Making Sense of Addiction and Its Treatment
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Styles of Secular Recovery
White, W. & Nicolaus, M. (2005). Styles of secular recovery. Counselor, 6(4), 58-61. Styles of Secular Recovery William L. White and Martin Nicolaus The last essay in this column noted the growing diversity in religious, spiritual and secular frameworks of recovery and sketched the history of religious approaches to addiction recovery. This essay reviews the history and growing varieties of secular recovery and the implications of such diversity for the addictions professional. A History of Secular Recovery The history of non-religious, non-spiritual approaches to the resolution of alcohol and other drug problems begins with the Washingtonian Revival of the 1840s. The Washingtonians removed preachers and physicians from the temperance lectern in favor of men and women who, in the vernacular of the day, were “reformed” or were “reforming.” The Washingtonians replaced religious admonitions not to drink with 1) public confession of one’s addiction, 2) a signed pledge of abstinence, 3) visits to younger members, 4) economic assistance to new members, 5) experience sharing meetings, 6) outreach to the suffering drunkard, and 7) sober entertainment and fellowship. While many Washingtonians entered the life of their local churches, Washingtonian leaders were charged by their religious critics with committing the sin of humanism--placing their own will above the power of God. Recovery support societies that followed the Washingtonians took on a more religious orientation, but secular recovery groups continued in some of the mid- century moderation societies, ribbon reform clubs and support societies that grew out of early treatment institutions, e.g. the Ollapod Club and the Keeley Leagues. -

Staying Connected Is Important: Virtual Recovery Resources
STAYING CONNECTED IS IMPORTANT: VIRTUAL RECOVERY RESOURCES • Refuge Recovery: Provides online and virtual INTRODUCTION support In an infectious disease outbreak, when social https://www.refugerecovery.org/home distancing and self-quarantine are needed to • Self-Management and Recovery Training limit and control the spread of the disease, (SMART) Recovery: Offers global community continued social connectedness to maintain of mutual-support groups, forums including a recovery is critically important. Virtual chat room and message board resources can and should be used during this https://www.smartrecovery.org/community/ time. Even after a pandemic, virtual support may still exist and still be necessary. • SoberCity: Offers an online support and recovery community This tip sheet describes resources that can be https://www.soberocity.com/ used to virtually support recovery from mental/ substance use disorders as well as other • Sobergrid: Offers an online platform to help resources. anyone get sober and stay sober https://www.sobergrid.com/ • Soberistas: Provides a women-only VIRTUAL RECOVERY PROGRAMS international online recovery community https://soberistas.com/ • Alcoholics Anonymous: Offers online support • Sober Recovery: Provides an online forum for https://aa-intergroup.org/ those in recovery and their friends and family https://www.soberrecovery.com/forums/ • Cocaine Anonymous: Offers online support and services • We Connect Recovery: Provides daily online https://www.ca-online.org/ recovery groups for those with substance use and -

Women Recovering in Alcoholics Anonymous: the Impact of Social Bonding
UNLV Retrospective Theses & Dissertations 1-1-2003 Women recovering in Alcoholics Anonymous: The impact of social bonding Tina Marie Wininger University of Nevada, Las Vegas Follow this and additional works at: https://digitalscholarship.unlv.edu/rtds Repository Citation Wininger, Tina Marie, "Women recovering in Alcoholics Anonymous: The impact of social bonding" (2003). UNLV Retrospective Theses & Dissertations. 1570. http://dx.doi.org/10.25669/s5bx-078s This Thesis is protected by copyright and/or related rights. It has been brought to you by Digital Scholarship@UNLV with permission from the rights-holder(s). You are free to use this Thesis in any way that is permitted by the copyright and related rights legislation that applies to your use. For other uses you need to obtain permission from the rights-holder(s) directly, unless additional rights are indicated by a Creative Commons license in the record and/ or on the work itself. This Thesis has been accepted for inclusion in UNLV Retrospective Theses & Dissertations by an authorized administrator of Digital Scholarship@UNLV. For more information, please contact [email protected]. WOMEN RECOVERING IN ALCOHOLICS ANONYMOUS: THE IMPACT OF SOCIAL BONDING by Tina Marie Wininger Bachelor of Arts University of Nevada, Las Vegas 2000 A thesis submitted in partial fulfillment of the requirements for the Master of Arts Degree in Sociology Department of Sociology College of Liberal Arts Graduate College University of Nevada, Las Vegas August 2003 Reproduced with permission of the copyright owner. Further reproduction prohibited without permission. UMI Number: 1417743 INFORMATION TO USERS The quality of this reproduction is dependent upon the quality of the copy submitted. -

Cognitive Behavioral Therapy for Substance Use Disorders Among Veterans
Cognitive Behavioral Therapy for Substance Use Disorders Among Veterans Therapist Manual Josephine M. DeMarce, Ph.D. Maryann Gnys, Ph.D. Susan D. Raffa, Ph.D. Bradley E. Karlin, Ph.D. Cognitive Behavioral Therapy for Substance Use Disorders Among Veterans Therapist Manual Suggested Citation: DeMarce, J. M., Gnys, M., Raffa, S. D., & Karlin, B. E. (2014). Cognitive Behavioral Therapy for Substance Use Disorders Among Veterans: Therapist Manual. Washington, DC: U.S. Department of Veterans Affairs. Table of Contents Table of Figures ..............................................................................................................................................vii Acknowledgements .......................................................................................................................................... ix Preface ............................................................................................................................................................... x Part 1: Background, Theory, Case Conceptualization, and Treatment Structure ....................1 Introduction ....................................................................................................................................................... 2 What is Cognitive Behavioral Therapy? ........................................................................................................ 2 About the Manual ......................................................................................................................................... -
Maintaining Sobriety How Support Groups Can Help
MAINTAINING SOBRIETY HOW SUPPORT GROUPS CAN HELP Barbara H. Bradford, LICSW March 19, 2014 Overview • What do we know • High cost of substance-related addictive disorders • Role of support groups • Resources What do we know? •More than one-half of American adults have a close family member who has or has had Alcohol Use Disorder (AUD) •The federal government estimates that 8.9 percent of full-time workers have drinking problems •Alcohol costs American business an estimated $134 billion in productivity losses, mostly due to missed work •According to SAMHSA, in 2011, 133.4 million people used alcohol & 22.5 million used illicit drugs. What do we know • 22% of men and 14% of women have some type of substance-related addictive disorder (National Survey on Drug Use and Health 2011) • According to the National Center for Health Statistics – there were 38,329 overdose deaths in the US in 2010. 57.7% of those involved pharmaceuticals, 74.3% were unintentional Support group history • Native Americans • Washingtonians • Oxford Groups • Alcoholics Anonymous • Post AA alternatives Alcoholics Anonymous • 1935 “Dr. Bob & Bill W” • Primary features – Admit to having problem with alcohol – Acknowledge role of “Higher Power” – Sharing experience in meeting settings – Peer mentoring (sponsorship) 2.1 million members in 150 countries Strong on line presence with e-groups available Narcotics Anonymous • 1953 NA began in California • AA endorsed NA to make use of AA 12 Steps/traditions • 1970’s time of rapid growth from 20 meetings nationally to 1100 meetings -

HOW to FIND a RECOVERY GROUP: MUTUAL HELP IS MORE THAN SELF-HELP William Doverspike, Ph.D
HOW TO FIND A RECOVERY GROUP: MUTUAL HELP IS MORE THAN SELF-HELP William Doverspike, Ph.D. Drdoverspike.com 770-913-0506 One of the most common statements heard in alcohol problems. A promising strategy mutual-support recovery groups is the involves assigning a person to alternative following: “I don’t need a self-help group. If I treatments based on specific needs and could have done it alone, I wouldn’t have characteristics of the individual. needed you.” Traditional Recovery Groups Beginning with Alcoholics Anonymous (AA), In addition to AA, there are also recovery which celebrated its 80th International groups for families and friends of alcoholics Convention of 70,000 sober alcoholics who met (Al-Anon) as well as children of alcoholics at the World Congress Center in Atlanta in July (Alateen). Mutual help recovery groups are also 2015, there are approximately 400 variations of available for those who suffer from narcotics 12 Step programs that have emerged. Two addiction to (Narcotics Anonymous), as well as decades ago, a monumental survey published in families and friends those affected by such Consumer Reports (1995) revealed that AA addiction (Nar-Anon). scored significantly better (251) than mental health professionals such as psychiatrists (226), In the metro Atlanta area, there are hundreds of social workers (225), psychologists (220), weekly AA and Al-Anon meetings. Many of family physicians (213) and marriage these meetings are held in churches and counselors (208). Although this survey was not synagogues, although AA and Al-Anon is not a scientific study, the readers of Consumer affiliated with any sect, religion, sect, Reports highlighted the popularity of mutual denomination, political entity, organization, or help recovery groups. -

COVID-19 and Mental Health Resources: Substance Use Recovery1
COVID-19 and Mental Health Resources: Substance Use Recovery1 For more fact sheets in this series, visit Pacific Southwest Mental Health Technology Transfer Center (PS MHTTC) COVID-19 and Mental Health Resources. For resources and virtual events from across the MHTTC Network, visit Responding to COVID-19. SAMHSA Resources • Addiction Technology Transfer Centers (ATTC) Network Resources on addiction for behavioral health providers, including in the Pacific Southwest region. • Coronavirus (COVID-19) Continually updated page of guidelines and resources from SAMHSA. Addresses topics for clinicians and providers such as managing patients’ withdrawal, opioid treatment programs and quarantine, and telemedicine for medication-assisted treatment. Resources for Those in Recovery (not peer-/community-based) • Virtual Recovery Resources Resource list from SAMHSA. • SMART (Self-Management and Recovery Training) Science-based tools and mutual support meetings for those in recovery and their loved ones. Also offers an online forum. • Recovery Speakers Inspirational and supportive recordings of speakers from different 12-step fellowships. 12 Step Meetings • 12-Step.org Online meeting calendar at various recovery-related websites. • Online Intergroup of Alcoholics Anonymous Portal to hundreds of online AA meetings happening worldwide, including groups in Spanish and other languages and groups for specific populations (women, young people, LGBTQ, secular, etc.). 1 Note: resources do not necessarily reflect the opinions of the Pacific Southwest Mental Health Technology Transfer Center or SAMHSA. Inclusion on this list does not imply endorsement. • Virtual NA: Virtual Meetings Searchable databases of online and phone-based Narcotics Anonymous meetings in multiple languages, including ASL. Select the “Formats” drop-down menu to find online or phone meetings specifically. -

Women in Alcoholics Anonymous: a Qualitative Research Study Ariel Larson
Duquesne University Duquesne Scholarship Collection Electronic Theses and Dissertations Summer 2015 Women In Alcoholics Anonymous: A Qualitative Research Study Ariel Larson Follow this and additional works at: https://dsc.duq.edu/etd Recommended Citation Larson, A. (2015). Women In Alcoholics Anonymous: A Qualitative Research Study (Doctoral dissertation, Duquesne University). Retrieved from https://dsc.duq.edu/etd/799 This Immediate Access is brought to you for free and open access by Duquesne Scholarship Collection. It has been accepted for inclusion in Electronic Theses and Dissertations by an authorized administrator of Duquesne Scholarship Collection. For more information, please contact [email protected]. WOMEN IN ALCOHOLICS ANONYMOUS: A QUALITATIVE RESEARCH STUDY A Dissertation Submitted to the McAnulty College and Graduate School of Liberal Arts Duquesne University In partial fulfillment of the requirements for the degree of Doctor of Philosophy By Ariel Larson May 2015 Copyright by Ariel Larson 2015 WOMEN IN ALCOHOLICS ANONYMOUS: A QUALITATIVE RESEARCH STUDY By Ariel Larson Approved May 1, 2015 ________________________________ ________________________________ Russell Walsh, Ph.D. Jessie Goicoechea, Ph.D. Professor of Psychology Assistant Professor of Psychology (Committee Chair) (Committee Member) ________________________________ Michael Flaherty, Ph.D. Guest Reader (Committee Member) ________________________________ ________________________________ James Swindal, Ph.D. Leswin Laubscher, Ph.D. Dean, McAnulty College Chair, Psychology Department Professor of Psychology iii ABSTRACT WOMEN IN ALCOHOLICS ANONYMOUS: A QUALITATIVE RESEARCH STUDY By Ariel Larson August 2015 Dissertation supervised by Russ Walsh, PhD This research looks at how women in particular navigate the complicated power dynamics of twelve-step programs, specifically AA, to achieve long-term sobriety. This study attempts to understand how women in AA are appropriating and shaping AA and its reliance on the twelve-steps in unique and resourceful ways to make recovery their own. -

AA Alternative Support Groups
AA Alternative Support Groups Secular Organizations for Sobriety (also known as Save Our Selves): Meetings are for people suffering from either alcoholism or drug addiction. SOS encourages the use of science and reason to further develop insight into the nature of one's own drug addiction, rather than spiritual principles or God. They believe that support is critical to helping individuals achieve and maintain sobriety, SOS credits the individual for achieving and maintaining his or her own sobriety, without reliance on any "Higher Power". SOS respects recovery in any form regardless of the path by which it is achieved. It is not opposed to or in competition with any other recovery programs. 4th Floor-Follow Signs The Titus Building Alec Tuesday 7:00 PM Edina 6550 York Ave So 612-405-8000 Mills Church Eric Friday 7:30 PM Minnetonka 13215 Minnetonka Dr 952-222-7697 Health Realization: Health Realization (HR) meetings are for people suffering from either alcoholism or drug addiction. HR focuses on developing the individual's personal capacity to overcome his or her drug or alcohol problem. HR meetings aim to empower such people through teaching conscious awareness of three principles: (1) Mind, (2) Consciousness, and (3) Thought. The goal is for the individual to gain control over their problem by integrating and practicing these three principles in their daily life. Conceptual Counseling 651-221-0334 Monday 5:00 PM St. Paul 287 E. 6th Street - Suite 300 Canvas Health Bruce Monday 7:00 PM Hope House Stillwater 375 East Orleans 651-436-7777 Recovery Church Meg Monday 7:00 PM Steps Room St. -

Alcoholics Anonymous: Come for Sobriety 11
ALCOHOLICS ANONYMOUS: COME FOR SOBRIETY 11 Alcoholics Anonymous: Come for Sobriety and Stay for the Fellowship Gary A. Cretser Behavioral Sciences William K. Lombardo Behavioral Sciences Heather Dickerson Behavioral Sciences Dorene Doherty Behavioral Sciences Matt Olson Behavioral Sciences Michelle Peñaflor Behavioral Sciences An open-ended questionnaire regarding various aspects of the mutual-help program of Alcoholics Anonymous (AA) was administered to a sample of 25 AA members. The questionnaire was designed to examine which elements of the AA program members considered most important in helping them overcome problems with alcohol. The data were also analyzed to determine which program element(s) were most responsible for maintaining membership in the organization. Our typical sample member was in their 30’s, a member of AA for at least 5 years, attended between 8 and 15 meetings a month, and became involved with AA through an order of the court or hospitalization. Our primary findings were that the spiritual, affiliative, and cognitive aspects were perceived as being most important. Although for most of the members surveyed, the entire program (i.e. the twelve steps, ‘Big Book,’ meetings and sponsor etc.) was perceived as critical in making it possible for them to overcome alcohol problems. Some evidence was found for the importance of ‘fellowship,’ broadly defined, in terms of the retention of members. The relation of these findings to earlier work on AA and 12-Step groups in general is discussed. Introduction Many people are committed members of Alcoholics Anonymous and fervently believe in the power of this 12-Step program to help them overcome alcohol dependency. -
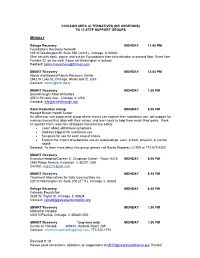
Chicago Area Additions/Alternatives to 12 Step
CHICAGO AREA ALTERNATIVES (OR ADDITIONS) TO 12 STEP SUPPORT GROUPS MONDAY Refuge Recovery MONDAY 12:00 PM Foundations Recovery Network 225 W Washington St. Suite 550 (2nd fl.), Chicago, IL 60603 (See security desk, sign in and ask for Foundations then take elevator to second floor. Enter from Franklin St. on the west if door on Washington is locked). Contact: [email protected] SMART Recovery MONDAY 12:00 PM Above and Beyond Family Recovery Center 2942 W Lake St.,Chicago, Illinois 60612, USA Contact: [email protected] SMART Recovery MONDAY 1:00 PM Breakthrough Urban Ministries 402 N St Louis Ave., Chicago, IL USA Contact: [email protected] Harm Reduction Group MONDAY 6:00 PM Howard Brown Health Center An affirming, non-judgmental group where clients can explore their substance use, get support for making choices that align with their values, and learn tools to help them reach their goals. Work on specific harm reduction strategies that prioritize safety Learn about withdrawal symptoms Address triggers for substance use Set goals for use for each drug of choice Explore the impact of substance use on relationships, work, school, physical, & mental health Contact: To learn more about this group, please call Sonila Sejdaras, LCSW at 773.572.8353 SMART Recovery Evanston Hospital/Doreen E. Chapman Center - Room 5415 MONDAY 6:00 PM 2650 Ridge Avenue, Evanston, IL 60201 USA Contact: [email protected] SMART Recovery MONDAY 6:15 PM Treatment Alternatives for Safe Communities Inc. 225 W Washington St. Suite 200 (2nd fl.), Chicago, IL 60603 Refuge Recovery MONDAY 6:30 PM Gateway Foundation 3828 W. -

Global Recognition
SMART RECOVERY SPOTLIGHT GLOBAL RECOGNITION U.S. GOVERNMENT AGENCIES AND PROFESSIONAL ORGANIZATIONS NATIONAL INSTITUTE ON DRUG ABUSE group could be helpful (e.g., going to SMART Recovery 3 Understanding Drug Abuse and Addiction: instead of AA …). What Science Says — Self-Help and Drug NIH funded CheckUp & Choices (www.smartrecovery. Addiction Treatment org/checkupandchoices), an evidence-based web Self-help groups can complement and extend the app based on SMART’s 4-Point Program that helps effects of professional drug addiction treatment. people stop drinking, which was developed under The most prominent groups are those affiliated with the leadership of Reid Hester, Ph.D. After NIAAA- Alcoholics Anonymous (AA), Narcotics Anonymous (NA), funded research proved its effectiveness, new apps and … SMART Recovery. Most drug addiction treatment were developed for opioids, stimulants, marijuana and programs encourage patients to participate in a self- compulsive gambling. help group during and after formal treatment.1 SMART’s InsideOut program for correctional facilities NIAAA ALCOHOL TREATMENT NAVIGATOR was funded by $1 million in NIDA Small Business Caretaker Support Resources Innovation Research Grants. SMART offers the court- Just as the needs of each person with alcohol use mandated nonreligious recovery support that meets disorder are different, each family’s needs are also the best practice standards set by the National different. Several resources are available to help you Association of Drug Court Professionals (NADCP). while your loved one is in treatment, and afterwards. Major research has established that the program significantly reduces reconviction rates.2 • Family therapy—often offered as part of a patient’s treatment. If not—or if you need additional or continuing support—you can use the Navigator’s NATIONAL INSTITUTE ON ALCOHOL ABUSE search guides to find a licensed addiction therapist AND ALCOHOLISM who offers family therapy.