Chimanimani and Chipinge Emergency and Early Recovery WASH Program (CCEER)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Evolving Water Point Mapping to Strategic Decision Making in Rural Malawi
MILLER et al. 41st WEDC International Conference, Egerton University, Nakuru, Kenya, 2018 TRANSFORMATION TOWARDS SUSTAINABLE AND RESILIENT WASH SERVICES Evolving water point mapping to strategic decision making in rural Malawi A. Miller, M. Nhlema, S. Kumwenda, E. Mbalame, Z. Uka, J. Feighery & R. Kalin (UK) PAPER 2920 There is a need to evolve from the simple mapping of water points, now often numerous, to effective decision making using these data. This paper outlines new developments of mWater as the preferred online Management Information System (MIS) tool to analyse significant volumes of water and sanitation data in Malawi. mWater exemplifies an evolving strategic decision-making tool used to formulate rural water supply investment strategies. A time series of 25,000 water points have been mapped since 2011 to build a complete asset register of water infrastructure to support government endeavours to reach Sustainable Development Goal 6. This comprehensive live database allows real-time analysis of over sixty variables, including linkage to concurrent mWater sanitation and waste data. This paper briefly illustrates several emergent uses of the facility to exemplify its potential in strategic decision making using Big Data. It is currently being rolled out across the entire country. Introduction Vast numbers of water point supplies continue to be installed across the developing world in an effort to meet United Nations Sustainable Development Goal 6 (SDG6) to “ensure availability and sustainable management of water and sanitation for all” (United Nations, 2017). It is paramount these investments are sustainable over time, and that robust management information systems (MISs) are developed to not only map this dynamic proliferation, but to critically use water point data within effective decision making to enable responsive sustainable management of the water resources within surrounding environments. -

Crop Area, Condition and Stage
Foreword The Government of Zimbabwe has continued to exhibit its commitment for reducing food and nutrition insecurity in Zimbabwe. Evidence include the culmination of ZimASSET’s Food and Nutrition Security Cluster and the multi-sector Food and Nutrition Security Policy (FNSP). Recognising the vagaries of climate variabilities and the unforeseeable potential livelihood challenges, Government put in place structures whose mandates are, among other things to provide early warning information for early actioning. The Food and Nutrition Council, through the ZimVAC, is one of such structures which strives to fulfil the aspirations of the FNSP’s commitment number 6 of providing food and nutrition early warning information. In response to the advent of the El Nino phenomena which has resulted in the country experiencing long dry spells, the ZimVAC undertook a rapid assessment focussing on updating the ZimVAC May 2015 results. The lean season monitoring focused on the relevant food and nutrition security parameters. The process followed a 3 pronged approach which were, a review of existing food and nutrition secondary data, qualitative district Focus Group Discussions (FGDs) and for other variables a quantitative household survey which in most cases are representative at provincial and national level. This report provides a summation of the results for the 3 processes undertaken and focuses on the following thematic areas: the rainfall season quality, 2015/16 agricultural assistance, crop and livestock condition, food and livestock markets, gender based violence, household income sources and livelihoods strategies, domestic and production water situation, health and nutrition, food assistance and a review of the rural food security projections. -
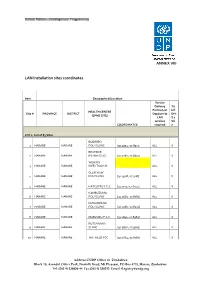
LAN Installation Sites Coordinates
ANNEX VIII LAN Installation sites coordinates Item Geographical/Location Service Delivery Tic Points (List k if HEALTH CENTRE Site # PROVINCE DISTRICT Dept/umits DHI (EPMS SITE) LAN S 2 services Sit COORDINATES required e LOT 1: List of 83 Sites BUDIRIRO 1 HARARE HARARE POLYCLINIC [30.9354,-17.8912] ALL X BEATRICE 2 HARARE HARARE RD.INFECTIO [31.0282,-17.8601] ALL X WILKINS 3 HARARE HARARE INFECTIOUS H ALL X GLEN VIEW 4 HARARE HARARE POLYCLINIC [30.9508,-17.908] ALL X 5 HARARE HARARE HATCLIFFE P.C.C. [31.1075,-17.6974] ALL X KAMBUZUMA 6 HARARE HARARE POLYCLINIC [30.9683,-17.8581] ALL X KUWADZANA 7 HARARE HARARE POLYCLINIC [30.9285,-17.8323] ALL X 8 HARARE HARARE MABVUKU P.C.C. [31.1841,-17.8389] ALL X RUTSANANA 9 HARARE HARARE CLINIC [30.9861,-17.9065] ALL X 10 HARARE HARARE HATFIELD PCC [31.0864,-17.8787] ALL X Address UNDP Office in Zimbabwe Block 10, Arundel Office Park, Norfolk Road, Mt Pleasant, PO Box 4775, Harare, Zimbabwe Tel: (263 4) 338836-44 Fax:(263 4) 338292 Email: [email protected] NEWLANDS 11 HARARE HARARE CLINIC ALL X SEKE SOUTH 12 HARARE CHITUNGWIZA CLINIC [31.0763,-18.0314] ALL X SEKE NORTH 13 HARARE CHITUNGWIZA CLINIC [31.0943,-18.0152] ALL X 14 HARARE CHITUNGWIZA ST.MARYS CLINIC [31.0427,-17.9947] ALL X 15 HARARE CHITUNGWIZA ZENGEZA CLINIC [31.0582,-18.0066] ALL X CHITUNGWIZA CENTRAL 16 HARARE CHITUNGWIZA HOSPITAL [31.0628,-18.0176] ALL X HARARE CENTRAL 17 HARARE HARARE HOSPITAL [31.0128,-17.8609] ALL X PARIRENYATWA CENTRAL 18 HARARE HARARE HOSPITAL [30.0433,-17.8122] ALL X MURAMBINDA [31.65555953980,- 19 MANICALAND -

February 2011
Zimbabwe Weekly Epidemiological Bulletin Number 102 Epidemiological week 10 (week ending 13 March) March 2011 Highlights Malaria outbreaks in Kadoma and Makoni Figure 1: Cumulative Cholera Cases since 1 January 2011 Cholera cases reported in Chiredzi Contents Chipinge 133 A. General context Mutare 86 B. Epidemic prone diseases C. Events of public health concern in the region Buhera 66 D. Preparedness Chiredzi E. Timeliness and completeness of data 42 F. Recommendations for action/follow up Bikita 42 Annex 1: National summary of cases/deaths by condition District Murewa 5 by week Annex 2: Standard case definitions and alert/action Chimanimani 4 epidemic thresholds Kadoma 2 Mutasa 1 A. General context 0 50 100 150 Cholera cases Cholera continues to be reported in week 10 of 2011, having spilled over from 2010. Since week 45 of Figure 2: Zimbabwe Cholera Epicurve, Week 5, 2010 to Week 10, 2011 2010, no new outbreaks of measles have been reported, although the situation is being closely 200 monitored. We are amidst the malaria season and 180 malaria outbreaks are now being reported. Within the C 160 region, suspected Rift Valley fever has been reported h 140C in South Africa. o 120a l 100s B. Epidemic prone diseases e e80 r 60s Cholera 40 a 20 Nine out of the 62 districts, namely: Bikita, Buhera, 0 17 33 5 9 13 21 25 29 37 41 45 49 1 5 9 Chimanimani, Chipinge, Chiredzi, Kadoma,Murewa, 1 Mutare and Mutasa have reported cases since the start of 2011. There were 381 cumulative cases: 324 2010 2011 suspected cases, 57 laboratory confirmed cases and 7 Epidemiological Week Number by year th deaths reported by the 13 March 2011. -

Water Point Mapping in East Africa Based on a Strategic Review of Ethiopia, Tanzania, Kenya and Uganda
Report Water point mapping in East Africa Based on a strategic review of Ethiopia, Tanzania, Kenya and Uganda A WaterAid report By Katharina Welle March 2010 Acknowledgements: This report was prepared for WaterAid’s East Africa region by Katharina Welle, with support from Yunia Musaazi, Tom Slaymaker, Vincent Casey and Lydia Zigomo. The contributions of country programme staff to the review process are gratefully acknowledged. Front cover image: WaterAid/Marco Betti Three pupils at their school’s water point, Ethiopia. The school has taps and girls’ and boys’ latrines, as well as a sanitation club. The pupils clean the compound every Friday, and the sanitation club perform regular plays to educate the pupils about sanitation and hygiene. Report ________________________________________________________________________________ Acronyms ________________________________________________________________________________ GIS Geographic Information System GLAAS Global Annual Assessment of Sanitation and Drinking Water (UN) GPS Global Positioning System HEWASA Health through Water and Sanitation Program ISF Ingeneras sin Fronteras (Engineers without Borders) JMP Joint Monitoring Program JSR Joint Sector Review M&E Monitoring and Evaluation MIS Management Information System MoWE Ministry of Water and Environment (Uganda) MoWI Ministry of Water and Irrigation (Tanzania, Kenya) MoWR Ministry of Water Resources (Ethiopia) NGO Non Governmental Organisation OECD Organisation for Economic Cooperation and Development SIMS Sector Information Management System -

John H. Peterson, Jr., Professor, Department of Sociology And
BOTTOM UP DEVELOPMENT IN DECENTRALIZED COMMON PROPERTY REGIMES: THE EXPERIENCES OF TWO DISTRICT COUNCILS IN SOUTHEASTERN ZIMBABWE John H. Peterson, Jr., Professor, Department of Sociology and Anthropology, PO Drawer C, Mississippi State, MS 39762; Fulbright Visiting Lecturer 1990-1991, Centre for Applied Social Science, University of Zimbabwe, PO Box MP 167, Mount Pleasant, Harare, Zimbabwe Paper presented at the International Association for the Study of Common Property, Common Property Conference, Winnipeg, Canada, September 26 - 29, 1991 The Communal Areas Management Program for Indigenous Resources (CAMPFIRE) in Zimbabwe seeks to substitute decentralized management and control of natural resources, especially wildlife, for centralized ownership and control. The preservation and utilization of Zimbabwe's natural resources through the CAMPFIRE program involves some important issues in addition to decentralization including conservation through utilization, and sustained development. A fifteen minute presentation can not begin to cover even one of these issues. I am focusing on decentralization because I was struck by the frequency with which leaders at the national and even district level continue to question the degree to which people at the community level are competent to made decisions about common property resources. Decentralization of common property resources raises the question of how far and to whom. There are no simple answers. But there are many potential recipients for decentralized control, each with a case for maintaining controls at particular levels or within some existing institutions. The greatest devolution of management would be to socio- governmental units with the least formal structures - the village and the ward. These people are most familiar with the wildlife and the practical realities of its management. -

The Sustainability of Water Supply Schemes
Research-inspired Policy and Practice Learning in Ethiopia and the Nile region DRAFT The Sustainability of Water Supply Schemes A case study in Alaba Special woreda Israel Deneke and Habtamu Abebe Hawassa March 2008 Working Paper 5 Research-inspired Policy and Practice Learning in Ethiopia and the Nile region (RiPPLE) Research-inspired Policy and Practice Learning in Ethiopia and the Nile region (RiPPLE) is a five-year research programme consortium funded by the UK's Department for International Development (DFID). It aims to advance evidence-based learning on water supply and sanitation (WSS) focusing specifically on issues of planning, financing, delivery and sustainability and the links between sector improvements and pro-poor economic growth. RIPPLE Working Papers contain research questions, methods, preliminary analysis and discussion of research results (from case studies or desk research). They are intended to stimulate debate on policy implications of research findings as well as feed into Long-term Action Research. RiPPLE Office, c/o WaterAid Ethiopia, Kirkos Sub-city, Kebele 04, House no 620, Debrezeit Road, PO Box 4812, Addis Ababa, Ethiopia. Acknowledgements The authors of this paper would like to thank the following for their invaluable support and time: • The Woreda LPA members for their support and time; • Desta Dimste, SNNPR Regional Facilitator, RiPPLE • Aschalew Sidelil, Alaba Special woreda Facilitator, RiPPLE • Tsegaw Hailu, Mirab Abaya woreda Facilitaor, RiPPLE • GaP theme members 1 Working Paper 5: The Sustainability -

UNICEF – Mozambique WASH for Children in Zambézia Province
SUBMITTED UNICEF – Mozambique WASH for Children in Zambézia Province Annex 1 Water supply, sanitation and hygiene in rural communities and schools (2014-2017) Programme Proposal September 2014 ACH 2009 1 SUBMITTED Contents 1. Overview ......................................................................................................................................... 4 2. Programme Rationale ..................................................................................................................... 4 WASH is critical to development ............................................................................................................ 4 Context in Mozambique .......................................................................................................................... 5 Context in Zambézia ............................................................................................................................... 5 3. The UNICEF WASH Approach .......................................................................................................... 6 4. Zambézia Programme Description .................................................................................................. 8 Impact ................................................................................................................................................... 10 Outcomes .............................................................................................................................................. 10 Outputs and activities -

Zimbabwe HIV Care and Treatment Project Baseline Assessment Report
20 16 Zimbabwe HIV Care and Treatment Project Baseline Assessment Report '' CARG members in Chipinge meet for drug refill in the community. Photo Credits// FHI 360 Zimbabwe'' This study is made possible through the support of the American People through the United States Agency for International Development (USAID.) The contents are the sole responsibility of the Zimbabwe HIV care and Treatment (ZHCT) Project and do not necessarily reflect the views of USAID or the U.S. Government. FOREWORD The Government of Zimbabwe (GoZ) through the Ministry of Health and Child Care (MoHCC) is committed to strengthening the linkages between public health facilities and communities for HIV prevention, care and treatment services provision in Zimbabwe. The Ministry acknowledges the complementary efforts of non-governmental organisations in consolidating and scaling up community based initiatives towards achieving the UNAIDS ‘90-90-90’ targets aimed at ending AIDS by 2030. The contribution by Family Health International (FHI360) through the Zimbabwe HIV Care and Treatment (ZHCT) project aimed at increasing the availability and quality of care and treatment services for persons living with HIV (PLHIV), primarily through community based interventions is therefore, lauded and acknowledged by the Ministry. As part of the multi-sectoral response led by the Government of Zimbabwe (GOZ), we believe the input of the ZHCT project will strengthen community-based service delivery, an integral part of the response to HIV. The Ministry of Health and Child Care however, has noted the paucity of data on the cascade of HIV treatment and care services provided at community level and the ZHCT baseline and mapping assessment provides valuable baseline information which will be used to measure progress in this regard. -

MASHONALAND EAST PROVINCE - Overview Map 26 October 2009 Legend Province Capital
MASHONALAND EAST PROVINCE - Overview Map 26 October 2009 Legend Province Capital Hunyani Casembi Key Location Chikafa Chidodo Muzeza Musengezi Mine Mushumbi Musengezi Pools Chadereka Mission Mbire Mukumbura Place of Local Importance Hoya Kaitano Kamutsenzere Kamuchikukundu Bwazi Muzarabani Mavhuradonha Village Bakasa St. St. Gunganyama Pachanza Centenary Alberts Alberts Nembire Road Network Kazunga Chawarura Dotito Primary Chironga Rushinga Mount Rushinga Mukosa Guruve Karanda Rusambo Marymount Chimanda Secondary Marymount Shinje Darwin Rusambo Centenary Nyamatikiti Guruve Feeder azowe MashonalandMount M River Goromonzi Darwin Mudindo Dindi Kafura Bure Nyamanyora Railway Line Central Goora Kondo Madombwe Chistungo Mutepatepa Dendera Nyamapanda International Boundary Madziwa Borera Chiunye Kotwa Nyakudya Shinga Bradley Jester Mvurwi Madziwa Vanad Kasimbwi Institute Masarakufa Nzvimbo Madziwa Province Boundary Feock Mutawatawa Mudzi Muswewenhede Chakonda Suswe Mudzi Mutorashanga Charewa Chikwizo Howard District Boundary Nyota Shamva Nyamatawa Gozi Institute Bindura Chindengu Kawere Muriel Katiyo Rwenya Freda & Mont Dor Caesar Nyamuzuwe River Mazowe Rebecca Uzumba Nyamuzuwe Katsande Makaha River Shamva Mudzonga Makosa Trojan Shamva Nyamakope Fambe Glendale BINDURA MarambaKarimbika Sutton Amandas Uzumba All Nakiwa Kapondoro Concession Manhenga Kanyongo Souls Great Muonwe Mutoko PfungweMuswe Dyke Mushimbo Chimsasa Lake/Waterbody Madamombe Jumbo Bosha Nyadiri Avila Makumbe Mutoko Jumbo Mazowe Makumbe Parirewa Nyawa Rutope Conservation Area -

Functionality of Handpump Water Supplies: a Review of Data from Sub-Saharan Africa and the Asia-Pacific Region
International Journal of Water Resources Development ISSN: 0790-0627 (Print) 1360-0648 (Online) Journal homepage: https://www.tandfonline.com/loi/cijw20 Functionality of handpump water supplies: a review of data from sub-Saharan Africa and the Asia-Pacific region Tim Foster, Sean Furey, Brian Banks & Juliet Willetts To cite this article: Tim Foster, Sean Furey, Brian Banks & Juliet Willetts (2019): Functionality of handpump water supplies: a review of data from sub-Saharan Africa and the Asia-Pacific region, International Journal of Water Resources Development, DOI: 10.1080/07900627.2018.1543117 To link to this article: https://doi.org/10.1080/07900627.2018.1543117 View supplementary material Published online: 11 Mar 2019. Submit your article to this journal Article views: 343 View related articles View Crossmark data Full Terms & Conditions of access and use can be found at https://www.tandfonline.com/action/journalInformation?journalCode=cijw20 INTERNATIONAL JOURNAL OF WATER RESOURCES DEVELOPMENT https://doi.org/10.1080/07900627.2018.1543117 Functionality of handpump water supplies: a review of data from sub-Saharan Africa and the Asia-Pacific region Tim Foster a, Sean Fureyb, Brian Banksc and Juliet Willetts a aInstitute for Sustainable Futures, University of Technology Sydney, Ultimo, Australia; bSKAT Foundation, St. Gallen, Switzerland; cGlobal Water Challenge, Global Environment & Technology Foundation, Arlington, VA, USA ABSTRACT ARTICLE HISTORY Handpumps are heavily relied upon for drinking water in rural areas of Received 17 April 2018 low- and middle-income countries, but their operation and mainte- Accepted 29 October 2018 nance remain problematic. This review presents updated and KEYWORDS expanded handpump functionality estimates for 47 countries in sub- Rural water supply; Saharan Africa and the Asia-Pacific region. -

Manicaland-Province
School Level Province District School Name School Address Secondary Manicaland Buhera BANGURE ZVAVAHERA VILLAGE WARD 19 CHIEF NYASHANU BUHERA Secondary Manicaland Buhera BETERA HEADMAN BETERA CHIEF NYASHANU Secondary Manicaland Buhera BHEGEDHE BHEGEDHE VILLAGE CHIEF CHAMUTSA Secondary Manicaland Buhera BIKA KWARAMBA VILLAGE WARD 16 CHIEF NYASHANU Secondary Manicaland Buhera BUHERA GAVA VILLAGE WARD 5 CHIEF MAKUMBE BUHERA Secondary Manicaland Buhera CHABATA MUVANGIRWA VILLAGE WARD 29 Secondary Manicaland Buhera CHANGAMIRE MATSVAI VILLAGE WARD 32 NYASHANU Secondary Manicaland Buhera CHAPANDUKA CHAPANDUKA VILLAGE CHIEF NYASHANU Secondary Manicaland Buhera CHAPWANYA CHAPWANYA HIGH SCHOOL WARD 2 BUHERA Secondary Manicaland Buhera CHAWATAMA CHAWATAMA VILLAGE WARD 31 CHIEF MAKUMBE Secondary Manicaland Buhera CHIMBUDZI MATASVA VILLAGE WARD 32 CHIEF NYASHANU CHINHUWO VILLAGE CHIWENGA TOWNSHIP CHIEF Secondary Manicaland Buhera CHINHUWO NYASHANU Secondary Manicaland Buhera CHIROZVA CHIROZVA VILLAGE Secondary Manicaland Buhera CHIURWI CMAKUVISE VILLAGE WARD 32 Secondary Manicaland Buhera DEVULI NENDANDA VILLAGE CHIEF CHAMUTSA WARD 33 Secondary Manicaland Buhera GOSHO SOJINI VILLAGE WARD 5 CHIEF MAKUMBE Secondary Manicaland Buhera GOTORA GOTORA VILLAGE WARD 22 CHIEF NYASHANU BUHERA Secondary Manicaland Buhera GUNDE MABARA VILLAGE WARD 9 CHIEF CHITSUNGE BUHERA Secondary Manicaland Buhera GUNURA CHIEF CHAMUTSA NEMUPANDA VILLAGE WARD 30 BUHERA Secondary Manicaland Buhera GWEBU GWEBU SECONDARY GWEBU VILLAGE Secondary Manicaland Buhera HANDE KARIMBA VILLAGE