Laboratory Diagnosis of Primary Immunodeficiencies.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

IDF Patient & Family Handbook
Immune Deficiency Foundation Patient & Family Handbook for Primary Immunodeficiency Diseases This book contains general medical information which cannot be applied safely to any individual case. Medical knowledge and practice can change rapidly. Therefore, this book should not be used as a substitute for professional medical advice. FIFTH EDITION COPYRIGHT 1987, 1993, 2001, 2007, 2013 IMMUNE DEFICIENCY FOUNDATION Copyright 2013 by Immune Deficiency Foundation, USA. REPRINT 2015 Readers may redistribute this article to other individuals for non-commercial use, provided that the text, html codes, and this notice remain intact and unaltered in any way. The Immune Deficiency Foundation Patient & Family Handbook may not be resold, reprinted or redistributed for compensation of any kind without prior written permission from the Immune Deficiency Foundation. If you have any questions about permission, please contact: Immune Deficiency Foundation, 110 West Road, Suite 300, Towson, MD 21204, USA; or by telephone at 800-296-4433. Immune Deficiency Foundation Patient & Family Handbook for Primary Immunodeficency Diseases 5th Edition This publication has been made possible through a generous grant from Baxalta Incorporated Immune Deficiency Foundation 110 West Road, Suite 300 Towson, MD 21204 800-296-4433 www.primaryimmune.org [email protected] EDITORS R. Michael Blaese, MD, Executive Editor Francisco A. Bonilla, MD, PhD Immune Deficiency Foundation Boston Children’s Hospital Towson, MD Boston, MA E. Richard Stiehm, MD M. Elizabeth Younger, CPNP, PhD University of California Los Angeles Johns Hopkins Los Angeles, CA Baltimore, MD CONTRIBUTORS Mark Ballow, MD Joseph Bellanti, MD R. Michael Blaese, MD William Blouin, MSN, ARNP, CPNP State University of New York Georgetown University Hospital Immune Deficiency Foundation Miami Children’s Hospital Buffalo, NY Washington, DC Towson, MD Miami, FL Francisco A. -

IDF Guide to Hematopoietic Stem Cell Transplantation
Guide to Hematopoietic Stem Cell Transplantation Immune Deficiency Foundation Guide to Hematopoietic Stem Cell Transplantation This publication contains general medical information that cannot be applied safely to any individual case. Medical knowledge and practice can change rapidly. Therefore, this publication should not be used as a substitute for professional medical advice. In all cases, patients and caregivers should consult their healthcare providers. Each patient’s condition and treatment are unique. Copyright 2018 by Immune Deficiency Foundation, USA Readers may redistribute this guide to other individuals for non-commercial use, provided that the text, html codes, and this notice remain intact and unaltered in any way. Immune Deficiency Foundation Guide to Hematopoietic Stem Cell Transplantation may not be resold, reprinted or redistributed for compensation of any kind without prior written permission from the Immune Deficiency Foundation (IDF). If you have any questions about permission, please contact: Immune Deficiency Foundation, 110 West Road, Suite 300, Towson, MD 21204, USA, or by telephone: 800-296-4433. For more information about IDF, go to: www.primaryimmune.org. This publication has been made possible through the IDF SCID Initiative and the SCID, Angels for Life Foundation. Acknowledgements The Immune Deficiency Foundation would like to thank the organizations and individuals who helped make this publication possible and contributed to the development of the Immune Deficiency Foundation Guide to Hematopoietic Stem -
Chapter 2 Agammaglobulinemia: X-Linked and Autosomal Recessive
Agammaglobulinemia: X-Linked and Autosomal Recessive Chapter 2 Agammaglobulinemia: X-Linked and Autosomal Recessive The basic defect in both X-Linked Agammaglobulinemia and autosomal recessive agammaglobulinemia is a failure of B-lymphocyte precursors to mature into B-lymphocytes and ultimately plasma cells. Since they lack the cells that are responsible for producing immunoglobulins, these patients have severe deficiencies of all types of immunoglobulins. Definition of X-Linked Agammaglobulinemia (XLA) and Autosomal Recessive Agammaglobulinemia (ARA) X-Linked Agammaglobulinemia (XLA) was first are not coated with antibody. All of these actions described in 1952 by Dr. Ogden Bruton. This disease, prevent germs from invading body tissues where they sometimes called Bruton’s Agammaglobulinemia or may cause serious infections. (See chapter titled “The Congenital Agammaglobulinemia, was one of the first Immune System and Primary Immunodeficiency immunodeficiency diseases to be identified. XLA is an Diseases.”) inherited immunodeficiency disease in which patients The basic defect in XLA is an inability of the patient to lack the ability to produce antibodies, the proteins that produce antibodies. Antibodies are produced by make up the gamma globulin or immunoglobulin specialized cells in the body, called plasma cells. fraction of blood plasma. Plasma cells develop in an orderly sequence of steps Antibodies are an integral part of the body’s defense beginning with stem cells located in the bone marrow. mechanism against certain types of microorganisms or The stem cells give rise to immature lymphocytes, germs, like bacteria or viruses. Antibodies are important called pro-B-lymphocytes. Pro-B-lymphocytes next in the recovery from infections and protect against develop into pre-B-cells, which then give rise to getting certain infections more than once. -

Practice Parameter for the Diagnosis and Management of Primary Immunodeficiency
Practice parameter Practice parameter for the diagnosis and management of primary immunodeficiency Francisco A. Bonilla, MD, PhD, David A. Khan, MD, Zuhair K. Ballas, MD, Javier Chinen, MD, PhD, Michael M. Frank, MD, Joyce T. Hsu, MD, Michael Keller, MD, Lisa J. Kobrynski, MD, Hirsh D. Komarow, MD, Bruce Mazer, MD, Robert P. Nelson, Jr, MD, Jordan S. Orange, MD, PhD, John M. Routes, MD, William T. Shearer, MD, PhD, Ricardo U. Sorensen, MD, James W. Verbsky, MD, PhD, David I. Bernstein, MD, Joann Blessing-Moore, MD, David Lang, MD, Richard A. Nicklas, MD, John Oppenheimer, MD, Jay M. Portnoy, MD, Christopher R. Randolph, MD, Diane Schuller, MD, Sheldon L. Spector, MD, Stephen Tilles, MD, Dana Wallace, MD Chief Editor: Francisco A. Bonilla, MD, PhD Co-Editor: David A. Khan, MD Members of the Joint Task Force on Practice Parameters: David I. Bernstein, MD, Joann Blessing-Moore, MD, David Khan, MD, David Lang, MD, Richard A. Nicklas, MD, John Oppenheimer, MD, Jay M. Portnoy, MD, Christopher R. Randolph, MD, Diane Schuller, MD, Sheldon L. Spector, MD, Stephen Tilles, MD, Dana Wallace, MD Primary Immunodeficiency Workgroup: Chairman: Francisco A. Bonilla, MD, PhD Members: Zuhair K. Ballas, MD, Javier Chinen, MD, PhD, Michael M. Frank, MD, Joyce T. Hsu, MD, Michael Keller, MD, Lisa J. Kobrynski, MD, Hirsh D. Komarow, MD, Bruce Mazer, MD, Robert P. Nelson, Jr, MD, Jordan S. Orange, MD, PhD, John M. Routes, MD, William T. Shearer, MD, PhD, Ricardo U. Sorensen, MD, James W. Verbsky, MD, PhD GlaxoSmithKline, Merck, and Aerocrine; has received payment for lectures from Genentech/ These parameters were developed by the Joint Task Force on Practice Parameters, representing Novartis, GlaxoSmithKline, and Merck; and has received research support from Genentech/ the American Academy of Allergy, Asthma & Immunology; the American College of Novartis and Merck. -

NIH Public Access Author Manuscript J Allergy Clin Immunol
NIH Public Access Author Manuscript J Allergy Clin Immunol. Author manuscript; available in PMC 2008 December 12. NIH-PA Author ManuscriptPublished NIH-PA Author Manuscript in final edited NIH-PA Author Manuscript form as: J Allergy Clin Immunol. 2007 October ; 120(4): 776±794. doi:10.1016/j.jaci.2007.08.053. The International Union of Immunological Societies (IUIS) Primary Immunodeficiency Diseases (PID) Classification Committee Raif. S. Geha, M.D., Luigi. D. Notarangelo, M.D. [Co-chairs], Jean-Laurent Casanova, M.D., Helen Chapel, M.D., Mary Ellen Conley, M.D., Alain Fischer, M.D., Lennart Hammarström, M.D., Shigeaki Nonoyama, M.D., Hans D. Ochs, M.D., Jennifer Puck, M.D., Chaim Roifman, M.D., Reinhard Seger, M.D., and Josiah Wedgwood, M.D. Abstract Primary immune deficiency diseases (PID) comprise a genetically heterogeneous group of disorders that affect distinct components of the innate and adaptive immune system, such as neutrophils, macrophages, dendritic cells, complement proteins, NK cells, as well as T and B lymphocytes. The study of these diseases has provided essential insights into the functioning of the immune system. Over 120 distinct genes have been identified, whose abnormalities account for more than 150 different forms of PID. The complexity of the genetic, immunological, and clinical features of PID has prompted the need for their classification, with the ultimate goal of facilitating diagnosis and treatment. To serve this goal, an international Committee of experts has met every two years since 1970. In its last meeting in Jackson Hole, Wyoming, United States, following three days of intense scientific presentations and discussions, the Committee has updated the classification of PID as reported in this article. -

Primary Immunodeficiency Disorders
ALLERGY AND IMMUNOLOGY 00954543 /98 $8.00 + .OO PRIMARY IMMUNODEFICIENCY DISORDERS Robert J. Mamlok, MD Immunodeficiency is a common thought among both patients and physicians when confronted with what is perceived as an excessive num- ber, duration, or severity of infections. Because of this, the starting point for evaluating patients for suspected immunodeficiency is based on what constitutes ”too many infections.” It generally is agreed that children with normal immune systems may have an average of 6 to 8 respiratory tract infections per year for the first decade of life. Even after a pattern of ab- normal infection is established, questions of secondary immunodeficiency should first be raised. The relatively uncommon primary immunodefi- ciency diseases are statistically dwarfed by secondary causes of recurrent infection, such as malnutrition, respiratory allergy, chronic cardiovascular, pulmonary, and renal disease, and environmental factors. On the other hand, a dizzying spiral of progress in our understanding of the genetics and immunology of primary immunodeficiency disease has resulted in improved diagnostic and therapeutic tools. Twenty-five newly recognized immunologic disease genes have been cloned in the last 5 ~ears.2~It has become arguably more important than ever for us to recognize the clinical and laboratory features of these relatively uncommon, but increasingly treatable, disorders. CLASSIFICATION The immune system has been classically divided into four separate arms: The B-cell system responsible for antibody formation, the T-cell sys- From the Division of Pediatric Allergy and Immunology, Texas Tech University Health Sci- ences Center, Lubbock, Texas PRIMARY CARE VOLUME 25 NUMBER 4 DECEMBER 1998 739 740 MAMLOK tem responsible for immune cellular regulation, the phagocytic (poly- morphonuclear and mononuclear) system and the complement (opsonic) system. -

Current Perspectives on Primary Immunodeficiency Diseases
Clinical & Developmental Immunology, June–December 2006; 13(2–4): 223–259 Current perspectives on primary immunodeficiency diseases ARVIND KUMAR, SUZANNE S. TEUBER, & M. ERIC GERSHWIN Division of Rheumatology, Allergy and Clinical Immunology, Department of Internal Medicine, University of California at Davis School of Medicine, Davis, CA, USA Abstract Since the original description of X-linked agammaglobulinemia in 1952, the number of independent primary immunodeficiency diseases (PIDs) has expanded to more than 100 entities. By definition, a PID is a genetically determined disorder resulting in enhanced susceptibility to infectious disease. Despite the heritable nature of these diseases, some PIDs are clinically manifested only after prerequisite environmental exposures but they often have associated malignant, allergic, or autoimmune manifestations. PIDs must be distinguished from secondary or acquired immunodeficiencies, which are far more common. In this review, we will place these immunodeficiencies in the context of both clinical and laboratory presentations as well as highlight the known genetic basis. Keywords: Primary immunodeficiency disease, primary immunodeficiency, immunodeficiencies, autoimmune Introduction into a uniform nomenclature (Chapel et al. 2003). The International Union of Immunological Societies Acquired immunodeficiencies may be due to malnu- (IUIS) has subsequently convened an international trition, immunosuppressive or radiation therapies, infections (human immunodeficiency virus, severe committee of experts every two to three years to revise sepsis), malignancies, metabolic disease (diabetes this classification based on new PIDs and further mellitus, uremia, liver disease), loss of leukocytes or understanding of the molecular basis. A recent IUIS immunoglobulins (Igs) via the gastrointestinal tract, committee met in 2003 in Sintra, Portugal with its kidneys, or burned skin, collagen vascular disease such findings published in 2004 in the Journal of Allergy and as systemic lupus erythematosis, splenectomy, and Clinical Immunology (Chapel et al. -

Antibody-Dependent Cellular Cytotoxicity in Primary Immunodeficiency Diseases and with Normal Leukocyte Subpopulations: IMPORTANCE of the TYPE of TARGET
Antibody-Dependent Cellular Cytotoxicity in Primary Immunodeficiency Diseases and with Normal Leukocyte Subpopulations: IMPORTANCE OF THE TYPE OF TARGET S. Ozden Sanal, Rebecca H. Buckley J Clin Invest. 1978;61(1):1-10. https://doi.org/10.1172/JCI108907. To gain insight into a possible role for antibody-dependent cell-mediated cytotoxicity in vivo, we examined the ability of leukocytes from 28 patients with primary immunodeficiency and from 20 normal controls to lyse three different types of antibody-coated targets in vitro. Mean cytotoxic indices ±1 SD elicited by unfractionated mononuclear cells from normal controls were 28.74±13.26 for human HLA antibody-coated lymphocyte targets, 42.79±8.27 for rabbit IgG antibody- coated chicken erythrocyte targets, and 47.58±10.34 for human anti-CD (Ripley)-coated O+ erythrocyte targets. Significantly (P=<0.05) lower than normal mean cytotoxic indices against lymphocyte targets were seen with effector cells from 10 patients with X-linked agammaglobulinemia (3.7±4.33), in 10 with common variable agammaglobulinemia (16.05±7.74), in 3 with immunodeficiency with hyper IgM (18.41±4.88), and in 2 with severe combined immunodeficiency (3.94±0.3). Antibody-dependent cytotoxicity against chicken erythrocytes was significantly (P=<0.05) lower than normal only in the common variable agammaglobulinemic group (33.33±12.3) and against human erythrocytes only in the common variable (34.36±9.59) and hyper IgM (27.54±0.66) groups. Rosette and anti-F(ab′)2 depletion studies with normal leukocytes indicated that a nonadherent, nonphagocytic, non-Ig-bearing, non-C receptor-bearing, Fc receptor- bearing lymphocyte was the only effector capable of lysing HLA antiboyd-coated lymphocyte targets. -

Warning Signs of Primary Immunodeficiency for Specialty Care Physicians
Juan Carlos Aldave, MD Allergy and Clinical Immunology Rebagliati Martins National Hospital, Lima-Peru [email protected] Warning signs of Primary Immunodeficiency for specialty care physicians The clinical presentation of PID can be diverse. However, there are clinical findings at the level of different organs and systems requiring PID suspicion; these findings must be quickly recognized by specialty care physicians: ALLERGY: Clinical manifestation Suspicion of PID Difficult-to-control asthma Selective IgA deficiency Common variable immunodeficiency (CVID) Specific antibody deficiency Recurrent or complicated sinusitis Antibody deficiencies Recurrent or complicated otitis Antibody deficiencies Eczema Wiskott-Aldrich syndrome Hyper-IgE syndrome Omenn syndrome IPEX ((immunodysregulation, polyendocrinopathy, enteropathy, X- linked syndrome) Netherton syndrome (ichthyosiform erythroderma, ichthyosis linearis, bamboo hair) Recurrent angioedema Hereditary angioedema (C1inh deficiency) Severe food and/or drug allergies DOCK8 defect (hyper-IgE syndrome) CARDIOLOGY: Clinical manifestation Suspicion of PID Congenital heart disease (interrupted DiGeorge syndrome aortic arch, pulmonary atresia, aberrant subclavian, tetralogy of Fallot) Congenital heart defects CHARGE syndrome (coloboma, heart defect, atresia choanae, retarded growth, genital hypoplasia, ear anomalies/deafness) THORACIC SURGERY: Clinical manifestation Suspicion of PID Thymoma and Good syndrome hypogammaglobulinemia Congenital heart disease (interrupted DiGeorge -

Blueprint Genetics Severe Combined Immunodeficiency Panel
Severe Combined Immunodeficiency Panel Test code: IM0101 Is a 80 gene panel that includes assessment of non-coding variants. Is ideal for patients with a clinical suspicion of combined immunodeficiencies. The genes on this panel are included in the Primary Immunodeficiency Panel. About Severe Combined Immunodeficiency Severe combined immunedeficiencies (SCIDs) are a group of primary immunodeficiencies characterized by specific mutations in genes of T and B-lymphocyte systems and leading to little or no immune response. Different subtypes of SCIDs are characterized and subdivided by the presence of circulating T and B cells. T cells are absent or markedly decreased in the most types, but levels of B cells vary. In addition, both of these disease subgroups (T-B+ and T-B-) can occur with or without NK cells. Patients with SCID are susceptible to recurrent infections that can be fatal. The worldwide prevalence of SCID is estimated to be at least 1:100,000 births, while some genetically more homogenous populations may show markedly increased numbers. Mutations in IL2RG are the most common reason for SCIDs, explaining approximately 50% of all cases and close to 100% of X-linked cases. Availability 4 weeks Gene Set Description Genes in the Severe Combined Immunodeficiency Panel and their clinical significance Gene Associated phenotypes Inheritance ClinVar HGMD ADA Severe combined immunodeficiency due to adenosine deaminase AR 49 93 deficiency AK2 Reticular dysgenesis AR 14 17 ATM Breast cancer, Ataxia-Telangiectasia AD/AR 1047 1109 BCL11B Immunodeficiency -

Patient & Family Handbook
Immune Deficiency Foundation Patient & Family Handbook For Primary Immunodeficiency Diseases This book contains general medical information which cannot be applied safely to any individual case. Medical knowledge and practice can change rapidly. Therefore, this book should not be used as a substitute for professional medical advice. SIXTH EDITION COPYRIGHT 1987, 1993, 2001, 2007, 2013, 2019 IMMUNE DEFICIENCY FOUNDATION Copyright 2019 by Immune Deficiency Foundation, USA. Readers may redistribute this article to other individuals for non-commercial use, provided that the text, html codes, and this notice remain intact and unaltered in any way. The Immune Deficiency Foundation Patient & Family Handbook may not be resold, reprinted or redistributed for compensation of any kind without prior written permission from the Immune Deficiency Foundation. If you have any questions about permission, please contact: Immune Deficiency Foundation, 110 West Road, Suite 300, Towson, MD 21204, USA; or by telephone at 800-296-4433. Immune Deficiency Foundation Patient & Family Handbook For Primary Immunodeficiency Diseases 6th Edition The development of this publication was supported by Shire, now Takeda. 110 West Road, Suite 300 Towson, MD 21204 800.296.4433 www.primaryimmune.org [email protected] Editors Mark Ballow, MD Jennifer Heimall, MD Elena Perez, MD, PhD M. Elizabeth Younger, Executive Editor Children’s Hospital of Philadelphia Allergy Associates of the CRNP, PhD University of South Florida Palm Beaches Johns Hopkins University Jennifer Leiding, -
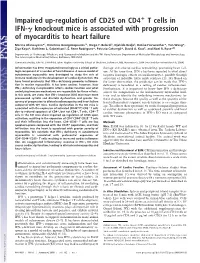
Impaired Up-Regulation of CD25 on CD4 T Cells in IFN-␥ Autoimmune Diseases
Impaired up-regulation of CD25 on CD4؉ T cells in IFN-␥ knockout mice is associated with progression of myocarditis to heart failure Marina Afanasyeva*†, Dimitrios Georgakopoulos†‡, Diego F. Belardi‡, Djahida Bedja§, DeLisa Fairweather*, Yan Wang*, Ziya Kaya*, Kathleen L. Gabrielson§, E. Rene Rodriguez*, Patrizio Caturegli*, David A. Kass‡, and Noel R. Rose*¶ʈ Departments of *Pathology, ‡Medicine, and §Comparative Medicine and the ¶W. Harry Feinstone Department of Molecular Microbiology and Immunology, The Johns Hopkins Medical Institutions, Baltimore, MD 21205 Communicated by John W. Littlefield, Johns Hopkins University School of Medicine, Baltimore, MD, November 5, 2004 (received for review March 8, 2004) Inflammation has been recognized increasingly as a critical patho- damage and adverse cardiac remodeling, promoting heart fail- logic component of a number of heart diseases. A mouse model of ure. At the same time, IFN-␥ has been reported to exert direct autoimmune myocarditis was developed to study the role of negative inotropic effects on cardiomyocytes, possibly through immune mediators in the development of cardiac dysfunction. We activation of inducible nitric oxide synthase (13, 14). Based on have found previously that IFN-␥ deficiency promotes inflamma- the latter observation, the prediction can be made that IFN-␥ tion in murine myocarditis. It has been unclear, however, how deficiency is beneficial in a setting of cardiac inflammation. IFN-␥ deficiency in myocarditis affects cardiac function and what Furthermore, it is important