborne TREATMENT particulates. Built-in protection from the growth of 2 TRUE HEPA FILTER odor causing bacteria, Captures 99.97% of mildew, and fungi on airborne particles as the True HEPA filter. small as 0.3 microns, ™ including pollen, 4 PLASMATRUE ragweed and other TECHNOLOGY allergens, viruses, Creates an ionized field germs, dust mites and to help safely remove mold spores. -

ASHRAE Position Document on Filtration and Air Cleaning
ASHRAE Position Document on Filtration and Air Cleaning Approved by ASHRAE Board of Directors January 29, 2015 Reaffirmed by Technology Council January 13, 2018 Expires January 23, 2021 ASHRAE 1791 Tullie Circle, NE • Atlanta, Georgia 30329-2305 404-636-8400 • fax: 404-321-5478 • www.ashrae.org © 2015 ASHRAE (www.ashrae.org). For personal use only. Additional reproduction, distribution, or transmission in either print or digital form is not permitted without ASHRAE's prior written permission. COMMITTEE ROSTER The ASHRAE Position Document on Filtration and Air Cleaning was developed by the Society's Filtration and Air Cleaning Position Document Committee formed on January 6, 2012, with Pawel Wargocki as its chair. Pawel Wargocki, Chair Dean A. Saputa Technical University of Denmark UV Resources Kongens Lyngby, Denmark Santa Clarita, CA Thomas H. Kuehn William J. Fisk University of Minnesota Lawrence Berkeley National Laboratory Minneapolis, MN Berkeley, CA H.E. Barney Burroughs Jeffrey A. Siegel Building Wellness Consultancy, Inc. The University of Toronto Johns Creek, GA Toronto, ON, Canada Christopher O. Muller Mark C. Jackson Purafil Inc. The University of Texas at Austin Doraville, GA Austin, TX Ernest A. Conrad Alan Veeck BOMA International National Air Filtration Association Washington DC Virginia Beach, VA Other contributors: Dean Tompkins Madison, WI for his contribution on photocatalytic oxidizers Paul Francisco, Ex-Officio Cognizant Committee Chair Environmental Health Committee University of Illinois Champaign, IL ASHRAE is a registered trademark in the U.S. Patent and Trademark Office, owned by the American Society of Heating, Refrigerating and Air-Conditioning Engineers, Inc. © 2015 ASHRAE (www.ashrae.org). For personal use only. -
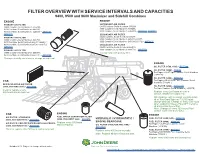
9400, 9500 and 9600 Maximizer and Sidehill Combines
FILTER OVERVIEW WITH SERVICE INTERVALS AND CAPACITIES 9400, 9500 and 9600 Maximizer and Sidehill Combines ENGINE ENGINE PRIMARY AIR FILTER SECONDARY AIR FILTER (9400 Combine Serial Numbers -655288, (9400 Combine Serial Numbers -655288, 9500 Combine Serial Numbers -645200, 9500 Combine Serial Numbers -645200, 9600 Combine Serial Numbers -645300) – AR80652, 9600 Combine Serial Numbers -645300) – AR80653, AR81313 AR82915 SECONDARY AIR FILTER PRIMARY AIR FILTER (9400 Combine Serial Numbers 655289-, (9400 Combine Serial Numbers 655289-, 9500 Combine Serial Numbers 645201-665977, 9500 Combine Serial Numbers 645201-665977, 9600 Combine Serial Numbers 645301-666172) – AR70107 9600 Combine Serial Numbers 645301-666172) – SECONDARY AIR FILTER AR70106 (9500 Combine Serial Numbers 665978-, PRIMARY AIR FILTER 9600 Combine Serial Numbers 666173-) – AR95759 (9500 Combine Serial Numbers 665978-, Change only with primary filter. 9600 Combine Serial Numbers 666173-) – AR95758 Change annually and clean or change as required. ENGINE OIL FILTER (9500, 9600) – RE57394 OIL FILTER (9400) – T19044 For Engine 6359T Upto Combine Serial Numbers ( -640100) OIL FILTER (9400) – RE59754 CAB For Engine 6068HH050 From Combine Serial Numbers (701246 -) RECIRCULATION AIR FILTER (9400, 9500 AND 9600) – AH115836 OIL FILTER (9400) – AH128448 For Upto Combine Serial Numbers ( -650370) Clean or replace every 200 hours and as required. Replace every 250 hours or once a season, whichever occurs first. Fill crankcase with seasonal viscosity grade oil or Torq-Gard Supreme™ (250 hours change interval). Change oil every 500 hours when using John Deere Plus-50™ II engine oil and a John Deere filter Note: Change oil every 100 hours if fuel contain more than 0.5% sulfur. ENGINE CAB ENGINE FUEL WATER SEPARATOR FILTER AIR FILTER, STANDARD HYDRAULIC / HYDROSTATIC / FUEL FILTER (9500,9600) – AR86745 (9400, 9500 AND 9600) – AH115833 (9400, 9500 ANDT 9600) – AT81478 ENGINE GEARCASE FUEL FILTER (9400) – AR86745 AIR FILTER, FOR OPERATORS WITH ALLERGIES Replace every 500 hours and as required. -

Fast Facts (PDF)
FAST FACTS According to the National Fire Protection Association, the leading factor contributing to home heating fires (30%) was mainly due to having a dirty chimney (i.e., creosote buildup). Heating equipment (including wood stoves) is the second leading cause of home fires, and third leading cause of home fire deaths. Most fireplace and chimney fires are caused by creosote buildup, and could be prevented. EPA believes there are approximately 13 million fireplaces, 250,000 hydronic heaters, and 8.5 million wood stoves in use nationwide. Five million (57 percent) of the nation’s wood stoves are older, inefficient devices. EPA estimates that if all of the old wood stoves in the United States were replaced with cleaner- burning hearth appliances, an estimated $56-126 billion in health benefits per year would be realized. Smoke from wood-burning stoves and fireplaces contain a mixture of harmful gases and particle matter (PM2.5). Breathing these small particles can cause asthma attacks and severe bronchitis, aggravate heart and lung disease, and may increase the likelihood of respiratory illnesses. Changing out one old dirty, inefficient wood stove is equivalent to the PM2.5 reduction of taking five old diesel trucks off the road. The benefits of replacing old wood stoves and fireplaces: • Saves money, fuel, time, and resources • Up to 50 percent more energy efficient, uses 1/3 less wood • Cuts creosote build-up in chimneys that helps reduce the risk of fire • Reduces PM2.5 indoors and out After start-up, a properly installed, correctly used EPA-certified wood stove should be smoke free. -

HEPA) Filter - Ultra Low Penetration Air (ULPA) Filter (Also Referred to As Extended Media
EPA-452/F-03-023 Air Pollution Cocntrol Technology Fact Sheet Name of Technology: Paper/Nonwoven Filter - High Efficiency Particle Air (HEPA) Filter - Ultra Low Penetration Air (ULPA) Filter (also referred to as Extended Media) Type of Technology: Control Device - Capture/Disposal Applicable Pollutants: Submicron Particulate Matter (PM) greater than or equal to 0.3 micrometer (µm) in aerodynamic diameter, and PM greater than or equal to 0.12 µm in aerodynamic diameter that is chemically, biologically, or radioactively toxic; hazardous air pollutants (HAPs) that are in particulate form, such as most metals (mercury is the notable exception, as a significant portion of emissions are in the form of elemental vapor). Achievable Emission Limits/Reductions: HEPA and ULPA filters are classified by their minimum collection efficiency. Many international standards and classes currently exist for high efficiency filters (Osborn, 1989). In general, HEPA and ULPA filters are defined as having the following minimum efficiency rating (Heumann, 1997): HEPA: 99.97% efficiency for the removal of 0.3 µm diameter or larger PM, ULPA: 99.9995% efficiency for the removal of 0.12 µm diameter or larger PM. Some extended media filters are capable of much higher efficiencies. Commercially available filters can control PM with 0.01 µm diameter at efficiencies of 99.99+% and PM with 0.1 µm diameter at efficiencies of 99.9999+% (Gaddish, 1989; Osborn, 1989). Several factors determine HEPA and ULPA filter collection efficiency. These include gas filtration, velocity, particle characteristics, and filter media characteristics. In general, the collection efficiency increases with increasing filtration velocity and particle size. -
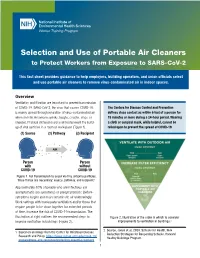
Selection and Use of Portable Air Cleaners to Protect Workers from Exposure to SARS-Cov-2
National Institute of Environmental Health Sciences Worker Training Program Selection and Use of Portable Air Cleaners to Protect Workers from Exposure to SARS-CoV-2 This fact sheet provides guidance to help employers, building operators, and union officials select and use portable air cleaners to remove virus-contaminated air in indoor spaces. Overview Ventilation and filtration are important to prevent transmission of COVID-19. SARS-CoV-2, the virus that causes COVID-19, The Centers for Disease Control and Prevention is mainly spread through inhalation of virus-contaminated air defines close contact as within 6 feet of a person for when an infected person speaks, laughs, coughs, sings, or 15 minutes or more during a 24-hour period. Wearing sneezes. Physical distancing alone will not prevent the build- a cloth or surgical mask, while helpful, cannot be up of viral particles in a room or workspace (Figure 1). relied upon to prevent the spread of COVID-19. (1) Source (2) Pathway (3) Recipient AIR Person Person with without COVID-19 COVID-19 Figure 1. For transmission to occur via tiny airborne particles, three things are necessary: source, pathway, and recipient.1 Approximately 40% of people who are infectious are asymptomatic (no symptoms) or presymptomatic (before symptoms begin) and may contaminate air unknowingly. Work settings with inadequate ventilation and/or those that require people to be close together for extended periods of time, increase the risk of COVID-19 transmission. The illustration at right outlines the recommended steps to Figure 2. Illustration of the order in which to consider improve ventilation in buildings (Figure 2). -

Effects of Temperature and Relative Humidity on Filter Loading by Simulated Atmospheric Aerosols & COVID-19 Related Mask and Respirator Filtration Study
Effects of Temperature and Relative Humidity on Filter Loading by Simulated Atmospheric Aerosols & COVID-19 Related Mask and Respirator Filtration Study A DISSERTATION SUBMITTED TO THE FACULTY OF THE UNIVERSITY OF MINNESOTA BY Chenxing Pei IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF DOCTOR OF PHILOSOPHY Dr. David Y.H. Pui, Advisor August 2020 © Chenxing Pei 2020 Acknowledgments First and foremost, I am deeply indebted to my advisor, Professor David Y. H. Pui, for his continuous guidance, mentoring, and inspiration throughout my undergraduate and graduate studies. He provided me with the encouragement and freedom to work on any filtration related studies that interested me. His support, patience, and trust have made my years spent in the Particle Technology Laboratory an enjoyable, enriching, and memorable experience in my life. I would like to express my deepest appreciation to my committee members: Prof. Thomas Kuehn, Prof. David Kittelson, and Prof. Kevin Janni for reviewing my dissertation, offering insightful comments and suggestions, and serving on my Ph. D. exam committees. I am extremely grateful to my committee members not only for their time and extreme patience, but for their intellectual contributions to my development as a scientist. I would also like to thank Dr. Qisheng Ou, whose help cannot be overestimated. Dr. Ou provided me with the tools that I needed to choose the right direction and successfully complete my dissertation. Special thanks to Dr. Young H. Chung, who led to many interesting and motivating discussions. His help and advice were invaluable for my research and life. Thanks also to Weiqi Chen, who collaborated with me on the smart sensor project. -

A Hybrid Air Purifier and Dehumidifier for the Best Possible Indoor Air
AD20 Hybrid / Air purifier & Dehumidifier A hybrid air purifier and dehumidifier for the best possible indoor air. & ER D AN EH Wood´s AD20 hybrid is a revolutionary innovation that LE UM C ID IF I R E I R E A CL AN E R A R I R I R E I A F combines Wood´s high standards for energy-effecient I D I C M L E U A H N E E D R & and reliable dehumidification, with Wood´s unique & R E N A E D L SWEDISH TECHNIQUE E C N U M I R D I I A F I E R Swedish filtration system and give you the best possible indoor air. Thanks to the patented filter system Active ION HEPA, manufactured in Sweden, AD20 Hybrid gives you an effective air cleaning-without compromising on power consumption or noise levels. Wood’s AD-20 Hybrid Specifications dehumidification AD20 Hybrid is reliable, efficient and energy-saving. Max. working area 100 m² Recommended area 2 - 60 m² AD20 Hybrid protects against moisture and mold dam- Capacity at 20ºC & 70% RF 10,6 litres/day age and also serve you with an air purifier in the same Capacity at 35ºC & 80% RF 20 litres/day Power at 27ºC & 60% RF 260 W machine. AD20 Hybrid is one of the smartest hybrid Power at 30ºC & 80% RF 310 W dehumidifiers / air purifiers on the market. Fan speeds 4 Airflow 100-200 m³/h Speed 1 100 m³/h Speed 2 130 m³/h Advantages: Speed 3 160 m³/h Speed 4 200 m³/h • Powerful and energy efficient dehumidification. -

Efficacy of Portable Air Cleaners and Masking for Reducing Indoor Exposure to Simulated Exhaled SARS-Cov-2 Aerosols — United States, 2021
Morbidity and Mortality Weekly Report Efficacy of Portable Air Cleaners and Masking for Reducing Indoor Exposure to Simulated Exhaled SARS-CoV-2 Aerosols — United States, 2021 William G. Lindsley, PhD1; Raymond C. Derk, MS1; Jayme P. Coyle, PhD1; Stephen B. Martin, Jr., PhD2; Kenneth R. Mead, PhD3; Francoise M. Blachere, MS1; Donald H. Beezhold, PhD1; John T. Brooks, MD4; Theresa Boots, MS1; John D. Noti, PhD1 On July 2, 2021, this report was posted as an MMWR Early conference room with a heating, ventilation, and air condition- Release on the MMWR website (https://www.cdc.gov/mmwr). ing (HVAC) system that provided 0.1 m3 per second of air flow SARS-CoV-2, the virus that causes COVID-19, can be (202 ft3 per minute; two air changes per hour) with no air spread by exposure to droplets and aerosols of respiratory fluids recirculation. Two HEPA air cleaners (Honeywell 50250-S, that are released by infected persons when they cough, sing, Kaz Inc.) were used, each rated to provide 250 ft3 per minute talk, or exhale. To reduce indoor transmission of SARS-CoV-2 (0.12 m3 per second) of air filtration for a combined total of between persons, CDC recommends measures including 5.2 air changes per hour. The two air cleaners were used in four physical distancing, universal masking (the use of face masks different locations: 1) center of the room on the floor behind in public places by everyone who is not fully vaccinated), and the source simulator; 2) left and right sides of the room on the increased room ventilation (1). -

Cabin Air Quality Brief
Briefing paper Cabin air quality – Risk of communicable diseases transmission The overall risk of contracting a disease from an ill person onboard an airplane is similar to that in other confined areas with high occupant density, such as a bus, a subway, or movie theatre for a similar time of exposure. anywhere where a person is in close contact with others. That said, the risk on airplanes is probably lower than in many confined spaces because modern airplanes have cabin air filtration systems equipped with HEPA filters. HEPA or high efficiency particulate air filters have similar performance to those used to keep the air clean in hospital operating rooms and industrial clean rooms. These filters are very effective at trapping microscopic particles as small as bacteria and viruses. HEPA filters are effective at capturing greater than 99 percent of the airborne microbes in the filtered air. Filtered, recirculated air provides higher cabin humidity levels and lower particulate levels than 100% outside air systems. The cabin air system is designed to operate most efficiently by delivering approximately 50 percent outside air and 50 percent filtered, recirculated air. This normally provides between 15 to 20 cubic feet of total air supply per minute per person in economy class. The total air supply is essentially sterile and particle-free. Cabin air circulation is continuous. Air is always flowing into and out of the cabin. Total airflow to the cabin is supplied at a bulk flow rate equivalent to 20 to 30 air changes per hour. This provides temperature control and minimizes temperature gradients within the cabin. -

Premium Wood Fireplaces
PREMIUM WOOD FIREPLACES ALL MODELS 2020 EPA CERTIFIED 1 Reimagine the (HEART)H of Your Home CATALYTIC TECHNOLOGY All Fireplace Xtrordinair™ wood fireplaces use state of the art catalytic technology. This allows our large capacity wood fire- places to produce highly efficient, clean fires in all burn settings. This bulletproof technology achieves roaring fires with super-long burn times and very high BTUs ranges, making it the perfect system for these powerhouse home heaters. CORD WOOD TESTING All of our wood fireplaces are 2020 EPA certified using the new EPA CORD WOOD protocol rather then the CRIB WOOD protocal that most other manufacturers test to. By testing with CORD WOOD you get a true real world measurement of how well the fireplace will burn and perform in your home. The 44 Elite™ is shown with the Classic Arch™ double door face. 2 CHAPTERS 1. Meet the Peak of Wood Fireplace Design Explore the 42 Apex™ & 42 Apex™ Clean Face Page 4 2. 42 Apex™ with Decorative Faces Page 6 3. Powerhouse Heaters, Elegant Style Elite™ Fireplaces are More than just a Name Page 10 4. 36 Elite™ Page 12 5. 44 Elite™ Page 14 6. Custom Shop Faces Page 18 8. How They Work 8. The 42 Apex™ Model 8. Page 20 8. The Elite™ Models Page 21 8. Framing 42 Apex™ Fireplace Framing Page 22 Elite™ Fireplace Framing Page 23 3 CHAPTER 1 __ Meet the Peak of Wood Fireplace Design Explore the 42 Apex™ The 42 Apex™ Wood Fireplace delivers natural convection heat efficiently throughout your home and offer a sleek, rectangular door and viewing area.