Failure of Initial Antiretroviral Treatment Regimens
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
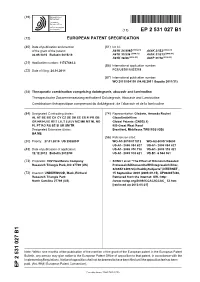
Ep 2531027 B1
(19) TZZ ¥_Z _T (11) EP 2 531 027 B1 (12) EUROPEAN PATENT SPECIFICATION (45) Date of publication and mention (51) Int Cl.: of the grant of the patent: A61K 31/4985 (2006.01) A61K 31/52 (2006.01) 06.05.2015 Bulletin 2015/19 A61K 31/536 (2006.01) A61K 31/513 (2006.01) A61K 38/55 (2006.01) A61P 31/18 (2006.01) (21) Application number: 11737484.3 (86) International application number: (22) Date of filing: 24.01.2011 PCT/US2011/022219 (87) International publication number: WO 2011/094150 (04.08.2011 Gazette 2011/31) (54) Therapeutic combination comprising dolutegravir, abacavir and lamivudine Therapeutische Zusammensetzung enthaltend Dolutegravir, Abacavir und Lamivudine Combinaison thérapeutique comprenant du dolutégravir, de l’abacavir et de la lamivudine (84) Designated Contracting States: (74) Representative: Gladwin, Amanda Rachel AL AT BE BG CH CY CZ DE DK EE ES FI FR GB GlaxoSmithKline GR HR HU IE IS IT LI LT LU LV MC MK MT NL NO Global Patents (CN925.1) PL PT RO RS SE SI SK SM TR 980 Great West Road Designated Extension States: Brentford, Middlesex TW8 9GS (GB) BA ME (56) References cited: (30) Priority: 27.01.2010 US 298589 P WO-A1-2010/011812 WO-A2-2009/148600 US-A1- 2006 084 627 US-A1- 2006 084 627 (43) Date of publication of application: US-A1- 2008 076 738 US-A1- 2009 318 421 12.12.2012 Bulletin 2012/50 US-A1- 2009 318 421 US-B1- 6 544 961 (73) Proprietor: VIIV Healthcare Company • SONG1 et al: "The Effect of Ritonavir-Boosted Research Triangle Park, NC 27709 (US) ProteaseInhibitors on the HIV Integrase Inhibitor, S/GSK1349572,in Healthy Subjects", INTERNET , (72) Inventor: UNDERWOOD, Mark, Richard 15 September 2009 (2009-09-15), XP002697436, Research Triangle Park Retrieved from the Internet: URL:http: North Carolina 27709 (US) //www.natap.org/2009/ICCAC/ICCAC_ 52.htm [retrieved on 2013-05-21] Note: Within nine months of the publication of the mention of the grant of the European patent in the European Patent Bulletin, any person may give notice to the European Patent Office of opposition to that patent, in accordance with the Implementing Regulations. -

( 12 ) United States Patent
US010426780B2 (12 ) United States Patent (10 ) Patent No. : US 10 ,426 , 780 B2 Underwood (45 ) Date of Patent : Oct . 1 , 2019 ( 54 ) ANTIVIRAL THERAPY 5 ,089 , 500 A 2 / 1992 Daluge 5 ,519 ,021 A 5 / 1996 Young et al. 5 ,641 , 889 A 6 / 1997 Daluge et al . (71 ) Applicant : VIIV HEALTHCARE COMPANY , 5 ,663 , 169 A 9 /1997 Young et al. Wilmington , DE (US ) 5 ,663 , 320 A 9 / 1997 Mansour et al. 5 ,693 ,787 A 12 / 1997 Mansour et al. (72 ) Inventor : Mark Richard Underwood , Research 5 ,696 ,254 A 12 / 1997 Mansour et al. Triangle Park , NC (US ) 5 , 808 , 147 A 9 / 1998 Daluge et al. 5 ,811 , 423 A 9 / 1998 Young et al . 5 , 840 , 990 A 11/ 1998 Daluge et al . ( 73 ) Assignee : ViiV Healthcare Company , 5 , 849 , 911 A 12 / 1998 Fassler et al. Wilmington , DE (US ) 5 , 905 , 082 A 5 / 1999 Roberts et al. 5 , 914 , 332 A 6 / 1999 Sham et al . ( * ) Notice : Subject to any disclaimer , the term of this 5 ,917 ,041 A 6 / 1999 Daluge et al. patent is extended or adjusted under 35 5 ,917 , 042 A 6 / 1999 Daluge et al . 5 ,919 ,941 A 7 / 1999 Daluge et al. U . S . C . 154 (b ) by 0 days. 5 , 922 ,695 A 7 / 1999 Arimilli et al. 5 , 935 , 94 A 8 / 1999 Munger et al . (21 ) Appl. No. : 15 / 366 , 442 5 ,977 ,089 A 11/ 1999 Arimilli et al . 6 ,043 ,230 A 3 / 2000 Arimilli et al . ( 22 ) Filed : Dec . -

Lamivudine in Combination with Zidovudine, Stavudine, Or Didanosine in Patients with HIV-1 Infection
Lamivudine in combination with zidovudine, stavudine, or didanosine in patients with HIV-1 infection. A randomized, double-blind, placebo-controlled trial Daniel R. Kuritzkes*, Ian Marschner†, Victoria A. Johnson‡, Roland Bassett†, Joseph J. Eron§, Margaret A. FischlII, Robert L. Murphy¶, Kenneth Fife**, Janine Maenza††, Mary E. Rosandich*, Dawn Bell‡‡, Ken Wood§§, Jean-Pierre Sommadossi‡, Carla PettinelliII II and the National Institute of Allergy and Infectious Disease AIDS Clinical Trials Group Protocol 306 Investigators Objective: To study the antiviral activity of lamivudine (3TC) plus zidovudine (ZDV), didanosine (ddI), or stavudine (d4T). Design: Randomized, placebo-controlled, partially double-blinded multicenter study. Setting: Adult AIDS Clinical Trials Units. Patients: Treatment-naive HIV-infected adults with 200–600 × 106 CD4 T lymphocytes/l. Interventions: Patients were openly randomized to a d4T or a ddI limb, then randomized in a blinded manner to receive: d4T (80 mg/day), d4T plus 3TC (300 mg/day), or ZDV (600 mg/day) plus 3TC, with matching placebos; or ddI (400 mg/day), ddI plus 3TC (300 mg/day), or ZDV (600 mg/day) plus 3TC, with matching placebos. After 24 weeks 3TC was added for patients assigned to the monotherapy arms. Main outcome measure: The reduction in plasma HIV-1 RNA level at weeks 24 and 48. From the *University of Colorado Health Sciences Center and Veterans Affairs Medical Center, Denver, Colorado, the †Center for Biostatistics in AIDS Research, Harvard School of Public Health, Boston, Massachusetts, the -

Recent Advances in Antiviral Therapy J Clin Pathol: First Published As 10.1136/Jcp.52.2.89 on 1 February 1999
J Clin Pathol 1999;52:89–94 89 Recent advances in antiviral therapy J Clin Pathol: first published as 10.1136/jcp.52.2.89 on 1 February 1999. Downloaded from Derek Kinchington Abstract indicated that using a combination of drugs In the early 1980s many institutions in might overcome this problem. The only Britain were seriously considering available drugs during the late 1980s were two whether there was a need for specialist other nucleotide reverse transcriptase inhibi- departments of virology. The arrival of tors (NRTI) which also targeted HIV reverse HIV changed that perception and since transcriptase (HIV-RT): 2',3'-dideoxycytidine then virology and antiviral chemotherapy (ddC) and 2',3'-dideoxyinosine (ddI).56 In have become two very active areas of bio- vitro combination studies gave surprising medical research. Cloning and sequencing results: those viruses that became highly resist- have provided tools to identify viral en- ant to ZDV remained sensitive to both ddC zymes and have brought the day of the and ddI.7 Furthermore, neither cross resistance “designer drug” nearer to reality. At the nor interference between the drugs was an other end of the spectrum of drug discov- issue, and subsequent clinical experience ery, huge numbers of compounds for showed that patients benefited when these two screening can now be generated by combi- compounds were used in combination with natorial chemistry. The impetus to find ZDV.8 It was also found by in vitro studies that drugs eVective against HIV has also virus isolated from patients on long term ZDV stimulated research into novel treatments monotherapy had become insensitive to ZDV, for other virus infections including her- but regained sensitivity when these patients pesvirus, respiratory infections, and were switched to ddI monotherapy. -

AVT-080205-Ait-Khaled
Antiviral Therapy 8:111-120 HIV-1 reverse transcriptase and protease resistance mutations selected during 16–72 weeks of therapy in isolates from antiretroviral therapy-experienced patients receiving abacavir/efavirenz/amprenavir in the CNA2007 study Mounir Ait-Khaled1*, Abdelrahim Rakik2, Philip Griffin2, Chris Stone2, Naomi Richards3, Deborah Thomas4, Judith Falloon5 and Margaret Tisdale2 for the CNA2007 international study team 1GlaxoSmithKline, HIV Clinical Development and Medical Affairs Europe, Greenford, UK 2GlaxoSmithKline, International Clinical Virology, Stevenage, UK 3GlaxoSmithKline, Statistics, Greenford, UK 4GlaxSmithKline, North American Medical Affairs, Research Triangle Park, NC, USA 5National Institute of Allergy and Infectious Diseases, National Institutes of Health, Bethesda, Md., USA *Corresponding author: Tel: +44 208 966 2703; Fax: +44 208 966 4514; E-mail: [email protected] Objective: To determine HIV-1 reverse transcriptase (RT) TAMs were observed, new L74V or I mutations developed and protease (PRO) mutations selected in isolates from in 39 and 16% of isolates, respectively, however, new antiretroviral therapy (ART)-experienced patients receiving M184V mutations were only detected in isolates from two an efavirenz/abacavir/amprenavir salvage regimen. patients, one of whom had added lamivudine + didano- Methods: Open-label, single arm of abacavir, 300 mg sine. M184V was common at baseline (55%) and twice daily, amprenavir, 1200 mg twice daily and maintained in 22/27 (81%) isolates (five of these 22 efavirenz, 600 mg once daily, in ART-experienced added lamivudine or didanosine, or both). The PRO muta- patients of which 42% were non-nucleoside reverse tran- tions selected were in accordance with the distinct scriptase inhibitor-naive. The virology population resistance profile of amprenavir compared with other examined consisted of all patients who took at least 16 protease inhibitors. -

This Project Has Been Supported with Unrestriced Grants from Abbvie Gilead Sciences HEXAL Janssen-Cilag MSD Viiv Healthcare By
This project has been supported with unrestriced grants from AbbVie Gilead Sciences HEXAL Janssen-Cilag MSD ViiV Healthcare By Marcus Altfeld, Hamburg/Boston (USA) Achim Barmeyer, Dortmund Georg Behrens, Hannover Dirk Berzow, Hamburg Christoph Boesecke, Bonn Patrick Braun, Aachen Thomas Buhk, Hamburg Rob Camp, Barcelona (Spain/USA) Rika Draenert, Munich Christian Eggers, Linz (Austria) Stefan Esser, Essen Gerd Fätkenheuer, Cologne Gunar Günther, Windhoek (Namibia) Thomas Harrer, Erlangen Christian Herzmann, Borstel Christian Hoffmann, Hamburg Heinz-August Horst, Kiel Martin Hower, Dortmund Christoph Lange, Borstel Thore Lorenzen, Hamburg Tim Niehues, Krefeld Christian Noah, Hamburg Ramona Pauli, Munich Ansgar Rieke, Koblenz Jürgen Kurt Rockstroh, Bonn Thorsten Rosenkranz, Hamburg Bernhard Schaaf, Dortmund Ulrike Sonnenberg-Schwan, Munich Christoph D. Spinner, Munich Thomas Splettstoesser (Figures), Berlin Matthias Stoll, Hannover Hendrik Streeck, Essen/Boston (USA) Jan Thoden, Freiburg Markus Unnewehr, Dortmund Mechthild Vocks-Hauck, Berlin Jan-Christian Wasmuth, Bonn Michael Weigel, Schweinfurt Thomas Weitzel, Santiago (Chile) Eva Wolf, Munich HIV 2015/16 www.hivbook.com Edited by Christian Hoffmann and Jürgen K. Rockstroh Medizin Fokus Verlag IV Christian Hoffmann, M.D., Ph.D. ICH Stadtmitte (Infektionsmedizinisches Centrum Hamburg) Glockengiesserwall 1 20095 Hamburg, Germany Phone: + 49 40 2800 4200 Fax: + 49 40 2800 42020 [email protected] Jürgen K. Rockstroh, M.D., Ph.D. Department of Medicine I University of Bonn Sigmund-Freud-Strasse 25 53105 Bonn, Germany Phone: + 49 228 287 6558 Fax: + 49 228 287 5034 [email protected] HIV Medicine is an ever-changing field. The editors and authors of HIV 2015/16 have made every effort to provide information that is accurate and complete as of the date of publication. -

Hiv Treatment Failure
HIV TREATMENT FAILURE: A REVIEW OF CURRENT CLINICAL RESEARCH A REPORT FROM THE FORUM FOR COLLABORATIVE HIV RESEARCH JUNE 1998 Acknowledgements This report was written for the Forum for Collaborative HIV Research by Mark Harrington of the Treatment Action Group and Julia Hidalgo, Sc.D, MPH, MSW. The data collection, editing and production processes were coordinated by David Barr. The following people contributed to this report by providing their ideas, their data, and/or their comments during the editing process: Donald Abrams, M.D. - University Of California/San Francisco Ellen Cooper, M.D. Lawrence Deyton, M.D. - Department Of Veteran’s Affairs Linda Distlerath, Ph.D - Merck And Co. Diane Goodwin, PharmD. - Glaxo Wellcome Neil Graham, M.D. - Glaxo-Wellcome Cheryl Karol, Phd. - Hoffman La Roche Deborah Katz , RN- NIAID Division of AIDS Bob Munk, PhD – CPCRA Community Constituency Group Maureen Myers, M.D. - Boeringer Ingleheim Jim Neaton, Ph.D. - University Of Minnesota David Pizzuti, M.D. - Abbott Laboratories Michael Saag, M.D. - University Of Alabama – Birmingham William Freimuth, M.D. – Pharmacia & Upjohn Joy Schmidt – Agouron Pharmaceuticals The following people contributed their time and effort in data collection and the production of this report: Tina Sogocia, MPH - Forum for Collaborative HIV Research William Gist - Forum for Collaborative HIV Research Mike Golde, MPH, JD - Forum for Collaborative HIV Research Deborah Waugh The Forum for Collaborative HIV Research, (FCHR) situated within the Center for Health Policy Research (CHPR) at The George Washington University Medical Center, is an independent public-private partnership composed of representatives from multiple interests in the HIV clinical research arena. -

219 = 141W94 (Amprenavir, Agenerase)
WOMEN=S INTERAGENCY HIV STUDY DRUG LIST 1 B BY ALPHABET 219 = 141W94 (Amprenavir, Agenerase) 147 = Dideoxyinosine ( ddI, Didanosine, Videx, 218 = 1592U89 (Abacavir, Ziagen) Videx EC) 204 = 3-TC (Epivir, Lamivudine) 220 = DMP266 (Efavirenz, Sustiva) 218 = Abacavir (Ziagen, 1592U89) 207 = Droxia (Hydroxyurea, Hydrea) 217 = ABT-378/r (Lopinavir/Ritonavir, Kaletra) 220 = Efavirenz (DMP266, Sustiva) 146 = Acyclovir (Zovirax) 221 = Emivirine (MKC-442, Coactinon) 234 = Adenine Fumarate (Tenofovir disoproxil, bis- 239 = Emtricitabine (Emtriva, Corviracil, FTC) POC PMPA, GS 902, Viread) 239 = Emtriva (emtricitabine, Coviracil, FTC) 224 = Adefovir (Preveon, bis-POM PMPA, GS 233 = ENF (enfuviratide, Fuzeon, T-20) 840) 233 = Enfuviratide (Fuzeon, T-20, ENF) 219 = Agenerase (Amprenavir, 141W94) 204 = Epivir (3-TC, Lamivudine) 098 = AL-721 (by Praxis) (egg lecithin) 254 = Epzicom (abacabir sulfate + lamivudine, 090 = Alpha Interferon Ziagen + Epivir) 101 = Ampligen 210 = Fortovase (Saquinavir, Invirase) 219 = Amprenavir (Agenerase, 141W94) 249 = fosamprenavir (Lexiva) 243 = Atazanavir (Retataz, BMS-232632) 239 = FTC (Emtriva, emtricitabine, Corviracil) 092 = AZT (Retrovir, Zidovudine) 233 = Fuzeon (enfuviratide, T-20, ENF) 122 = Beta Interferon 224 = GS 840 (Adefovir, Preveon, bis-POM 234 = bis-POC PMPA (Tenofovir disoproxil, PMPA) Viread, Adenine Fumarate, GS 902) 234 = GS 902 (Tenofovir disoproxil, bis-POC 224 = bis-POM PMPA (Adefovir, Preveon, GS PMPA, Adenine Fumarate, Viread) 840) 094 = Hivid (ddC, dideoxycytidine, Zalcitabine) 243 = BMS-232632 -

Literature References EMTRICITABINE/RILPIVIRINE
SECTION 2.7 CLINICAL SUMMARY Section 2.7.5 — Literature References EMTRICITABINE/RILPIVIRINE/ TENOFOVIR DISOPROXIL FUMARATE FIXED-DOSE COMBINATION Gilead Sciences International Limited 18 August 2010 CONFIDENTIAL AND PROPRIETARY INFORMATION Emtricitabine/Rilpivirine/Tenofovir Disoproxil Fumarate Section 2.7.5 Literature References Final 2.7. CLINICAL SUMMARY 2.7.5. Literature References 1469 Mulato AS, Cherrington JM. Anti-HIV activity of adefovir (PMEA) and PMPA in combination with antiretroviral compounds: in vitro analyses. Antiviral Res 1997 Nov;36 (2):91-7. 1574 Robbins BL, Srinivas RV, Kim C, Bischofberger N, Fridland A. Anti-human immunodeficiency virus activity and cellular metabolism of a potential prodrug of the acyclic nucleoside phosphonate 9-R-(2-phosphonomethoxypropyl)adenine (PMPA), Bis(isopropyloxymethylcarbonyl) PMPA. Antimicrob Agents Chemother 1998 Mar;42 (3):612-7. 2190 DeGruttola V, Dix L, D'Aquila R, Holder D, Phillips A, Mounir A-K, et al. The relation between baseline HIV drug resistance and response to antiretroviral therapy: re-analysis of retrospective and prospective studies using astandardized data analysis plan. Antivir Ther 2000;5 (1):41-8. 2226 Fischl MA, Richman DD, Hansen N, Collier AC, Carey JT, Pra MF, et al. The safety and efficacy of zidovudine (AZT) in the treatment of subjects with mildy symptomatic human immunodeficiency virus type 1 (HIV) infection. A double- blind, placebo-controlled trial. Ann Intern Med 1990;112 (10):727-37. 2520 Cihlar T, Ho ES, Lin DC, Mulato AS. Human renal organic anion transporter 1 (hOAT1) and its role in the nephrotoxicity of antiviral nucleotide analogs. Nucleosides Nucleotides Nucleic Acids 2001;20 (4-7):641-8. -

Guidelines for Antiretroviral Therapy for HIV Infection
Docket: 1-5462 Initial: JN 15462 February 24/98 CMAJ /Page 496 Customer: CMAJ Feb 24/98 Guidelines for antiretroviral therapy for HIV infection Education Éducation Anita R. Rachlis, MD; Donald P. Zarowny, MD; for the Canadian HIV Trials Network Antiretroviral Working Group* *Members of Canadian HIV Trials Network Antiretroviral Abstract Working Group are listed at the end of the article. Objective: To develop guidelines for health care providers and their HIV-positive patients on the clinical use of antiretroviral agents for HIV infection. This article has been peer reviewed. Options: Recommendations published in 1996 by an international panel. Outcomes: Improvement in clinical outcomes or in surrogate markers of disease CMAJ 1998;158:496-505 activity. Evidence and values: The Canadian HIV Trials Network held a workshop on Oct. 19–20, 1996, to develop Canadian guidelines that incorporate information from recent basic and clinical research. Recommendations: Recommendations for the use of antiretroviral drugs in HIV in- fection are provided for initial therapy, continuing therapy, primary infection, vertical transmission, pediatric therapy and postexposure prophylaxis. Validation: The guidelines are based on consensus of the participants attending the workshop: Canadian investigators, clinicians and invited representatives from the community, government and the pharmaceutical industry. They are subject to review and updating as new information on clinical benefits is published. Sponsors: The workshop was organized by the National Centre of the Canadian HIV Trials Network. Unrestricted educational grants were provided by 8 phar- maceutical companies. Additional support was provided from the National AIDS Strategy of Health Canada. Résumé Objectif : Créer, pour les fournisseurs de soins de santé et leurs patients infectés In this article . -

Longitudinal Analysis of the Utility of Liver Biochemistry in Hospitalised COVID-19 Patients As Prognostic Markers
medRxiv preprint doi: https://doi.org/10.1101/2020.09.15.20194985; this version posted September 18, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity. All rights reserved. No reuse allowed without permission. Longitudinal analysis of the utility of liver biochemistry in hospitalised COVID-19 patients as prognostic markers. Authors: Tingyan Wang1,2*, David A Smith1,3*, Cori Campbell1,2*, Steve Harris1,4, Hizni Salih1, Kinga A Várnai1,3, Kerrie Woods1,3, Theresa Noble1,3, Oliver Freeman1, Zuzana Moysova1,3, Thomas Marjot5, Gwilym J Webb6, Jim Davies1,4, Eleanor Barnes2,3*, Philippa C Matthews3,7*. Affiliations: 1. NIHR Oxford Biomedical Research Centre, Big Data Institute, University of Oxford 2. Nuffield Department of Medicine, University of Oxford 3. Oxford University Hospitals NHS Foundation Trust 4. Department of Computer Science, University of Oxford 5. Oxford Liver Unit, Translational Gastroenterology Unit, John Radcliffe Hospital, Oxford University Hospitals 6. Cambridge Liver Unit, Addenbrooke's Hospital, Cambridge 7. Department of Infectious Diseases and Microbiology, Oxford University Hospitals NHS Foundation Trust *Equal Contributions Corresponding Author: Professor Eleanor Barnes, The Peter Medawar Building for Pathogen Research, South Parks Road, Oxford, OX1 3SY, UK. Telephone: 01865 281547. Email: [email protected] Author Contributions: T.W, D.A.S, C.C., P.C.M and E.B contributed equally to this work. T.W, D.A.S and C.C performed the data analysis and wrote the manuscript and were supervised by E.B, P.C.M and J.D. -

Structural Aspects of Drug Resistance and Inhibition of HIV-1 Reverse Transcriptase
Viruses 2010, 2, 606-638; doi:10.3390/v2020606 OPEN ACCESS viruses ISSN 1999-4915 www.mdpi.com/journal/viruses Review Structural Aspects of Drug Resistance and Inhibition of HIV-1 Reverse Transcriptase Kamalendra Singh, Bruno Marchand, Karen A. Kirby, Eleftherios Michailidis and Stefan G. Sarafianos * Christopher Bond Life Sciences Center & Department of Molecular Microbiology & Immunology, University of Missouri, Columbia, Missouri 65211, USA; E-Mails: [email protected] (K.S.); [email protected] (B.M.); [email protected] (K.A.K.); [email protected] (E.M.) * Author to whom correspondence should be addressed; E-Mail: [email protected]; Tel.: +1-573-882-4338. Received: 2 December 2009; in revised form: 22 January 2010 / Accepted: 3 February 2010 / Published: 11 February 2010 Abstract: HIV-1 Reverse Transcriptase (HIV-1 RT) has been the target of numerous approved anti-AIDS drugs that are key components of Highly Active Anti-Retroviral Therapies (HAART). It remains the target of extensive structural studies that continue unabated for almost twenty years. The crystal structures of wild-type or drug-resistant mutant HIV RTs in the unliganded form or in complex with substrates and/or drugs have offered valuable glimpses into the enzyme’s folding and its interactions with DNA and dNTP substrates, as well as with nucleos(t)ide reverse transcriptase inhibitor (NRTI) and non-nucleoside reverse transcriptase inhibitor (NNRTIs) drugs. These studies have been used to interpret a large body of biochemical results and have paved the way for innovative biochemical experiments designed to elucidate the mechanisms of catalysis and drug inhibition of polymerase and RNase H functions of RT.