The 2017 Utah Primary Care Summit 8:30
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Utah's Official Voter Information Pamphlet
UTAH’S OFFICIAL VOTER INFORMATION PAMPHLET 2018 GENERAL ELECTION TUESDAY, NOVEMBER 6TH NOTE: This electronic version of the voter information pamphlet contains general voting information for all Utah voters. To view voting information that is specific to you, visit VOTE.UTAH.GOV, enter your address, and click on “Sample Ballot, Profiles, Issues.” For audio & braille versions of the voter information pamphlet, please visit blindlibrary.utah.gov. STATE OF UTAH OFFICE OF THE LIEUTENANT GOVERNOR SPENCER J. COX LIEUTENANT GOVERNOR Dear Utah Voter, My office is pleased to present the 2018 Voter Information Pamphlet. Please take the time to read through the material to learn more about the upcoming General Election on November 6, 2018. Inside you will find information about candidates, ballot questions, judges, and how to vote. In addition to this pamphlet, you can visit VOTE.UTAH.GOV to find even more information about the election. At VOTE.UTAH.GOV you can view your sample ballot, find your polling location, and view biographies for the candidates in your area. If you need assistance of any kind, please call us at 1-800-995-VOTE, email [email protected], or stop by our office in the State Capitol building. Thank you for doing your part to move our democracy forward. Sincerely, Spencer J. Cox Lieutenant Governor WHAT’S IN THIS PAMPHLET? 1. WHO ARE THE CANDIDATES? 2 U.S. Senate 3 U.S. House of Representatives 5 Utah State Legislature 9 Utah State Board of Education 28 2. WHAT ARE THE QUESTIONS ON MY BALLOT? 30 Constitutional Amendment A 32 Constitutional Amendment B 35 Constitutional Amendment C 39 Nonbinding Opinion Question Number 1 44 Proposition Number 2 45 Proposition Number 3 66 Proposition Number 4 74 3. -

Utah State Board of Education Meeting Minutes
UTAH STATE BOARD OF EDUCATION MEETING MINUTES January 8, 2015 A regular meeting of the Utah State Board of Education was held January 8, 2015 at the Utah State Office of Education, 250 East 500 South, Salt Lake City, Utah. At the direction of the Chair, Vice Chair David Thomas conducted. The meeting convened at 8:30 a.m. Board Members present: Chair David L. Crandall Member Mark Huntsman First Vice Chair David L. Thomas Member Marlin Jensen (non-voting) Second Vice Chair Jennifer Johnson Member Jefferson Moss Member Laura Belnap Member C. Mark Openshaw Member Leslie B. Castle Member R. Dean Rowley (non-voting) Member Freddie Cooper (non-voting) Member Spencer F. Stokes Member Brittney Cummins Member Teresa L. Theurer (non-voting) Member Barbara W. Corry Member Terryl Warner Member Kristin Elinkowski (non-voting) Member Joel Wright Member Linda Hansen Board Members participating by phone: Member Dixie L. Allen Member Steven R. Moore (non-voting) Executive and Board staff present: Brad Smith, State Superintendent Bruce Williams, Associate Supt. Joel Coleman, USDB Superintendent Lorraine Austin, Board Secretary Russ Thelin, USOR Executive Director Emilie Wheeler, Board Communications Sydnee Dickson, Deputy Supt. Specialist Judy Park, Associate Supt. Chris Lacombe, Assistant A.G. Others present: Chris Godfrey, Utah School Employees Association; Lydia Nuttall, parent; Kris Fawson, State Independent Living Council; Vincent Newmeyer; Frank Strickland; Jan Ferré, LCPD; Dessle Olson, UNBC; Rebecca Chavez-Houck, Utah House of Representatives; Rich Nelson, LITC; Blake Wight, Thanksgiving Point; Stephen Ward, Granite School District; Ken O’Brien, Salt Lake City School District. Utah State Board of Education Minutes -2- January 8, 2015 Opening Business Vice Chair David Thomas called the meeting to order at 8:30 a.m. -

Ebay Inc. Non-Federal Contributions: January 1 – December 31, 2018
eBay Inc. Non-Federal Contributions: January 1 – December 31, 2018 Campaign Committee/Organization State Amount Date Utah Republican Senate Campaign Committee UT $ 2,000 1.10.18 Utah House Republican Election Committee UT $ 3,000 1.10.18 The PAC MO $ 5,000 2.20.18 Anthony Rendon for Assembly 2018 CA $ 3,000 3.16.18 Atkins for Senate 2020 CA $ 3,000 3.16.18 Low for Assembly 2018 CA $ 1,000 3.16.18 Pat Bates for Senate 2018 CA $ 1,000 3.16.18 Brian Dahle for Assembly 2018 CA $ 1,000 3.16.18 Friends of John Knotwell UT $ 500 5.24.18 NYS Democratic Senate Campaign Committee NY $ 1,000 6.20.18 New Yorkers for Gianaris NY $ 500 6.20.18 Committee to Elect Terrence Murphy NY $ 500 6.20.18 Friends of Daniel J. O'Donnell NY $ 500 6.20.18 NYS Senate Republican Campaign Committee NY $ 2,000 6.20.18 Clyde Vanel for New York NY $ 500 6.20.18 Ben Allen for State Senate 2018 CA $ 1,000 6.22.18 Steven Bradford for Senate 2020 CA $ 1,000 6.22.18 Mike McGuire for Senate 2018 CA $ 1,000 6.22.18 Stern for Senate 2020 CA $ 1,000 6.22.18 Marc Berman for Assembly 2018 CA $ 1,000 6.22.18 Autumn Burke for Assembly 2018 CA $ 1,000 6.22.18 Ian Calderon for Assembly 2018 CA $ 1,000 6.22.18 Jim Cooper for Assembly 2018 CA $ 1,000 6.22.18 Tim Grayson for Assembly 2018 CA $ 1,000 6.22.18 Blanca Rubio Assembly 2018 CA $ 1,000 6.22.18 Friends of Kathy Byron VA $ 500 6.22.18 Friends of Kirk Cox VA $ 1,000 6.22.18 Kilgore for Delegate VA $ 500 6.22.18 Lindsey for Delegate VA $ 500 6.22.18 McDougle for Virginia VA $ 500 6.22.18 Stanley for Senate VA $ 1,000 6.22.18 Wagner -

Enrolled Copy HB 86 1 SOCIAL SECURITY TAX AMENDMENTS Chief Sponsor
Enrolled Copy H.B. 86 1 SOCIAL SECURITY TAX AMENDMENTS 2 2021 GENERAL SESSION 3 STATE OF UTAH 4 Chief Sponsor: Walt Brooks 5 Senate Sponsor: Wayne A. Harper 6 Cosponsors: Karianne Lisonbee Travis M. Seegmiller 7 Nelson T. Abbott A. Cory Maloy Rex P. Shipp 8 Carl R. Albrecht Kelly B. Miles V. Lowry Snow 9 Stewart E. Barlow Jefferson Moss Robert M. Spendlove 10 Kera Birkeland Merrill F. Nelson Jeffrey D. Stenquist 11 Steve R. Christiansen Val L. Peterson Jordan D. Teuscher 12 James A. Dunnigan Candice B. Pierucci Mike Winder 13 Steve Eliason Susan Pulsipher 14 Craig Hall Adam Robertson 15 Stephen G. Handy Mike Schultz 16 17 LONG TITLE 18 General Description: 19 This bill provides for an individual income tax credit for certain social security benefits. 20 Highlighted Provisions: 21 This bill: 22 < defines terms; 23 < enacts a tax credit for social security benefits that are included in the claimant's 24 federal adjusted gross income; 25 < provides that an individual who claims the tax credit for social security benefits may 26 not also claim the retirement tax credit; 27 < grants rulemaking authority to the State Tax Commission; and 28 < makes technical and conforming changes. H.B. 86 Enrolled Copy 29 Money Appropriated in this Bill: 30 None 31 Other Special Clauses: 32 This bill provides retrospective operation. 33 Utah Code Sections Affected: 34 AMENDS: 35 59-10-1002.2, as last amended by Laws of Utah 2016, Chapter 263 36 59-10-1019, as renumbered and amended by Laws of Utah 2008, Chapter 389 37 ENACTS: 38 59-10-1042, Utah Code Annotated 1953 39 40 Be it enacted by the Legislature of the state of Utah: 41 Section 1. -

April 2017 Newsletter
1 April 2017 Volume 42 Issue 4 THE UTAH TAXPAYER A Publication of the Utah Taxpayers Association If Congress Acts, What Will APRIL 2017 Volume 42 Federal Tax Reform Look Like? With Congress’s failure to repeal and replace the Affordable If Congress Acts, What Will Care Act, attention in Washington, D.C. appears to be turning Federal Tax Reform Look towards federal tax reform. This is a needed change as the Like? Page 1 United States has not seen any comprehensive tax reform since My Corner: Employed by 1986. The nation’s economy has evolved since the 1980’s and Page 2 Utah’s Tax Watchdog for 40 the tax code needs to be reformed to match the economic Years activity of today’s world. Page 2 Currently the federal tax code imposes high marginal rates on 2017 Legislative Session: A both businesses and individuals. According to the Washington, Page 4 D.C. based Tax Foundation, the United States has one of the Mixed Bag of Success, Tax Increases Page 5 highest corporate income tax rates in the world. Significant tax reform would be targeted at lowering those rates. The struggle 2017 Legislative Scorecard for the reform will be how to do it such that it best benefits the Released, 34 “Friend of the United States overall. Taxpayer” Awarded Page 7 The U.S. tax system is complex. The Tax Foundation has stated that individuals spent 8.9 billion hours complying with Utah’s Income Tax Rate the Internal Revenue Tax Code in 2016 and figures that the Ranks Second Highest total cost for tax compliance in 2016 was $409 billion. -

Utah DRAFT State Profile and Data Sheet
8/03/2015 Utah DRAFT State Profile and Data Sheet Utah Demographic Information: Total Population: 2.94 million Growth Rate (since 2001): 1.2% Largest Populated Counties: Salt Lake 1,029,655 Utah 516,564 Davis 306,479 Weber 231,236 Square Miles: 82,169 College Degree (Bachelors or higher): 30.3% Economic Indicators: Total Civilian Labor Force: 1.4 million Current Unemployment: 3.8% State GDP (nominal): 141 billion (2014) Latest GDP Growth Estimate: 5.02% % of U.S. GDP: .84% GDP Per Capita: $48,580 Income Per Capita: $28,184 Utah CMAQ Funding: EPA Non-Attainment Counties: $ 10,750,409 Utah Political Landscape: State Governor: Gary Herbert (R) Committees of Note: Majority Leader—Senate: Ralph Okerlund (R) Natural Resources, Agriculture, Majority Leader—House: Jim Dunnigan (R) and Environment: Senate President: Wayne L. Niederhauser (R) Lee B. Perry (R), Chair H Scott K. Jenkins (R), Chair S House Speaker: Greg Hughes (R) Transportation: U.S. Senators: Johnny Anderson (R), Chair H Alvin B. Jackson (R), Chair S Orrin Hatch (R) Mike Lee (R) Natural Resources, Agriculture, U.S. Representatives by District: and Environmental Quality Rob Bishop (R) - 1st Jason Chaffetz (R) - 3rd Appropriations Subcommittee: Chris Stewart (R) - 2nd Mia Love (R) - 4th David P. Hinkins (R), S Utah Department of Transportation: Mike K. McKell (R), H Executive Director : Regional Directors: Carlos Braceras Kris Peterson Nathan Lee Teri Newell Rick Torgerson Deputy Director: (Northern Utah and (Central Utah) (Southern Wasatch (Central and Northern Wasatch Front) Front and Uintah Basin) Southern Utah) Shane Marshall Utah Legislative Landscape: Utah could have the first commercial oil sands mine in the 14 AFV Bills Proposed in 2015—5 bills enacted: United States by year’s end. -

DRAFT MINUTES SENATE HEALTH and HUMAN SERVICES STANDING COMMITTEE Tuesday, February 18, 2020|8:00 A.M.|250 State Capitol
DRAFT MINUTES SENATE HEALTH AND HUMAN SERVICES STANDING COMMITTEE Tuesday, February 18, 2020|8:00 a.m.|250 State Capitol Members Present: Sen. Evan J. Vickers Sen. Ronald Winterton, Chair Sen. David G. Buxton Members Absent: Sen. Allen M. Christensen President J. Stuart Adams Sen. Luz Escamilla Sen. Jani Iwamoto Staff Present: Sen. Scott D. Sandall Karin M. Rueff, Policy Analyst Annette Sion, Committee Secretary Note: A copy of related materials and an audio recording of the meeting can be found at www.le.utah.gov. Chair Winterton called the meeting to order at 8:01 a.m. MOTION: Sen. Buxton moved to approve the minutes from February 12, 2020. The motion passed with a vote of 6 - 0 - 2. Yeas-6 Nays-0 Absent-2 Sen. D. Buxton Sen. J. Adams Sen. A. Christensen Sen. J. Iwamoto Sen. L. Escamilla Sen. S. Sandall Sen. E. Vickers Sen. R. Winterton 1 . S.B. 121 Medical Cannabis Amendments (Vickers, E.) Sen. Vickers presented the bill with the assistance of Mr. Rich Oborn, Director, Center for Medical Cannabis, Utah Department of Health. SB 121 Cannabis Amendments 1st Substitute SB 121 MOTION: Sen. Vickers moved to replace S.B. 121 with 1st Substitute S.B. 121. The motion passed with a vote of 6 - 0 - 2. Yeas-6 Nays-0 Absent-2 Sen. D. Buxton Sen. J. Adams Sen. A. Christensen Sen. J. Iwamoto Sen. L. Escamilla Sen. S. Sandall Sen. E. Vickers Sen. R. Winterton Spencer Hadley, lobbyist, Utah Therapeutic Health Center, spoke for the bill. Nathan Kazerian, on behalf of spouse, spoke against the bill. -

House of Representatives State of Utah UTAH STATE CAPITOL COMPLEX • 350 STATE CAPITOL P.O
House of Representatives State of Utah UTAH STATE CAPITOL COMPLEX • 350 STATE CAPITOL P.O. BOX 145030 • SALT LAKE CITY, UTAH 84114-5030 • (801)538-1029 AGENDA TO: Members of the House Revenue and Taxation Standing Committee FROM: Rep. Ryan D. Wilcox, Chair Rep. Jim Nielson, Vice Chair RE: Committee Meeting DATE: Wednesday, February 5, 2014 TIME: 4:00 PM PLACE: 445 State Capitol - Call to order and approval of minutes - The following bills are scheduled for consideration: 1. HB0084 School District Amendments (C. Hall) (aos/ccs) 2. HB0273 Property Tax Residential Exemption Amendments (V. Snow) (rlr/lge) COMMITTEE MEMBERS Rep. Ryan D. Wilcox, Chair Rep. Jim Nielson, Vice Chair Rep. Jacob L. Anderegg Rep. Joel K. Briscoe Rep. Melvin R. Brown Rep. Tim M. Cosgrove Rep. Steve Eliason Rep. Gage Froerer Rep. Francis D. Gibson Rep. Eric K. Hutchings Rep. Brian S. King Rep. John Knotwell Rep. Kay L. McIff Rep. Douglas V. Sagers Rep. Jon E. Stanard Rep. Earl D. Tanner Committee Analyst: Leif G. Elder, Office of Legislative Research and General Counsel Committee Secretary: An Bradshaw In compliance with the Americans with Disabilities Act, persons needing auxiliary communicative aids and services for this meeting should call the Office of Legislative Research and General Counsel at 801-538-1032 or use Relay Utah (toll-free in-state 7-1-1 or Spanish language 888-346-3162), giving at least 48 hours notice or the best notice practicable. Every effort will be made to accommodate requests for aids and services for effective communication during the annual General Session. However, given the unpredictable and fast-paced nature of the legislative process, it is essential that you notify us as soon as possible. -

2017 UTAH LEGISLATIVE SCORECARD 1 TABLE of CONTENTS DEAR History of AFP-UT’S Legislative Scorecard
2017 UTAH LEGISLATIVE SCORECARD 1 TABLE OF CONTENTS DEAR History of AFP-UT’s Legislative Scorecard.................2 Grading Methodology..........................................................2 CONCERNED What is Economic Freedom..............................................2 Champions of Prosperity....................................................3 CITIZEN Prosperity Elevated..............................................................3 , House of Representatives Scores: Summary.........4-5 Senate Scores: Summary....................................................6 Anti/Pro Economic Freedom Bills Explained........7-11 Evelyn Everton 2017 House & Senate Grades: Detailed..................12-17 Utah State Director Stories from the Field.....................................................5-17 Thank you for taking the time to learn more about Americans for Prosperity- Utah and our Prosperity Elevated Legislative Agenda. Our mission is to hold elected officials accountable and stand up to the business-as-usual political class. We’re committed, through our Legislative Scorecard to show you how your legislators vote in key policy areas. We’ve built an aggressive policy platform through our Prosperity Elevated initiative, which we’ll go into further detail within. Through the intense effort by our policy team to assemble this comprehensive analysis, you will be able to clearly see which lawmakers are being good stewards of your tax dollars, what reforms passed or failed during the 2017 legislative session, and how those outcomes affect you, your family, and your business. The 2017 Legislative Scorecard is a diligent effort by the Americans for Prosperity-Utah staff to share with you more about the policies we are fighting, but also an opportunity for us to share with you some of the personal stories that make up our team of staff and volunteers from across the state and that work tirelessly to continue to grow this movement for economic freedom. -
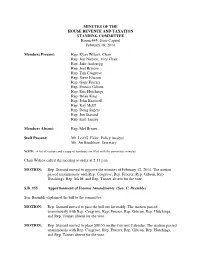
Minutes for 02/18
MINUTES OF THE HOUSE REVENUE AND TAXATION STANDING COMMITTEE Room 445, State Capitol February 18, 2014 Members Present: Rep. Ryan Wilcox, Chair Rep. Jim Nielson, Vice Chair Rep. Jake Anderegg Rep. Joel Briscoe Rep. Tim Cosgrove Rep. Steve Eliason Rep. Gage Froerer Rep. Francis Gibson Rep. Eric Hutchings Rep. Brian King Rep. John Knotwell Rep. Kay McIff Rep. Doug Sagers Rep. Jon Stanard Rep. Earl Tanner Members Absent: Rep. Mel Brown Staff Present: Mr. Leif G. Elder, Policy Analyst Ms. An Bradshaw, Secretary NOTE: A list of visitors and a copy of handouts are filed with the committee minutes. Chair Wilcox called the meeting to order at 2:11 p.m. MOTION: Rep. Stanard moved to approve the minutes of February 12, 2014. The motion passed unanimously with Rep. Cosgrove, Rep. Froerer, Rep. Gibson, Rep. Hutchings, Rep. McIff, and Rep. Tanner absent for the vote. S.B. 155 Apportionment of Income Amendments (Sen. C. Bramble) Sen. Bramble explained the bill to the committee. MOTION: Rep. Stanard moved to pass the bill out favorably. The motion passed unanimously with Rep. Cosgrove, Rep. Froerer, Rep. Gibson, Rep. Hutchings, and Rep. Tanner absent for the vote. MOTION: Rep. Stanard moved to place SB155 on the Consent Calendar. The motion passed unanimously with Rep. Cosgrove, Rep. Froerer, Rep. Gibson, Rep. Hutchings, and Rep. Tanner absent for the vote. House Revenue and Taxation Standing Committee February 18, 2014 Page 2 H.B. 77 Tax Credit for Home-schooling Parent (Rep. D. Lifferth) Rep. Lifferth explained the bill to the committee. Spoke for the bill: Hannah DeForest, citizen Elaine Augustine, citizen Connor Boyack, Libertas Institute Spoke against the bill: Deon Turley, Utah Parent Teacher Association Mark Mickelsen, Utah Education Association MOTION: Rep. -

REPORT on the 2016 UTAH LEGISLATIVE SESSION the 2016 Legislative Session Was Excellent for the University of Utah. Thanks To
REPORT ON THE 2016 UTAH LEGISLATIVE SESSION The 2016 Legislative Session was excellent for the University of Utah. Thanks to President Pershing’s outstanding leadership and the positive outreach of our university advocates, we were able to secure a two-percent performance-based compensation increase plus the additional cost of benefits for faculty and staff. Additionally, we are pleased to report the University received approval to commence the planning and design of the Medical Education and Discovery Complex. SUCCESSES FOR THE UNIVERSITY OF UTAH Ø 2% performance-based compensation increase plus an appropriation for the increased cost in benefits Ø Intent language to allow the University to begin planning and design for the Medical Education and Discovery/Rehabilitation Hospital Ø Approval to bond up to $50M to construct the David Eccles School of Business Executive Education Building Ø $8.8M in one-time funding for the Regents Scholarship program Ø $5M in one-time funding for Performance Based Funding of which will be distributed by formula to all institutions of higher education Ø $5M in ongoing funding for Market Demand Programs which will be distributed by formula to all institutions of higher education (UofU estimate $1.8M ongoing) Ø $1.8M from last year’s Engineering Initiative funding Ø $1.5M in ongoing funding for the University of Utah and Dixie State University Healthcare Partnership program Ø $1.5M in ongoing funding for Strategic Workforce Amendments (SB103) Ø $1.2M in one-time funding for the Huntsman Cancer Institute Ø -

DRAFT MINUTES SOCIAL SERVICES APPROPRIATIONS SUBCOMMITTEE Tuesday, February 11, 2020|7:59 A.M.|30 House Building
DRAFT MINUTES SOCIAL SERVICES APPROPRIATIONS SUBCOMMITTEE Tuesday, February 11, 2020|7:59 a.m.|30 House Building Members Present: Rep. Marsha Judkins Sen. Allen M. Christensen, Senate Chair Rep. Norman K. Thurston Rep. Paul Ray, House Chair Rep. Raymond P. Ward, House Vice Chair Members Absent: Sen. Luz Escamilla President J. Stuart Adams Sen. Keith Grover Sen. Kirk A. Cullimore Sen. Daniel Hemmert Rep. Adam Robertson Sen. Todd Weiler Rep. Steve R. Christiansen Staff Present: Rep. Kim F. Coleman Russell T. Frandsen, Finance Officer Rep. Jennifer Dailey-Provost Clare Tobin Lence, Finance Manager Rep. Brad M. Daw Kimberly D. Madsen, Financial Analyst Rep. Sandra Hollins An Bradshaw, Committee Secretary Note: A copy of related materials and an audio recording of the meeting can be found at www.le.utah.gov. Chair Christensen called the meeting to order at 8:22 a.m. 1 . Public Input on Topics on Today's Agenda Gary Edwards, Director, Salt Lake County Health Department and representing the Utah Association of Local Health Departments, spoke for funding for ICF - ID. Bill Cosgrove, pediatrician and Chair, Medicare Medical Care Advisory Committee, spoke in support of 12 month continuous enrollment. Seth Andrews, Primary Children's Hospital, spoke in support of 12 month continuous enrollment. 2 . Requests for Appropriation Russell Frandsen discussed alternative funding sources. 5b1-Home Health Hub - Itemized Budget 5b2-Home Health Hub Development Performance Measures Sen. Iwamoto and Clay Watson, past president of Utah Health Information Network, presented the budget request for Coordination of Care for Older Adults Receiving Health Care Services. Dr. Matt Hoffman, Chief Medical Informatics Officer, Utah Health Information Network, provided additional information.