Antidiabetic Potential of Saffron and Its Active Constituents
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Abigail Marklew, Juha Kammonen, Emma Richardson & Jonathan
Development and validation of NMDA receptor ligand- gated ion channel assays using the Qube 384 automated electrophysiology platform Abigail Marklew, Juha Kammonen, Emma Richardson & Jonathan Mann Saffron Walden, Essex, UK Abigail Marklew, Juha Kammonen, Emma Richardson and Gary Clark Saffron1 ABSTRACT Walden, Essex, UK 2 MATERIALS AND METHODS Ligand-gated ion channels are of particular interest to the pharmaceutical industry for the Cell Culture: HEK-NMDA NR1/N2A receptor cells were produced at Charles River Laboratories and treatment of diseases from a variety of therapeutic areas including CNS disorders, respiratory are commercially available. All cells were grown according to their respective SOPs as developed by disease and chronic pain. Ligand-gated ion channels have historically been investigated using Charles River, except for the use of D-(-)-AP-5 as antagonist during induction. Cells were kept in a fluorescence-based and low throughput patch-clamp techniques. However the development of the serum-free medium in the cell hotel on the Qube instrument for up to 4 hours during experiment. Qube 384 automated patch-clamp system has allowed rapid exchange of liquid and direct Induction: Cells were induced 24 h prior to use using 1 µg/mL tetracycline and 100 µM D-(-)-AP-5 in measurement of ion channel currents on a millisecond timescale, making it possible to run HTS neurobasal medium + 10% dialysed FBS. campaigns and support SAR with a functional readout. Solutions: The following extracellular saline solution was used (mM): 145 NaCl. 4 KCl, 10 HEPES, 10 Glucose, 2 CaCl2, pH7.4. Intracellular solution (mM): 70 KCl, 70 KF, 10 HEPES, 1 EGTA, pH7.2. -
Investigation Into Potential Endocrine Disruptive Effects of Sceletium Tortuosum
Investigation into potential endocrine disruptive effects of Sceletium tortuosum by Letitia Louw Dissertation presented for the degree of Master of Science in the Faculty of Science at Stellenbosch University Supervisor: Prof C. Smith Co-supervisor: Prof AC. Swart March 2018 Stellenbosch University https://scholar.sun.ac.za Declaration By submitting this dissertation electronically, I declare that the entirety of the work contained therein is my own, original work, that I am the sole author thereof (save to the extent explicitly otherwise stated), that reproduction and publication thereof by Stellenbosch University will not infringe any third party rights and that I have not previously in its entirety or in part submitted it for obtaining any qualification. March 2018 Copyright © 2018 Stellenbosch University All rights reserved i Stellenbosch University https://scholar.sun.ac.za What if I fall? Oh, but darling what if you fly? ii Stellenbosch University https://scholar.sun.ac.za ABSTRACT Depression has been recognised by the World Health Organisation (WHO) as the leading cause of disability, affecting an estimated 300 million people globally. To date antidepressants are prescribed as the first step in the treatment strategy. However, finding the appropriate antidepressant is often a lengthy process and is usually accompanied by side effects. A major and often unexpected side effect is reduced sexual function, which has been reported to aggravate depression and could possibly lead to poor compliance to medication. Sceletium tortuosum is a native South African plant, which has exhibited both antidepressant and anxiolytic properties. Although the exact mechanism of action remains to be elucidated, there are currently two hypotheses which attempt to explain it’s mechanism of action. -

Jp Xvii the Japanese Pharmacopoeia
JP XVII THE JAPANESE PHARMACOPOEIA SEVENTEENTH EDITION Official from April 1, 2016 English Version THE MINISTRY OF HEALTH, LABOUR AND WELFARE Notice: This English Version of the Japanese Pharmacopoeia is published for the convenience of users unfamiliar with the Japanese language. When and if any discrepancy arises between the Japanese original and its English translation, the former is authentic. The Ministry of Health, Labour and Welfare Ministerial Notification No. 64 Pursuant to Paragraph 1, Article 41 of the Law on Securing Quality, Efficacy and Safety of Products including Pharmaceuticals and Medical Devices (Law No. 145, 1960), the Japanese Pharmacopoeia (Ministerial Notification No. 65, 2011), which has been established as follows*, shall be applied on April 1, 2016. However, in the case of drugs which are listed in the Pharmacopoeia (hereinafter referred to as ``previ- ous Pharmacopoeia'') [limited to those listed in the Japanese Pharmacopoeia whose standards are changed in accordance with this notification (hereinafter referred to as ``new Pharmacopoeia'')] and have been approved as of April 1, 2016 as prescribed under Paragraph 1, Article 14 of the same law [including drugs the Minister of Health, Labour and Welfare specifies (the Ministry of Health and Welfare Ministerial Notification No. 104, 1994) as of March 31, 2016 as those exempted from marketing approval pursuant to Paragraph 1, Article 14 of the Same Law (hereinafter referred to as ``drugs exempted from approval'')], the Name and Standards established in the previous Pharmacopoeia (limited to part of the Name and Standards for the drugs concerned) may be accepted to conform to the Name and Standards established in the new Pharmacopoeia before and on September 30, 2017. -

NMDA Receptor Antagonist Rodent Models for Cognition in Schizophrenia and Identification of Novel Drug Treatments, an Update
Neuropharmacology xxx (2017) 1e22 Contents lists available at ScienceDirect Neuropharmacology journal homepage: www.elsevier.com/locate/neuropharm Invited review NMDA receptor antagonist rodent models for cognition in schizophrenia and identification of novel drug treatments, an update Daniela Cadinu, Ben Grayson, Giovanni Podda, Michael K. Harte, Nazanin Doostdar, * Joanna C. Neill Division of Pharmacy and Optometry, School of Health Sciences, University of Manchester, Manchester, M13 9PT, UK article info abstract Article history: Negative and cognitive deficit symptoms in schizophrenia remain an unmet clinical need. Improved Received 31 August 2017 understanding of the neuro- and psychopathology of cognitive dysfunction in the illness is urgently Received in revised form required to enhance the development of new improved therapeutic strategies. Careful validation of 28 October 2017 animal models that mimic the behaviour and pathology of complex psychiatric disorders is an essential Accepted 27 November 2017 step towards this goal. Non-competitive NMDAR (N-Methyl-D-aspartate receptor) antagonists e.g. Available online xxx phencyclidine (PCP), ketamine and dizocilpine (MK-801) can effectively replicate certain aspects of negative and cognitive deficits associated with schizophrenia in animals. In 2010 we reviewed the effects Keywords: Cognition of NMDAR antagonism in tests for domains of cognition affected in schizophrenia, social behaviour and Schizophrenia neuropathology, and in 2014, in tests for negative symptoms. In this update, we -
The Effect of Aqueous Crocus Sativus L. Extract on Intracerebroventricular Streptozotocin-Induced Cognitive Deficits in Male
! )* +#, ('"#$#%& %" "(St ) ! (Ph D ) – (Ph D ) – (Ph D ) * " (St ) "(St ) #$#% $ ! "#$ : * najafabady @yahoo .com :&'()* + , !! / / : //: "#$ "B 6" + .( "& A * .*& 5>?@ - -2 + ( *68 9: 6; *+< =(% <* .67 5234 /01 .) .( "& - "()* + , "' & % & : .( "& A * - ."E + MN & L K 50 1 -) "E <* 5J 51& & "I* >? H ). ("& EA * - 5 "E F3G& 50 1 CD .1* ' 0I* . 5 *UB .) A "1+<001* .6; A?& 9I* T 6 <* 5' ."E + M N R S)7 & -*Q4< 5&8 34 L* 51& : P) D+ 9J' & Z1 + +* .)<+ 57 01* 5N*% 9(4 Y 5D ( g /kg ) A "1+<001* T 6 <* ( *68 V * .*& :) + + * Y <_ <* Q01* & 5 ] MN ^ "G\ + > "[ .<*0N* -<8 T D <* ."E + MN -*6 " + 5 *UB .) 6; .) A?& 9I* e " -*Q4< & - + STZ ch STZ cg -*Q4< & - + 0 7 c ( ACSF 7 ) e' cd 0 7 cb .) +E & `a .' 5& <* 9J' .) -<8 *+ jk1 H 7 5@QB 9I* 9J' & ( a mg /kg ) * -*Q4< 34 0Q) i & 5N*% <* S " <+ Y <* H '- +E . ' -<8 . ' 5 5& <* 5 ] MN -* "N ) -*6 " -* 4 & .*J "[ .) .+<& 7N B 9J' Y <_ -<8 . ' 5 ."E .0* "[ -<8 & .<*0N* -<8 .) * . ' 5 0E M * -* 4 & T"2? 1+ <* j Y & A'+ l* <* 24 "I i e) .<* 0N* -<8 m1 e) 9J' Y < -<8 .) * . ' 5 Q01* ) +E .*& 5 0 +cA -<8 -& * 5 > iB + 51& j"*+ cJ1+7 .' 5& <* -7J= + .?I + 0\ "& q "UB .) pG0 * H+* oN & ' - 5 "1+<001* .) & 2 -*Q4< 34 & ' - 5 "1+<001* .) :n 0 .<*0N* -<8 * A "1+<001* +E ."E + MN C "18 -* 6" * 5 > D & -*Q4< 34 +o4 & . * -\ 9J' Y <_ 0(7 .* S)7 > "[ & 94 + 7 5 V * .6; A?& 9I* A "1+<001* T 6 <* 5' MN S)7 <* ."E=% ."Q L* -*Q4< 34 5=7 D & :."E V "0 . -

Crocus Sativus L. Extracts and Its Constituents Crocins and Safranal; Potential Candidates for Schizophrenia Treatment?
molecules Review Crocus sativus L. Extracts and Its Constituents Crocins and Safranal; Potential Candidates for Schizophrenia Treatment? Nikolaos Pitsikas Department of Pharmacology, School of Medicine, Faculty of Health Sciences, University of Thessaly, Biopolis, Panepistimiou 3, 415-00 Larissa, Greece; [email protected]; Tel.: +30-2410-685-535 Abstract: Schizophrenia is a chronic mental devastating disease. Current therapy suffers from various limitations including low efficacy and serious side effects. Thus, there is an urgent necessity to develop new antipsychotics with higher efficacy and safety. The dried stigma of the plant Crocus sativus L., (CS) commonly known as saffron, are used in traditional medicine for various purposes. It has been demonstrated that saffron and its bioactive components crocins and safranal exert a beneficial action in different pathologies of the central nervous system such as anxiety, depression, epilepsy and memory problems. Recently, their role as potential antipsychotic agents is under investigation. In the present review, I intended to critically assess advances in research of these molecules for the treatment of schizophrenia, comment on their advantages over currently used neuroleptics as well-remaining challenges. Up to our days, few preclinical studies have been conducted to this end. In spite of it, results are encouraging and strongly corroborate that additional research is mandatory aiming to definitively establish a role for saffron and its bioactive components for the treatment of schizophrenia. Keywords: Crocus sativus L.; crocins; schizophrenia Citation: Pitsikas, N. Crocus sativus L. Extracts and Its Constituents Crocins and Safranal; Potential Candidates for 1. Schizophrenia Schizophrenia Treatment? Molecules Schizophrenia is a serious chronic mental disease that affects up to 1% of the world 2021, 26, 1237. -

Saffron: a Good Fit for New England
Saffron: A Good Fit for New England Margaret Skinner, Bruce L. Parker & Arash Ghalehgolabbehbahani North American Center for Saffron Research & Development University of Vermont What is Saffron? Crocus sativus (=cultivated) Stigma The most expensive spice in the world over $3,000-9,000/lb! Origin: Probably Greece or Crete Flowering: autumn Reproduction: Corm In cultivation for over 3,500 yr Stamen Why grow SAFFRON in the Northeast? Over 90% of farms in the Northeast are ranked as “Small”. 40 acres are lost to development every hour in the US. 42% of all developed land in the US is in the East. Crop diversification is key to success for small farms. What is Saffron good for? Culinary spice Medicinal herb Medicinal extract Perfume Ornamental plant Fabric dye Liqueur Where is Saffron Grown? Grown by Penn. Dutch as early as 1700s. Italy Spain Iran Tajikista n Morocco Greece India In 2016 the US imported 46 tons of saffron! Imports are estimated to triple by 2025. Why is Saffron so expensive? Currently most harvesting is done by hand. One acre (field-grown) in Iran produces about three pounds of saffron. Why is Saffron so expensive? Currently all processing is done by hand. 4,000 blooms = 1 oz of saffron Potential of Saffron for Diversified Farmers High value crop with long shelf live Low input (except harvesting & processing) Production is relatively simple Most labor outputs are for 4 weeks in Oct./Nov. Fits into traditional vegetable production cycle Lots of possible value-added products Saffron safes Saffron honey Saffron flavored oil Saffron flavored syrup Saffron Production Cycle Vegetative stage Dec. -

GROW YOUR OWN SAFFRON Saffron Spice Is Obtained from the Saffron Crocus (Crocus Sativus), a Large, Lavender, Fall-Blooming Crocu
GROW YOUR OWN SAFFRON By W allace P. Howell, W SU Benton-Franklin County Master Gardener. Revised October 1996 Saffron spice is obtained from the saffron crocus saffron, and have made a practice of giving the extras (Crocus sativus), a large, lavender, fall-blooming away to other gardeners, in batches of 40 or 50 bulbs. crocus, with three brilliant red stigmas. In the Tri- I dug my saffron bulbs this past summer after five Cities, C. sativus blooms about mid-October. The years in the ground, and found about 1,000. All stigmas need to be plucked from the blooms while except 150 were given away, and those 150 were they are still fresh. The most convenient way to pick immediately replanted. The bulbs should be planted them is with tweezers. After they have been picked, about two inches deep, like other crocus. They are they should be thoroughly air-dried, and stored in a quite hardy, and will go through winter temperatures tight spice bottle or vial until used. down to -15°F, or so, without injury. This type of crocus does not like to be in continuously wet ground. Saffron has been used since ancient times, both as a In fact, the bulbs will rot if planted in a swampy dye, and to flavor food. It lends a unique color and place, or in a garden where the ground has standing flavor to many foods prepared in countries around the water. I water mine occasionally during hot weather Mediterranean Sea. Saffron was introduced into (about every two weeks). -
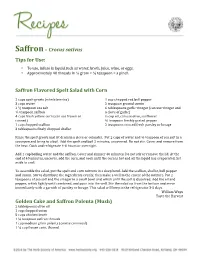
Saffron – Crocus Sativus Tips for Use
Saffron – Crocus sativus Tips for Use: • To use, infuse in liquid such as water, broth, juice, wine, or eggs. • Approximately 40 threads in ¼ gram = ½ teaspoon = a pinch Saffron Flavored Spelt Salad with Corn 2 cups spelt groats (whole berries) 1 cup chopped red bell pepper 3 cups water 2 teaspoon ground cumin 2 ½ teaspoon sea salt 6 tablespoons garlic vinegar (can use vinegar and ½ teaspoon saffron a clove of garlic) 4 cups fresh yellow corn (can use frozen or ⅔ cup oil, can use olive, sunflower canned) ¼ teaspoon freshly grated pepper 1 cup chopped scallion 2 teaspoons minced fresh parsley or lovage 3 tablespoons finely chopped shallot Rinse the spelt groats and let drain in a sieve or colander. Put 2 cups of water and ½ teaspoon of sea salt in a saucepan and bring to a boil. Add the spelt and boil 2 minutes, uncovered. Do not stir. Cover and remove from the heat. Cook and refrigerate 4-6 hours or overnight. Add 1 cup boiling water and the saffron. Cover and simmer 40 minutes. Do not stir or remove the lid. At the end of 40 minutes, uncover, add the corn, and cook until the corn is hot and all the liquid has evaporated. Set aside to cool. To assemble the salad, put the spelt and corn mixture in a deep bowl. Add the scallion, shallot, bell pepper and cumin. Stir to distribute the ingredients evenly, then make a well in the center of the mixture. Put 2 teaspoons of sea salt and the vinegar in a small bowl and whisk until the salt is dissolved. -

Constituents of Saffron (Crocus Sativus L.) As Potential Candidates for the Treatment of Anxiety Disorders and Schizophrenia
molecules Review Constituents of Saffron (Crocus sativus L.) as Potential Candidates for the Treatment of Anxiety Disorders and Schizophrenia Nikolaos Pitsikas Department of Pharmacology, School of Medicine, Faculty of Health Sciences, University of Thessaly, Panepistimiou 3 (Biopolis), Larissa 41500, Greece; [email protected]; Tel.: +30-2410-685-535 Academic Editors: Maria Z. Tsimidou and Petros A. Tarantilis Received: 8 December 2015 ; Accepted: 29 February 2016 ; Published: 2 March 2016 Abstract: Anxiety disorders and schizophrenia are common public health issues. The dried stigma of the plant Crocus sativus L., (C. sativus) commonly known as saffron are used in folk medicine for various purposes. Several lines of evidence suggest that C. sativus, crocins and safranal are implicated in anxiety and schizophrenia. Here, I intend to critically review advances in research of these emerging molecules for the treatment of anxiety and schizophrenia, discuss their advantages over currently used anxiolytics and neuroleptics, as well remaining challenges. Current analysis shows that C. sativus and its components might be a promising class of compounds for the treatment of the above mentioned psychiatric diseases. Keywords: Crocus sativus L.; anxiety; stress; schizophrenia 1. Introduction Crocus sativus L. (C. sativus), is a perennial herb member of the Iridaceae family, the line of Liliaceae. This plant is cultivated in many countries such as Azerbaijan, China, France, Greece, Egypt, India, Iran, Israel, Italy, Mexico, Morocco, Spain and Turkey. Its product is the well-known spice called saffron. Saffron, in filaments, is the dried dark-red stigmas of C. sativus flower [1]. One stigma of saffron weighs about 2 mg and each flower has three stigmata; 150,000 flowers must be carefully picked one by one to obtain 1 kg of spice. -

Supplement Ii to the Japanese Pharmacopoeia Seventeenth Edition
SUPPLEMENT II TO THE JAPANESE PHARMACOPOEIA SEVENTEENTH EDITION O‹cial from June 28, 2019 English Version THE MINISTRY OF HEALTH, LABOUR AND WELFARE Notice: This English Version of the Japanese Pharmacopoeia is published for the convenience of users unfamiliar with the Japanese language. When and if any discrepancy arises between the Japanese original and its English translation, the former is authentic. Printed in Japan The Ministry of Health, Labour and Welfare Ministerial Notification No. 49 Pursuant to Paragraph 1, Article 41 of Act on Securing Quality, Efficacy and Safety of Products Including Pharmaceuticals and Medical Devices (Act No. 145, 1960), this notification stated that a part of the Japanese Pharmacopoeia was revised as follows*. NEMOTO Takumi The Minister of Health, Labour and Welfare June 28, 2019 A part of the Japanese Pharmacopoeia (Ministerial Notification No. 64, 2016) was revised as follows*. (The text referred to by the term ``as follows'' are omitted here. All of the revised Japanese Pharmacopoeia in accordance with this notification (hereinafter referred to as ``new Pharmacopoeia'' in Supplement 2) are made available for public exhibition at the Pharmaceutical Evaluation Division, Pharmaceutical Safety and Environmen- tal Health Bureau, Ministry of Health, Labour and Welfare, at each Regional Bureau of Health and Welfare, and at each Prefectural Office in Japan). Supplementary Provisions (Effective Date) Article 1 This Notification is applied from June 28, 2019. (Transitional measures) Article 2 In the case of drugs which are listed in the Japanese Pharmacopoeia (hereinafter referred to as ``previous Pharmacopoeia'') [limited to those listed in new Pharmacopoeia] and drugs which have been approved as of June 28, 2019 as prescribed under Paragraph 1, Article 14 of Act on Securing Quality, Efficacy and Safety of Products Including Pharmaceuticals and Medical Devices [including drugs the Minister of Health, Labour and Welfare specifies (the Ministry of Health and Welfare Ministerial Notification No. -

The Effect of Aqueous Crocus Sativus L. Extract on Intracerebroventricular Streptozotocin-Induced Cognitive Deficits in Rat: a Behavioral Analysis
Iranian Journal of Pharmaceutical Research (2009), 8 (3): 185-191 Copyright © 2009 by School of Pharmacy Received: June 2008 Shaheed Beheshti University of Medical Sciences and Health Services Accepted: February 2009 Original Article The Effect of Aqueous Crocus sativus L. Extract on Intracerebroventricular Streptozotocin-induced Cognitive Deficits in Rat: a Behavioral Analysis Mohsen Khalili a*, Mehrdad Roghania and Majid Ekhlasib aDepartment of Physiology, School of Medicine and Medicinal Plant and Neuroscience Research Center, Shahed University of Medical Sciences, Tehran, Iran. bDepartment of Physiology, School of Medicine, Shahed University, Tehran, Iran. Abstract Intracerebroventricular (ICV) injection of streptozotocin (STZ) causes cognitive impairment in rats. The beneficial effect of Crocus sativus L. extract (CSE) was evaluated on ICV STZ-induced learning, memory, and cognitive impairment in male rats. For this purpose, rats were injected with ICV STZ bilaterally, on days 1 and 3 (3 mg/kg). The STZ-injected rats received CSE (60 mg/kg; i.p.) every other day, starting one day before surgery, for three weeks. The learning and memory performance was assessed using passive avoidance paradigm, and for spatial cognition evaluation, Y-maze task was used. It was found that CSE-treated STZ- injected rats show higher correct choices and lower errors in Y maze than vehicle-treated STZ- injected rats. In addition, CSE administration significantly attenuated learning and memory impairment in treated STZ-injected group in passive avoidance test. Therefore, these results demonstrate the effectiveness of CSE in preventing the cognitive deficits caused by ICV STZ in rats and its potential in the treatment of neurodegenerative diseases such as Alzheimer’s disease (AD).