Telemedicine and Its Potential for the Future of Healthcare
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

APPROPRIATE HEALTH TECHNOLOGY Emlrc44itech.Disc./1
WORLD HEALTH ORGANIZATION ~egional Office for the Eastern Mediterranean ORGANISATION MONDIALE DE LA SANTE Bureau regional de la Mediterranee orientale REGIONAL COMMITTEE FOR THE EMlRC44/Tech.Disc'/l EASTERN MEDITERRANEAN August 1997 Forty-fourth Session Original: Arabic Agenda item 7 TECHNICAL DISCUSSIONS APPROPRIATE HEALTH TECHNOLOGY EMlRC44ITech.Disc./1 CONTENTS page Executive Summary 1. Introduction....................................................................................................... 1 2. Definitions......................................................................................................... 1 2.1 Health technology..................................................................................... I 2.2 Appropriate technology............................................................................. I 3. Appropriate technology and future trends........................................................... 3 3. I General..................................................................................................... 3 3.2 Health care.................................................................... ............................ 3 3.3 Gene technology..... ....... ....... ............ ........................................................ 4 3.4 Laboratory medicine technologies............................................................. 4 3.5 Transfusion medicine................................................................................. 5 3.6 Diagnostic imaging................................................................................... -

Patient-Monitoring Systems
17 Patient-Monitoring Systems REED M. GARDNER AND M. MICHAEL SHABOT After reading this chapter,1 you should know the answers to these questions: ● What is patient monitoring, and why is it done? ● What are the primary applications of computerized patient-monitoring systems in the intensive-care unit? ● How do computer-based patient monitors aid health professionals in collecting, analyzing, and displaying data? ● What are the advantages of using microprocessors in bedside monitors? ● What are the important issues for collecting high-quality data either automatically or manually in the intensive-care unit? ● Why is integration of data from many sources in the hospital necessary if a computer is to assist in critical-care-management decisions? 17.1 What Is Patient Monitoring? Continuous measurement of patient parameters such as heart rate and rhythm, respira- tory rate, blood pressure, blood-oxygen saturation, and many other parameters have become a common feature of the care of critically ill patients. When accurate and imme- diate decision-making is crucial for effective patient care, electronic monitors frequently are used to collect and display physiological data. Increasingly, such data are collected using non-invasive sensors from less seriously ill patients in a hospital’s medical-surgical units, labor and delivery suites, nursing homes, or patients’ own homes to detect unex- pected life-threatening conditions or to record routine but required data efficiently. We usually think of a patient monitor as something that watches for—and warns against—serious or life-threatening events in patients, critically ill or otherwise. Patient monitoring can be rigorously defined as “repeated or continuous observations or meas- urements of the patient, his or her physiological function, and the function of life sup- port equipment, for the purpose of guiding management decisions, including when to make therapeutic interventions, and assessment of those interventions” (Hudson, 1985, p. -

Dec 3 1 2013
X 133704. DEC 3 1 2013 510(K) Summary for M1 Capnography Mask 1. Submission Sponsor Monitor Mask, Inc. 551543 dAvenue NE Seattle WA, 98105 USA Phone: 877.226.1776 Contact: JW Beard MD, MBA, Founder and CEO 2. Submission Correspondent Emergo, Group, Inc. 816 Congress Avenue, Suite 1400 Austin, TX 78701 office Phone: (512) 327.9997 Fax: (512) 327.9998 Contact: Stuart RGoldman, Senior Consultant, RA/QA Email: oroiect.manapement~emerpogroup.com 3. Date Prepared September 20, 2013 4. Device Identification Trade/Proprietary Name: M1 Capnography Mask Common/Usual Name: oxygen/capnography mask Classification Name: analyzer, gas, carbon-dioxide, gaseous-phase Classification Regulation: §868.1400 Product Code: CCK (primary); BYG (secondary) Device Class: Class 11 Classification Panel: Anesthesiology 5. Legally Marketed Predicate Device CapnoxygenO Mask (K(971229) manufactured by Medlsys (Southmedic) 6. Device Description The M1 Capnography Mask is connected to a gas source for delivering low flow oxygen through flexible tubing to the patient, and at the same time provides a means to attach a capnograph for monitoring exhaled carbon dioxide during nose and mouth breathing. The capnograph gas sample tube attaches to a standard female Luer connector on either the left or right side of the M1 Capnography Mask. The M1 Capnography Mask will initially be made available in only one size, adult large (Model #001). Page 5-1 7. Indication for Use Statement The M1 Capnography Mask is a single-use device intended for delivering supplemental oxygen and monitoring exhaled carbon dioxide in non-intubated spontaneously breathing patients. Standard oxygen tubing and two female Luer ports for gas sample line attachment are included. -

Serious Adverse Event Reporting Under Directives 90/385/Eec and 93/42/Eec
EUROPEAN COMMISSION DG Internal Market, Industry, Entrepreneurship and SMEs Consumer, Environmental and Health Technologies Health technology and Cosmetics MEDDEV 2.7/3 revision 3 May 2015 GUIDELINES ON MEDICAL DEVICES CLINICAL INVESTIGATIONS: SERIOUS ADVERSE EVENT REPORTING UNDER DIRECTIVES 90/385/EEC AND 93/42/EEC. Note The present Guidelines are part of a set of Guidelines relating to questions of application of EC-Directives on medical Devices. They are legally not binding. The Guidelines have been carefully drafted through a process of intensive consultation of the various interested parties (competent authorities, Commission services, industries, other interested parties) during which intermediate drafts where circulated and comments were taken up in the document. Therefore, this document reflects positions taken by representatives of interest parties in the medical devices sector. These guidelines incorporate changes introduced by Directive 2007/47/EC amending Council Directive 90/385/EEC and Council Directive 93/42/EEC. 1 MEDICAL DEVICES DIRECTIVES CLINICAL INVESTIGATION GUIDELINES FOR ADVERSE EVENT REPORTING UNDER DIRECTIVES 90/385/EEC AND 93/42/EEC Index 1. INTRODUCTION 2. SCOPE 3. DEFINITIONS 4. REPORTABLE EVENTS 5. REPORT BY WHOM 6. REPORT TO WHOM 7. REPORTING TIMELINES 8. CAUSALITY ASSESSMENT 9. REPORTING FORM Appendix – Summary Reporting Form 2 1. INTRODUCTION This guidance defines Serious Adverse Event (SAE) reporting modalities and includes a summary tabulation reporting format. Individual reporting should be performed in accordance with national requirements. The objective of this guidance is to contribute to the notification of SAEs to all concerned National Competent Authorities (NCAs ) 1 in the context of clinical investigations in line with the requirements of Annex 7 of Directive 90/385/EEC and Annex X of Directive 93/42/EEC, as amended by Directive 2007/47/EC. -
Medical Device Software Regulation Software Qualification And
AHWP/WG1/R001:2014 REFERENCE DOCUMENT (DRAFT for Public Comments) Title: White Paper on Medical Device Software Regulation – Software Qualification and Classification Author: Work Group 1, Pre-Market Submission and CSDT Date 22 May 2014 Copyright © 2014 by the Asian Harmonization Working Party Table of Contents 1. Introduction ............................................................................................................................. 2 2. Definitions ................................................................................................................................ 2 3. Types of Software that are Regulated as Medical Devices ........................................... 4 4. Forms of Medical Device Software .................................................................................... 4 5. SaMD Medical Device Software Classification Globally .............................................. 6 5.1. International Medical Device Regulatory Forum (IMDRF) .................................... 6 5.1.1. IMDRF qualification criteria .......................................................................................... 6 5.2. Australia TGA ..................................................................................................................... 7 5.2.2. Risk classification of software in TGA ...................................................................... 7 5.3. China .................................................................................................................................... -

Ministry of Medical Services Pharmacy and Poisons Board Kenya
MINISTRY OF MEDICAL SERVICES PHARMACY AND POISONS BOARD KENYA GUIDELINES ON SUBMISSION OF DOCUMENTATION FOR REGISTRATION OF MEDICAL DEVICES FIRST EDITION September, 2011 ACKNOWLEDGEMENTS PREFACE Medical Device Regulation in Kenya will be supervised and directed by Kenya Pharmacy and Poisons Board (PPB). Classification, requirements and evaluation of Medical Devices will be mainly simulation of rules and regulations recognized by the international regulatory benchmarks, which are mainly: a. The Pharmacy and Poisons Act Chapter 244 of 2002 b. Global Harmonization Task Force (GHTF) for Medical Device c. EU Medical Device Directives 93/42/EEC, EU In Vitro Diagnostic Device Directive Ministry of Medical Services Page 2 of 2 Pharmacy and Poisons Board Kenya (IVDD) 98/79/EC and EU Active Implantable Medical Device Directive (AIMDD) 90/385/EEC. d. US FDA (United States Food & Drug Administration) e. Australia TGA (Therapeutics Goods Act) The regulation of medical devices in Kenya is aimed at maintaining balance between ensuring product safety, quality and effectiveness and providing the public with timely access to medical devices and preventing the entrance of unsafe or ineffective devices into the market. SCOPE These guidelines shall apply to medical devices and their accessories. For the purposes of these guidelines, accessories shall be treated as medical devices in their own right. Where a device is intended to administer a medicinal product, that device shall be governed by this guideline, without prejudice to the corresponding regulations for registration of medicinal products for human use set by the PPB. If, however, such a device is placed on the market in such a way that the device and the medicinal product form a single integral product which is intended exclusively for use in the given combination and which is not reusable, that single product shall be governed by corresponding regulations for registration of medicinal products for human use set by the PPB. -

Data Protection on Pharmacovigilance and Medical Device Safety
DATA PROTECTION ON PHARMACOVIGILANCE AND MEDICAL DEVICE SAFETY General Galena Pharma Oy, founded in 1996, is a pharmaceutical company specialising in contract manufacturing and packaging. A significant part of the service includes product development, registration & marketing authorization and post-market surveillance. The wide range of our products comprises human and veterinary medicinal products, medical devices in Classes IIa and IIb, cosmetics, food supplements, animal care products and nutritional supplements. The products we manufacture are sold mainly in pharmacies. Galena Pharma has a legal obligation to monitor the adverse events and the effects of their products in the countries where they are getting sold and carry out a continuous risk-benefit assessment. It is called pharmacovigilance and medical device safety operation. With the help of this system and quality assurance management, Galena Pharma can manage adverse events and protect public health. Thanks to this, the safety of Galena Pharma's products is guaranteed. It is the responsibility of the competent authority to inspect and evaluate the pharmacovigilance and medical device safety activities of the company and validate it. Pharmacovigilance and medical device safety obligate Galena Pharma to process the information of the patient and/or the notifier of the adverse reaction, based on which a person can be directly or indirectly identified. These are personal data whose processing is mandatory for Galena Pharma in order to comply with its pharmacovigilance and medical device safety obligations and report any adverse reactions or events that come to their notice to the competent authorities in a relevant and appropriate manner. This privacy statement describes how personal data gets processed for pharmacovigilance and medical device safety purposes under applicable data protection laws and the obligations set out in the EU Data Protection Regulation (EU 2016/679). -

Strengthening Care Management with Health Information Technology a Learning Guide
Strengthening Care Management with Health Information Technology A Learning Guide Presenting lessons learned by the 17 Beacon Community Awardees of the Office of the National Coordinator for Health Information Technology in the U.S. Department of Health and Human Services July 2013 i The Beacon Community Cooperative Agreement Program demonstrates how health IT investments and Meaningful Use of electronic health records (EHR) advance the vision of patient-centered care, while achieving the three-part aim of better health, better care at lower cost. The Department of Health and Human Services, Office of the National Coordinator for Health IT (ONC) is providing $250 million over three years to 17 selected communities throughout the United States that have already made inroads in the development of secure, private, and accurate systems of EHR adoption and health information exchange. Each of the 17 communities—with its unique population and regional context—is actively pursuing the following areas of focus: • Building and strengthening the health IT infrastructure and exchange capabilities within communities, positioning each community to pursue a new level of sustainable health care quality and efficiency over the coming years; • Translating investments in health IT to measureable improvements in cost, quality and population health; and • Developing innovative approaches to performance measurement, technology and care delivery to accelerate evidence generation for new approaches. For more information about the Beacon Community Program visit www.healthit.gov. This Learning Guide is part of the Beacon Nation project and is funded by the Hawai’i Island Beacon Community, an awardee of ONC Beacon Community Program. The Learning Guide was produced by Booz Allen Hamilton, under a contract with the Hawai’i Island Beacon Community. -

How to Leverage Health Technology to Improve Patient Flow
How to Leverage Health Technology to Improve Patient Flow 3/31/2017 A growing population has led to an increased demand for healthcare services. Concurrently, healthcare reforms and reimbursement requirements necessitate improvements in quality care and patient satisfaction. Healthcare facilities have begun searching for ways in which to handle the influx of patients without sacrificing either quality or the patient experience. How can your facility achieve increased volume and profits while maintaining quality and improving patient satisfaction? This whitepaper addresses how RTLS (Real Time Locating System) technology can be implemented to solve critical issues such as: · Increased capacity · Decreased waiting times · Patient and staff satisfaction · Increased healthcare staff productivity Increased Capacity The aging population in the United States is requiring more healthcare services. As the Baby Boomer population ages, almost twenty percent of the current population living in the United States will reach age 65 or older. This increase in the aging population leads to a significant growth in the number of individuals with chronic conditions. According to the American Hospital Association, the number of Boomers with multiple chronic conditions is continuing to grow and will reach about 37 million adults by 2030.i The prevalence of chronic conditions is also increasing in the United States population as a whole and calls for increased medical services and innovative approaches on how to properly deliver care to this population. Many healthcare delivery systems are utilizing RTLS technology to meet the increased population challenge. The Nor-Lea Medical Clinic in Lovington, New Mexico implemented an RTLS system to handle their growing influx of patients. -
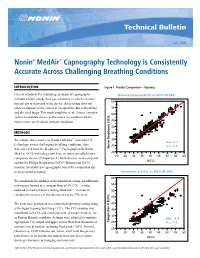
Nonin® Medair™ Capnography Technology Is Consistently Accurate Across Challenging Breathing Conditions
Technical Bulletin July 2009 Nonin® MedAir™ Capnography Technology is Consistently Accurate Across Challenging Breathing Conditions INTRODUCTION Figure 1: Product Comparison – Accuracy Current standards for evaluating accuracy of capnographs NoninNonin RespSense RespSense EtCOEtCO2 vs NICONICO (N-364)(N=364) includes simple, steady flow gas validation in which a known 60 percent gas is delivered to the device. Such testing does not allow evaluation of the effects of complexities due to breathing 55 and diseased lungs. This study sought to create a more complex 2 50 system to evaluate device performance in conditions which better represented realistic patient conditions. 45 40 METHODS 35 Resp EtCO2 To evaluate the accuracy of Nonin’s MedAir™ end-tidal CO 30 2 Bias: 0.2 technology across challenging breathing conditions, data 25 Arms: 2.6 was collected from the RespSense™ Capnograph with Nonin Nonin RespSense EtCO 20 MedAir EtCO2 technology and from an internationally known 20 25 30 35 40 45 50 55 60 competitor device (Competitor A). Both devices were compared ® NICO against the Philips Respironics NICO Mainstream EtCO2 monitor, a mainstream capnograph chosen for comparison due Root Mean Square Error 2.563916 Mean of Response 0.178683 to its accepted accuracy. CompetitorNellcor EtCO A EtCO2 vs2 NICOvs NICO (N=364) (N-364) 60 To compliment the findings of the simulation testing, an additional 55 test was performed at a constant flow of 5% CO2—a value required in medical device testing standards1—in order to 50 validate the accuracy of the devices at a static CO2 level. 2 45 The tests were performed in a controlled laboratory setting using 40 a Michigan Training Test Lung (TTL). -

Biomedical Engineering (BMD ENG) 1
Biomedical Engineering (BMD_ENG) 1 Through the course, students will learn how to apply these experimental BIOMEDICAL ENGINEERING and computational genomics technologies to study gene expression regulation underlying various biological processes, such as oncogenesis. (BMD_ENG) Students will also apply computational and statistical skills, using linux and R/Matlab/Python. BMD_ENG 101-0 Introduction to Biomedical Engineering (0 Unit) BMD_ENG 317-0 Biochemical Sensors (1 Unit) Information to 1) help students determine if BME is the right major Theory, design, and applications of chemical sensors used in medical for them and 2) learn how to make the most of their undergraduate diagnosis and patient monitoring. Electrochemical and optical sensors. experience. The field of biomedical engineering, career and research Prerequisites: BIOL_SCI 215-0; BIOL_SCI 219-0; CHEM 210-1; opportunities, ethics. PHYSICS 135-2; PHYSICS 135-3. BMD_ENG 207-0 BME Lab: Experimental Design (0.5 Unit) A laboratory BMD_ENG 323-0 Visual Engineering Science (1 Unit) course focusing on quantitative physiological measurements Mammalian visual system. Physiological optics. Visual image and analyses, instrument characterization, statistical design of representation and interpretation. Visual adaptation. Motion. Color vision. experiments, and training in preparation and organization of laboratory Prerequisite: PHYSICS 135-2. notes and reports. Prerequisite: BMD_ENG 220-0 or IEMS 303-0 or MECH_ENG 359-0. BMD_ENG 325-0 Introduction to Medical Imaging (1 Unit) Diagnostic X-rays; X-ray film and radiographic image; computed BMD_ENG 220-0 Introduction to Biomedical Statistics (1 Unit) Basic tomography; ultrasound. statistical concepts presented with emphasis on their relevance to Prerequisite: PHYSICS 135-3 or equivalent. biological and medical investigations. -

Executive Brief: Top 10 Health Technology Hazards for 2017
EXECUTIVE BRIEF Top 10 Health Technology Hazards for 2017 A Report from Health Devices November 2016 EXECUTIVE BRIEF Top 10 Health Technology Hazards for 2017 A Report from Health Devices November 2016 Top 10 Health Technology Hazards for 2017 Executive Brief ECRI Institute is providing this abridged version of its 2017 Top 10 list of health technology hazards as a free public service to inform healthcare facilities about important safety issues involving the use of medical devices and systems. The full report— including detailed problem descriptions and ECRI Institute’s step-by-step recommendations for addressing the hazards—is available to members of certain ECRI Institute programs through their membership web pages. The List for 2017 1. Infusion Errors Can Be Deadly If Simple Safety Steps Are Overlooked 2. Inadequate Cleaning of Complex Reusable Instruments Can Lead to Infections 3. Missed Ventilator Alarms Can Lead to Patient Harm 4. Undetected Opioid-Induced Respiratory Depression 5. Infection Risks with Heater-Cooler Devices Used in Cardiothoracic Surgery 6. Software Management Gaps Put Patients, and Patient Data, at Risk 7. Occupational Radiation Hazards in Hybrid ORs 8. Automated Dispensing Cabinet Setup and Use Errors May Cause Medication Mishaps 9. Surgical Stapler Misuse and Malfunctions 10. Device Failures Caused by Cleaning Products and Practices The Purpose of the List The safe use of health technology—from basic infusion pumps to large, complex imaging systems—requires identifying possible sources of danger or difficulty with those technologies and taking steps to minimize the likelihood that adverse events will occur. This list will help healthcare facilities do that.