Recommendations for the Practice of Echocardiography in Infective Endocarditis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Cardiac CT - Quantitative Evaluation of Coronary Calcification
Clinical Appropriateness Guidelines: Advanced Imaging Appropriate Use Criteria: Imaging of the Heart Effective Date: January 1, 2018 Proprietary Date of Origin: 03/30/2005 Last revised: 11/14/2017 Last reviewed: 11/14/2017 8600 W Bryn Mawr Avenue South Tower - Suite 800 Chicago, IL 60631 P. 773.864.4600 Copyright © 2018. AIM Specialty Health. All Rights Reserved www.aimspecialtyhealth.com Table of Contents Description and Application of the Guidelines ........................................................................3 Administrative Guidelines ........................................................................................................4 Ordering of Multiple Studies ...................................................................................................................................4 Pre-test Requirements ...........................................................................................................................................5 Cardiac Imaging ........................................................................................................................6 Myocardial Perfusion Imaging ................................................................................................................................6 Cardiac Blood Pool Imaging .................................................................................................................................12 Infarct Imaging .....................................................................................................................................................15 -
Resting Coronary Flow Velocity in The
European Heart Journal – Cardiovascular Imaging (2012) 13,79–85 CLINICAL/ORIGINAL PAPERS doi:10.1093/ehjci/jer153 Resting coronary flow velocity in the functional evaluation of coronary artery stenosis: study on sequential use of computed tomography angiography and transthoracic Doppler Downloaded from https://academic.oup.com/ehjcimaging/article/13/1/79/2397059 by guest on 30 September 2021 echocardiography Esa Joutsiniemi 1, Antti Saraste 1,2*, Mikko Pietila¨ 1, Heikki Ukkonen 1,2, Sami Kajander 2, Maija Ma¨ki 2,3, Juha Koskenvuo 3, Juhani Airaksinen 1, Jaakko Hartiala 3, Markku Saraste 3, and Juhani Knuuti 2 1Department of Cardiology, Turku University Hospital, Kiinamyllynkatu 4-8, 20520 Turku, Finland; 2Turku PET Centre, Kiinamyllynkatu 4-8, 20520 Turku, Finland; and 3Department of Clinical Physiology and Nuclear Medicine, Turku University Hospital, Kiinamyllynkatu 4-8, 20520 Turku, Finland Received 10 March 2011; accepted after revision 2 August 2011; online publish-ahead-of-print 30 August 2011 Aims Accelerated flow at the site of flow-limiting stenosis can be detected by transthoracic Doppler echocardiography (TTDE). We studied feasibility and accuracy of sequential coronary computed tomography angiography (CTA) and TTDE in detection of haemodynamically significant coronary artery disease (CAD). ..................................................................................................................................................................................... Methods We prospectively enrolled 107 patients with intermediate (30–70%) pre-test likelihood of CAD. All patients under- and results went CTA using a 64-slice scanner. Using TTDE, the ratio of maximal diastolic flow velocity to pre-stenotic flow velocity (M/P ratio) was measured in the coronary segments with stenosis in CTA. In all patients, the results were compared with invasive coronary angiography, including measurement of fractional flow reserve when appropriate. -

CASE REPORTS Supraventricular Tachycardia As the Initial
http://crim.sciedupress.com Case Reports in Internal Medicine, 2015, Vol. 2, No. 3 CASE REPORTS Supraventricular tachycardia as the initial presentation of bacterial infective endocarditis: A rare case report Wei-Tsung Wu1, Hung-Ling Huang2, Ho-Ming Su1, 3, Tsung-Hsien Lin1, 3, Kun-Tai Lee1, 3, Sheng-Hsiung Sheu1, 3, Po-Chao Hsu1, 3 1. Division of Cardiology, Department of Internal Medicine, Kaohsiung Medical University Hospital, Kaohsiung Medical University, Kaohsiung, Taiwan, ROC. 2. Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Kaohsiung Medical University Hospital, Kaohsiung Medical University, Kaohsiung, Taiwan, ROC. 3. Department of Internal Medicine, Faculty of Medicine, School of Medicine, Kaohsiung Medical University, Kaohsiung, Taiwan, ROC Correspondence: Po-Chao Hsu. Address: Division of Cardiology, Department of Internal Medicine, Kaohsiung Medical University Hospital, 100 Tzyou 1st Road, Kaohsiung. 80708, Taiwan, ROC. Email: [email protected] Received: May 19, 2015 Accepted: June 15, 2015 Online Published: June 17, 2015 DOI: 10.5430/crim.v2n3p26 URL: http://dx.doi.org/10.5430/crim.v2n3p26 Abstract Infective endocarditis (IE) is an infection of the heart valves or the heart’s inner lining. The clinical symptoms of infectious endocarditis vary considerably, some are subtle and non-specific, which make the diagnosis difficult or the signs misleading. In some cases cardiac symptoms are associated with intra cardiac extension of the infection, including murmur, conduction blocks and congestive heart failure. However, there was no literature description of supraventricular tachycardia (SVT) as the initial presentation of IE. Herein we report a case of bacterial IE with SVT as the initial presentation of disease, which finally leaded to catastrophic outcome. -

Unique Mitral Valve Mass: Think Beyond Vegetation
Published online: 2021-08-09 CASE REPORT Unique mitral valve mass: Think beyond vegetation Mahmoud Farhoud, Husam Bakdash Department of Internal Medicine, University of Kansas School of Medicine, Wichita, Kansas, United States Access this article online ABSTRACT Website: www.avicennajmed.com DOI: 10.4103/2231-0770.140661 Osteosarcoma is a rare cardiac malignant tumor. This case of cardiac osteosarcoma presented Quick Response Code: with atrial fibrillation. Initial echocardiogram demonstrated mitral valve echodensity and mitral valve regurgitation. Surgery and histopathological examination identified the tumor as an osteosarcoma. Tumor grade appeared to be prognostically important in cardiac sarcoma, with poor prognosis in high‑grade tumors. Key words: Atrial fibrillation, cardiac osteosarcoma, mitral valve, vegetation INTRODUCTION An electrocardiogram showed AF with RVR and no specific ST segment or T wave abnormalities. The patient was A primary cardiac malignant tumor is very rare. About 75% admitted to the telemetry ward and started on diltiazem drip. of primary cardiac tumors are benign, and 75% of these are atrial myxomas.[1] Most cardiac malignant tumors are Transthoracic echocardiography demonstrated normal metastatic tumors from melanoma, lung carcinoma, and systolic function and the anterior mitral valve leaflet was breast carcinoma.[2] Primary cardiac osteosarcomas usually severely thickened, with extensive vegetation/mass involving originate in the left atrium.[3] In contrast, osteosarcomas the whole leaflet [Figure 1 and Video 1]. There were severe metastatic to the heart most commonly involve the right mitral regurgitation and moderate mitral stenosis. Blood cardiac chambers.[4] We present a patient who had atrial cultures and serologies for cat scratch disease, brucella, fibrillation (AF) and mitral valve mass. -

Myocarditis, Pericarditis Cardiomyopathies
Endocarditis, myocarditis, pericarditis. Cardiomyopathies Attila Zalatnai Endocarditis: inflammation of the endocardium, especially the valves 1. Infective endocarditis: (bacteria, fungi) Predisposing factors: - septicemia - valve malformations - deformed, calcified valves - arteficial valve implantation - previous rheumatic fever - peridontal, periapical foci! Most important causative agents: Strcc. viridans Enterococcus (Str. fecalis) Staphylococcus aureus Candida species Morphology: Vegetations Valve destruction Both Complications: embolization (septic emboli, septic abscesses) sepsis „mycotic aneurysms”, subarachnoidal hemorrhage acute left sided heart failure (regurgitation, chorda tendinea rupture) healing by scarring and calcification VITIUM stenosis insufficiency combined 2. Non-infective endocarditis: verrucous endocarditis (rheumatic fever) SLE (Libman-Sacks endocarditis) – atypical „marantic” endocarditis - paraneoplastic Myocarditis: an inflammatory infiltrate (helper T-cells, macrophages) of the myocardium with necrosis and/or degeneration of adjacent myocytes Genetic and environmental disposition + causative mechanisms Direct cytotoxic Aberrant effect of infectious induction of causative agents apoptosis Cytokine expression in the myocardium Secondary autoimmune (TNF-alpha, NOS) mechanisms Etiology of the myocarditis - I. Infectious origin - VIRUSES (Coxsackie B, enterovirus, influenza, CMV, EBV, HSV… Coxsackie A9 – self limiting disease; Coxsackie B3 – severe, sometimes lethal) - bacteria (Diphtheria, tbc, clostridia, staphylococci, -

Comparison of Echocardiography and Angiography in Determining the Cause of Severe Aortic Regurgitation
Br Heart J: first published as 10.1136/hrt.51.1.36 on 1 January 1984. Downloaded from Br Heart J 1984; 51: 36-45 Comparison of echocardiography and angiography in determining the cause of severe aortic regurgitation NICHOLAS L DEPACE, PASQUALE F NESTICO, MORRIS N KOTLER, GARY S MINTZ, DEMETRIOS KIMBIRIS, INDER P GOEL, E ELAINE GLAZIER-LASKEY, JOHN ROSS From the LikoffCardiovascular Institute, Hahnemann University, Philadelphia, Pennsylvania, USA SUMMARY To assess the accuracy of echocardiography in determining the cause of aortic regurgita- tion M mode and cross sectional echocardiography were compared with angiography in 43 patients with predominant aortic regurgitation. Each patient had all three investigations performed during the same admission to hospital. In each instance, the cause of aortic regurgitation was confirmed at surgery or necropsy. Seventeen patients had rheumatic aortic valve disease, 13 bacterial endocarditis with a perforated or partially destroyed cusp, five a biscuspid aortic valve (four with a history of endocarditis), and eight aortic regurgitation secondary to aortic root dilatation or aneurysm. Overall sensitivity of echocardiography and aortography was 84% in determining the cause of aortic regurgi- tation. Thus, rheumatic valve disease and endocarditis appear to be the most common causes of severe aortic regurgitation in this hospital based population. Furthermore, echocardiography is a sensitive non-invasive technique for determining the cause of aortic regurgitation and allows differentiation of valvular from root causes of aortic regurgitation. Aortic regurgitation may be caused by valvular dis- ment for predominant aortic regurgitation were http://heart.bmj.com/ ease, aortic root disease, or a combination of both. reviewed. -

The Challenge of Assessing Heart Valve Prostheses by Doppler Echocardiography
Editorial Comment The Challenge of Assessing Heart Valve Prostheses by Doppler Echocardiography Helmut Baumgartner, MD, Muenster, Germany The assessment of prosthetic valve function remains challenging. by continuous-wave Doppler measurement. Using these velocities Echocardiography has become the key diagnostic tool not only be- for the calculation of transvalvular gradients results in marked overes- cause of its noninvasive nature and wide availability but also because timation of the actual pressure drop across the prostheses.6 The fact of limitations inherent in alternative diagnostic techniques. Invasive that this phenomenon more or less disappears in malfunctioning bi- evaluation is limited particularly in mechanical valves that cannot leaflet prostheses when the funnel-shaped central flow channel ceases be crossed with a catheter, and in patients with both aortic and mitral to exist because of restricted leaflet motion makes the interpretation valve replacements, full hemodynamic assessment would even of Doppler data and their use for accurate detection of prosthesis mal- require left ventricular puncture. Although fluoroscopy and more function even more complicated.7 Furthermore, the lack of a flat ve- recently computed tomography allow the visualization of mechanical locity profile and the central high velocities described above cause valves and the motion of their occluders, the evaluation of prosthetic erroneous calculations of valve areas when the continuity equation valves typically relies on Doppler echocardiography. incorporates such measurements.8 For these reasons, the analysis of Although Doppler echocardiography has become an ideal nonin- occluder motion using fluoroscopy (in mitral prostheses, this may vasive technique for the evaluation of native heart valves and their also be obtained on transesophageal echocardiography) remains es- function, the assessment of prosthetic valves has remained more dif- sential to avoid the misinterpretation of high Doppler velocities across ficult. -

Thoracic Aorta
GUIDELINES AND STANDARDS Multimodality Imaging of Diseases of the Thoracic Aorta in Adults: From the American Society of Echocardiography and the European Association of Cardiovascular Imaging Endorsed by the Society of Cardiovascular Computed Tomography and Society for Cardiovascular Magnetic Resonance Steven A. Goldstein, MD, Co-Chair, Arturo Evangelista, MD, FESC, Co-Chair, Suhny Abbara, MD, Andrew Arai, MD, Federico M. Asch, MD, FASE, Luigi P. Badano, MD, PhD, FESC, Michael A. Bolen, MD, Heidi M. Connolly, MD, Hug Cuellar-Calabria, MD, Martin Czerny, MD, Richard B. Devereux, MD, Raimund A. Erbel, MD, FASE, FESC, Rossella Fattori, MD, Eric M. Isselbacher, MD, Joseph M. Lindsay, MD, Marti McCulloch, MBA, RDCS, FASE, Hector I. Michelena, MD, FASE, Christoph A. Nienaber, MD, FESC, Jae K. Oh, MD, FASE, Mauro Pepi, MD, FESC, Allen J. Taylor, MD, Jonathan W. Weinsaft, MD, Jose Luis Zamorano, MD, FESC, FASE, Contributing Editors: Harry Dietz, MD, Kim Eagle, MD, John Elefteriades, MD, Guillaume Jondeau, MD, PhD, FESC, Herve Rousseau, MD, PhD, and Marc Schepens, MD, Washington, District of Columbia; Barcelona and Madrid, Spain; Dallas and Houston, Texas; Bethesda and Baltimore, Maryland; Padua, Pesaro, and Milan, Italy; Cleveland, Ohio; Rochester, Minnesota; Zurich, Switzerland; New York, New York; Essen and Rostock, Germany; Boston, Massachusetts; Ann Arbor, Michigan; New Haven, Connecticut; Paris and Toulouse, France; and Brugge, Belgium (J Am Soc Echocardiogr 2015;28:119-82.) TABLE OF CONTENTS Preamble 121 B. How to Measure the Aorta 124 I. Anatomy and Physiology of the Aorta 121 1. Interface, Definitions, and Timing of Aortic Measure- A. The Normal Aorta and Reference Values 121 ments 124 1. -

Infective Endocarditis in Neonates
Arch Dis Child: first published as 10.1136/adc.63.1.53 on 1 January 1988. Downloaded from Archives of Disease in Childhood, 1988, 63, 53-57 Infective endocarditis in neonates C O'CALLAGHAN AND P MCDOUGALL Department of Neonatology, Royal Children's Hospital, Melbourne, Australia SUMMARY Five patients with neonatal infective endocarditis were reviewed, two of whom survived. Infection was caused by Staphylococcus aureus in four and by Candida albicans in one. All cases of bacterial endocarditis had clinical signs of septicaemia, positive blood cultures, thrombocytopenia, microscopic haematuria, and heart murmurs. Three developed skin abscesses early in their illnesses. Three patients had two dimensional echocardiographic studies that showed bacterial vegetations. One of these studies was done before the heart murmur could be heard. We suggest that echocardiography in conjunction with the clinical picture described may help in making an early diagnosis of endocarditis in neonates. Bacterial endocarditis in neonates is a rare and and tracheal aspirates; he was treated with intra- usually fatal disease; the first survivor was reported venous vancomycin. in 1983.1 2We became interested in the disease after At 26 days of age the baby had not improved and two patients in our neonatal unit survived. We a systolic murmur could be heard. Echocardio- therefore reviewed all five cases of neonatal infec- graphy showed vegetation round the mitral valve. tive endocarditis seen at this hospital over the past Despite the addition of fusidic acid to his treatment 10 years to see if we could find similarities that could he continued to deteriorate and died at 28 days. -
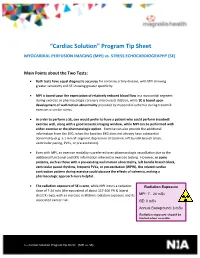
“Cardiac Solution” Program Tip Sheet
“Cardiac Solution” Program Tip Sheet MYOCARDIAL PERFUSION IMAGING (MPI) vs. STRESS ECHOCARDIOGRAPHY (SE) Main Points about the Two Tests: Both tests have equal diagnostic accuracy for coronary artery disease, with MPI showing greater sensitivity and SE showing greater specificity. MPI is based upon the expectation of relatively reduced blood flow in a myocardial segment during exercise or pharmacologic coronary microvessel dilation, while SE is based upon development of wall motion abnormality provoked by myocardial ischemia during treadmill exercise or similar stress. In order to perform a SE, one would prefer to have a patient who could perform treadmill exercise well, along with a good acoustic imaging window, while MPI can be performed with either exercise or the pharmacologic option. Exercise can also provide the additional information from the EKG, when the baseline EKG does not already have substantial abnormality (e.g. a 1 mm ST segment depression at baseline, left bundle branch block, ventricular pacing, PVCs, or pre-excitation). Even with MPI, an exercise modality is preferred over pharmacologic vasodilation due to the additional functional and EKG information inherent in exercise testing. However, in some patients, such as those with a pre-existing wall motion abnormality, left bundle branch block, ventricular paced rhythms, frequent PVCs, or pre-excitation (WPW), the related cardiac contraction pattern during exercise could obscure the effects of ischemia, making a pharmacologic approach more helpful. The radiation exposure of SE is zero, while MPI incurs a radiation Radiation Exposure dose of 7-24 mSv (the equivalent of about 117-400 PA & lateral chest X-rays), with an increase in lifetime radiation exposure and its MPI: 7 - 24 mSv associated cancer risk. -

2Nd Quarter 2001 Medicare Part a Bulletin
In This Issue... From the Intermediary Medical Director Medical Review Progressive Corrective Action ......................................................................... 3 General Information Medical Review Process Revision to Medical Record Requests ................................................ 5 General Coverage New CLIA Waived Tests ............................................................................................................. 8 Outpatient Hospital Services Correction to the Outpatient Services Fee Schedule ................................................................. 9 Skilled Nursing Facility Services Fee Schedule and Consolidated Billing for Skilled Nursing Facility (SNF) Services ............. 12 Fraud and Abuse Justice Recovers Record $1.5 Billion in Fraud Payments - Highest Ever for One Year Period ........................................................................................... 20 Bulletin Medical Policies Use of the American Medical Association’s (AMA’s) Current Procedural Terminology (CPT) Codes on Contractors’ Web Sites ................................................................................. 21 Outpatient Prospective Payment System January 2001 Update: Coding Information for Hospital Outpatient Prospective Payment System (OPPS) ......................................................................................................................... 93 he Medicare A Bulletin Providers Will Be Asked to Register Tshould be shared with all to Receive Medicare Bulletins and health care -

Transesophageal Echocardiographic Detection of Cardiac Embolic Source in Cor Triatriatum Complicated by Aortic Saddle Emboli
294 N. Cohen et al.: Brucellu endocarditis 4. Delvecchio G, Fracassetti 0, Lorenzi N: Brucellu endocarditis.fnt 15. Farid Z, Trabolsi B: Successful treatment of IWO cases of Br~rlltr J Curdiol1991 ;33:328-329 endocarditiswith rifampicin. BrMedJ 1985;29I : 1 10 5. Jeroudi MO, Halim MA, Harder EJ, Al-Sibai MB, Ziady G, 16. Al-Harthi SS: The morbidity and mortality pattern ofB~.~ccd/~ren- Mercer EN: Brucellu endocarditis.Br Heart J 1987;58:279-283 docarditis. Int J CurdiolI989:25:321-324 6. Fernandez-Guerrero ML: Zoonotic endocarditis. lnfect Dis Clin 17. Quinn RW, Brown JW Bacterial endocarditis. Arch hirm Md North Am 3993;7:135-1 52 1954;94:679684 7. Pazderka E, Jones JW: BruceNu abortus endocarditis: Successful 18. Micozzi A, Venditti M, Gentile G, Alessandii N, Santero M, Mar- treatment of an infected aortic valve. Arch Intern Med 1982;142: tino P: Successful treatment of Bvucelkc nic~/itrnsi.tendocarditis 1567- I568 with pefloxacin. EuvJ Clin Microhiollnjiw Di.v 1990;9:44W? 8. Valliattu J, Shuhaiber H, Kiwan Y, Araj G, Chugh T Brucellu en- 19. Al Mudallal DS, Mousa ARM, Marafie AA: Apyrcxic H~~rrc~c~lltr docarditis: Report of one case and review of the literature. J Cur- melitensis aortic valve endocarditis. Trop Gc~pMeti 1989i-l I : diovusc Surg 1989;30:782-785 372-376 9. Al-Kasab S, AI-Faghin MR, Al-Yousef S, Ali Khan MA, Ribeiro 20. Peery TM, Belter LF: Brucellosis and heart disease. Fatal hrucel- PA, Nazzal S, Al-Zaibag M: Brucellu infective endocarditis: Suc- losis: A review of the literature and repon of ncw cahes.