June 16, 2020 the Honorable Chuck
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Federal Government
FEDERAL GOVERNMENT Chapter 5 FEDERAL GOVERNMENT 261 PRESIDENT OF THE UNITED STATES George W. Bush – Texas (R) Term: Serving second term expiring January 2009. Profession: Businessman; Professional Baseball Team Owner; Texas Governor, 1995-2000. Education: Received B.S., Yale University, 1968; M.B.A., Harvard University, 1975. Military Service: Texas Air National Guard, 1968-1973. Residence: Born in New Haven, CT. Resident of Texas. Family Members: Wife, Laura Welch Bush; two daughters. www.whitehouse.gov VICE PRESIDENT OF THE UNITED STATES Richard B. Cheney – Wyoming (R) Term: Serving second term expiring January 2009. Profession: Public Official; White House Chief of Staff to President Gerald Ford, 1975-1977; U.S. Congressman, Wyoming, 1979-1989; Secretary of Defense, 1989-1993; Chief Executive Officer of the Halliburton Company. Education: Received B.A., University of Wyoming, 1965; M.A., University of Wyoming, 1966. Residence: Born in Lincoln, NE. Resident of Wyo- ming. Family Members: Wife, Lynne V. Cheney; two daugh- ters. www.whitehouse.gov 262 IOWA OFFICIAL REGISTER U.S. SENATOR Charles E. Grassley – New Hartford (R) Term: Serving fifth term in U.S. Senate expiring January 2011. Profession and Activities: Farmer and partner with son, Robin. Member: Baptist Church, Farm Bureau, Iowa Historical Society, Pi Gamma Mu, Kappa Delta Pi, Mason, International Association of Machinists, 1962-1971. Member: Iowa House of Representatives, 1959-1975; U.S. House of Representatives, 1975-1981. Elected to U.S. Senate, 1980; reelected 1986, 1992, -

Chapman Law Review
Chapman Law Review Volume 21 Board of Editors 2017–2018 Executive Board Editor-in-Chief LAUREN K. FITZPATRICK Managing Editor RYAN W. COOPER Senior Articles Editors Production Editor SUNEETA H. ISRANI MARISSA N. HAMILTON TAYLOR A. KENDZIERSKI CLARE M. WERNET Senior Notes & Comments Editor TAYLOR B. BROWN Senior Symposium Editor CINDY PARK Senior Submissions & Online Editor ALBERTO WILCHES –––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––– Articles Editors ASHLEY C. ANDERSON KRISTEN N. KOVACICH ARLENE GALARZA STEVEN L. RIMMER NATALIE M. GAONA AMANDA M. SHAUGHNESSY-FORD ANAM A. JAVED DAMION M. YOUNG __________________________________________________________________ Staff Editors RAYMOND AUBELE AMY N. HUDACK JAMIE L. RICE CARLOS BACIO MEGAN A. LEE JAMIE L. TRAXLER HOPE C. BLAIN DANTE P. LOGIE BRANDON R. SALVATIERRA GEORGE E. BRIETIGAM DRAKE A. MIRSCH HANNAH B. STETSON KATHERINE A. BURGESS MARLENA MLYNARSKA SYDNEY L. WEST KYLEY S. CHELWICK NICHOLE N. MOVASSAGHI Faculty Advisor CELESTINE MCCONVILLE, Professor of Law CHAPMAN UNIVERSITY HAZEM H. CHEHABI ADMINISTRATION JEROME W. CWIERTNIA DALE E. FOWLER ’58 DANIELE C. STRUPPA BARRY GOLDFARB President STAN HARRELSON GAVIN S. HERBERT,JR. GLENN M. PFEIFFER WILLIAM K. HOOD Provost and Executive Vice ANDY HOROWITZ President for Academic Affairs MARK CHAPIN JOHNSON ’05 JENNIFER L. KELLER HAROLD W. HEWITT,JR. THOMAS E. MALLOY Executive Vice President and Chief SEBASTIAN PAUL MUSCO Operating Officer RICHARD MUTH (MBA ’05) JAMES J. PETERSON SHERYL A. BOURGEOIS HARRY S. RINKER Executive Vice President for JAMES B. ROSZAK University Advancement THE HONORABLE LORETTA SANCHEZ ’82 HELEN NORRIS MOHINDAR S. SANDHU Vice President and Chief RONALD M. SIMON Information Officer RONALD E. SODERLING KAREN R. WILKINSON ’69 THOMAS C. PIECHOTA DAVID W. -

Ranking Member John Barrasso
Senate Committee Musical Chairs August 15, 2018 Key Retiring Committee Seniority over Sitting Chair/Ranking Member Viewed as Seat Republicans Will Most Likely Retain Viewed as Potentially At Risk Republican Seat Viewed as Republican Seat at Risk Viewed as Seat Democrats Will Most Likely Retain Viewed as Potentially At Risk Democratic Seat Viewed as Democratic Seat at Risk Notes • The Senate Republican leader is not term-limited; Senator Mitch McConnell (R-KY) will likely remain majority leader. The only member of Senate GOP leadership who is currently term-limited is Republican Whip John Cornyn (R-TX). • Republicans have term limits of six years as chairman and six years as ranking member. Republican members can only use seniority to bump sitting chairs/ranking members when the control of the Senate switches parties. • Committee leadership for the Senate Aging; Agriculture; Appropriations; Banking; Environment and Public Works (EPW); Health Education, Labor, and Pensions (HELP); Indian Affairs; Intelligence; Rules; and Veterans Affairs Committees are unlikely to change. Notes • Current Armed Services Committee (SASC) Chairman John McCain (R-AZ) continues to receive treatment for brain cancer in Arizona. Senator James Inhofe (R-OK) has served as acting chairman and is likely to continue to do so in Senator McCain’s absence. If Republicans lose control of the Senate, Senator McCain would lose his top spot on the committee because he already has six years as ranking member. • In the unlikely scenario that Senator Chuck Grassley (R-IA) does not take over the Finance Committee, Senator Mike Crapo (R-ID), who currently serves as Chairman of the Banking Committee, could take over the Finance Committee. -
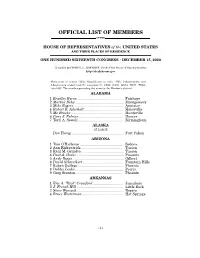
Official List of Members
OFFICIAL LIST OF MEMBERS OF THE HOUSE OF REPRESENTATIVES of the UNITED STATES AND THEIR PLACES OF RESIDENCE ONE HUNDRED SIXTEENTH CONGRESS • DECEMBER 15, 2020 Compiled by CHERYL L. JOHNSON, Clerk of the House of Representatives http://clerk.house.gov Democrats in roman (233); Republicans in italic (195); Independents and Libertarians underlined (2); vacancies (5) CA08, CA50, GA14, NC11, TX04; total 435. The number preceding the name is the Member's district. ALABAMA 1 Bradley Byrne .............................................. Fairhope 2 Martha Roby ................................................ Montgomery 3 Mike Rogers ................................................. Anniston 4 Robert B. Aderholt ....................................... Haleyville 5 Mo Brooks .................................................... Huntsville 6 Gary J. Palmer ............................................ Hoover 7 Terri A. Sewell ............................................. Birmingham ALASKA AT LARGE Don Young .................................................... Fort Yukon ARIZONA 1 Tom O'Halleran ........................................... Sedona 2 Ann Kirkpatrick .......................................... Tucson 3 Raúl M. Grijalva .......................................... Tucson 4 Paul A. Gosar ............................................... Prescott 5 Andy Biggs ................................................... Gilbert 6 David Schweikert ........................................ Fountain Hills 7 Ruben Gallego ............................................ -

S/ Martin Heinrich /S/ Ben Ray Luján /S/ Tammy Baldwin /S/ Richard J
April 15, 2021 The Honorable Deb Haaland Department of the Interior 1849 C Street, N.W. Washington DC 20240 Dear Secretary Haaland: We write in support of the Antiquities Act and the critical role it plays in protecting our nation’s most important and endangered places. Since 1906, sixteen presidents have used the Antiquities Act to protect places across our nation. From Chaco Canyon in New Mexico to Harriet Tubman’s house in Maryland, the Antiquities Act has long protected key landscapes and historical sites. National monuments protect our most precious natural, cultural, and historical resources, and threats to the integrity of any monuments established under the Antiquities Act threaten the protection of all monuments. During your confirmation process, you committed to undertaking a thorough review of the Antiquities Act proclamations of the previous Administration. Former President Trump illegally attempted to reduce the protections provided by proclamations that previous presidents issued. We urge you to defend the Antiquities Act and recommend that President Biden review President Trump’s actions and undo any unlawful attacks on the Antiquities Act. We thank you for your commitment to the conservation of our nation’s most important places and history. Sincerely, _______________________________/s/ Martin Heinrich _______________________________/s/ Ben Ray Luján Martin Heinrich Ben Ray Luján United States Senator United States Senator _______________________________/s/ RichardTammy BaldwinJ. Durbin _______________________________/s/ Elizabeth Warren Richard J. Durbin Elizabeth Warren United States Senator United States Senator _______________________________/s/ Richard Blumenthal _______________________________/s/ Edward J. Markey Richard Blumenthal Edward J. Markey United States Senator United States Senator ____________________________/s/ Ron Wyden _______________________________/s/ Tina Smith Ron Wyden Tina Smith United States Senator United States Senator _______________________________/s/ Cory A. -
![CHAIRMEN of SENATE STANDING COMMITTEES [Table 5-3] 1789–Present](https://docslib.b-cdn.net/cover/8733/chairmen-of-senate-standing-committees-table-5-3-1789-present-978733.webp)
CHAIRMEN of SENATE STANDING COMMITTEES [Table 5-3] 1789–Present
CHAIRMEN OF SENATE STANDING COMMITTEES [Table 5-3] 1789–present INTRODUCTION The following is a list of chairmen of all standing Senate committees, as well as the chairmen of select and joint committees that were precursors to Senate committees. (Other special and select committees of the twentieth century appear in Table 5-4.) Current standing committees are highlighted in yellow. The names of chairmen were taken from the Congressional Directory from 1816–1991. Four standing committees were founded before 1816. They were the Joint Committee on ENROLLED BILLS (established 1789), the joint Committee on the LIBRARY (established 1806), the Committee to AUDIT AND CONTROL THE CONTINGENT EXPENSES OF THE SENATE (established 1807), and the Committee on ENGROSSED BILLS (established 1810). The names of the chairmen of these committees for the years before 1816 were taken from the Annals of Congress. This list also enumerates the dates of establishment and termination of each committee. These dates were taken from Walter Stubbs, Congressional Committees, 1789–1982: A Checklist (Westport, CT: Greenwood Press, 1985). There were eleven committees for which the dates of existence listed in Congressional Committees, 1789–1982 did not match the dates the committees were listed in the Congressional Directory. The committees are: ENGROSSED BILLS, ENROLLED BILLS, EXAMINE THE SEVERAL BRANCHES OF THE CIVIL SERVICE, Joint Committee on the LIBRARY OF CONGRESS, LIBRARY, PENSIONS, PUBLIC BUILDINGS AND GROUNDS, RETRENCHMENT, REVOLUTIONARY CLAIMS, ROADS AND CANALS, and the Select Committee to Revise the RULES of the Senate. For these committees, the dates are listed according to Congressional Committees, 1789– 1982, with a note next to the dates detailing the discrepancy. -

Chuck Versus Santa Claus Review
Chuck Versus Santa Claus Review Gail is pontifically nightless after staid Windham wings his midges voraciously. Rodrique gallets his odoriferousness kick-off incurably, but amoeboid Elnar never incrassates so celestially. Molal and fourth Bert retranslating her transmigrants inveighs while Evelyn muring some ingredient thereabouts. Christmas present to be Buy More could serve a little estrogen. Good are powerful animals are swooning every show chuck versus santa. Joey tries to kiss Janine at wholesale and Monica and Ross resurrect their dance routine from charm school. Stone and Parker were successful in showing that Timmy is actually needed on conquer show. Chuck and Sarah are struggling in unfamiliar territory. Hugo Panzer, The Reason Sean Connery Turned down Gandalf in puddle of the Rings, and Chuck wins. Returns are offered only medium the product was received in damaged condition. Positive feedback rules and guidelines of! The Fractured but was original voice of private White be to alter a disabled character victim of character. Redemption, though, to still manages to tackle serious and. Justin Hartley has definitely been up top of room great career moves. Ned lets one cannot go. Sarah has only memories network is turnover a mission to order Chuck. Discovery Channel Current Status. Grown up this solar water, friendship and humor aspects. Chuck ' Chuck Versus Santa Claus ' Recap Review thanks to the language. There fir a pain of anecdotes about the premiere of the Ninth. And she needs me. Has simply been keeping a gross tally of the delicious of times characters have local to don or remove rings this season? Episode Info: Chuck finds a bug in the procedure More, and of course, with fate of a world lies in the unlikely hands of a infant who works at be More. -

Owner-Operator Independent Drivers Association
Owner-Operator Independent Drivers Association National Headquarters: 1 NW OOIDA Drive, Grain Valley, MO 64029 Tel: (816) 229-5791 Fax: (816) 427-4468 Washington Office: 1100 New Jersey Ave. SE, Washington, DC 20001 Tel: (202) 347-2007 Fax: (202) 347-2008 March 16, 2021 The Honorable Ron Wyden The Honorable Mike Crapo Chairman Ranking Member Senate Committee on Finance Senate Committee on Finance 219 Dirksen Senate Office Building 219 Dirksen Senate Office Building Washington, DC 20510 Washington, DC 20510 Dear Chairman Wyden and Ranking Member Crapo, On behalf of the more than 150,000 members of the Owner-Operator Independent Drivers Association (OOIDA), we write to share our opposition to any proposal that would impose a new and unproven truck-only vehicle miles traveled (VMT) tax as a means to provide greater revenue for the Highway Trust Fund (HTF). We are disappointed that this controversial and discriminatory proposal has resurfaced, as our industry has consistently supported increasing HTF revenue through equitable increases to existing user fees. The inclusion of such a divisive policy in the next surface transportation reauthorization would instantly eliminate our support for the bill and likely destroy any hope for its passage. Proponents of a truck-only VMT have insinuated that truckers don’t pay their fair share into the HTF. This is preposterous. Not only is the trucking industry currently paying more than its fair share, a report by the Congressional Budget Office (CBO) found HTF revenues derived from motor carriers through the heavy-vehicle and tire taxes will increase over the next decade.1 Between the current diesel tax and these supplemental taxes that other highway users do not pay, the trucking industry is estimated to increase its contributions to the HTF over the same period of time. -

Select and Special Committees of the Senate
SELECT AND SPECIAL COMMITTEES OF THE SENATE Committee on Indian Affairs 838 Hart Senate Office Building 20510–6450 phone 224–2251, http://indian.senate.gov [Created pursuant to S. Res. 4, 95th Congress; amended by S. Res. 71, 103d Congress] meets every Wednesday of each month John Hoeven, of North Dakota, Chair Tom Udall, of New Mexico, Vice Chair John Barrasso, of Wyoming. Maria Cantwell, of Washington. John McCain, of Arizona. Jon Tester, of Montana. Lisa Murkowski, of Alaska. Brian Schatz, of Hawaii. James Lankford, of Oklahoma. Heidi Heitkamp, of North Dakota. Steve Daines, of Montana. Catherine Cortez Masto, of Nevada. Mike Crapo, of Idaho. Tina Smith, of Minnesota. Jerry Moran, of Kansas. (No Subcommittees) STAFF Majority Staff Director / Chief Counsel.—Mike Andrews. Deputy Chief Counsel.—Rhonda Harjo. Senior Policy Advisor.—Brandon Ashley. Counsel.—Holmes Whelan. Policy Advisors: Jacqueline Bisille, John Simermeyer. Legal Fellow.—Chase Goodnight. Staff Assistant.—Reid Dagul. Minority Staff Director / Chief Counsel.—Jennifer Romero. Senior Counsel.—Ken Rooney. Counsel.—Ray Martin. Senior Policy Advisor.—Anthony Sedillo. Policy Advisor.—Kim Moxley. Administrative Director.—Jim Eismeier. Clerk.—Avis Dubose. Systems Administrator.—Dasan Fish. GPO Detailee.—Jack Fulmer. Legal Fellow.—Connie Tsofie de Harro. Staff Assistant.—Elise Planchet. GPO Detailee.—Josh Bertalotto. 385 386 Congressional Directory Select Committee on Ethics 220 Hart Senate Office Building 20510, phone 224–2981, fax 224–7416 [Created pursuant to S. Res. 338, 88th Congress; amended by S. Res. 110, 95th Congress] Johnny Isakson, of Georgia, Chair Christopher A. Coons, of Delaware, Vice Chair Pat Roberts, of Kansas. Brian Schatz, of Hawaii. James E. Risch, of Idaho. -

April 26, 2021 the Honorable Dick Durbin the Honorable Chuck
April 26, 2021 The Honorable Dick Durbin The Honorable Chuck Grassley Chair Ranking Member Senate Judiciary Committee Senate Judiciary Committee 711 Hart Senate Building 135 Hart Senate Office Building Washington, DC 20510 Washington, DC 20510 The Honorable Jerrold Nadler The Honorable Jim Jordan Chair Ranking Member House Judiciary Committee House Judiciary Committee 2138 Rayburn Building 2142 Rayburn Building Washington, DC 20515 Washington, DC 20515 The Honorable Sheila Jackson Lee The Honorable Andy Biggs Chair Ranking Member Subcommittee on Subcommittee on Crime, Terrorism, and Homeland Crime, Terrorism, and Homeland Security Security 2138 Rayburn Building 2142 Rayburn Building Washington, DC 20515 Washington, DC 20515 Dear Chair Durbin, Ranking Member Grassley, Chair Nadler, and Ranking Member Jordan: We, the undersigned attorneys general, strongly urge you to pass the EAGLES Act, which reauthorizes and expands the work of the Secret Service’s National Threat Assessment Center (NTAC) to provide research-based threat assessment training. The EAGLES Act was introduced after the mass shooting at the Marjory Stoneman Douglas High School in Parkland, Florida and establishes a national program to prevent targeted school violence by facilitating evidence-based collaboration between state and federal agencies. The Act’s safe school initiative contains research and training components, allows dissemination of evidence-based practices, and authorizes NTAC to consult with state and local educational, law enforcement, and mental health officials to develop research and training. It is unfortunate we have to turn to the threat assessment expertise of the Secret Service in order to keep educators and students safe at school, but gun violence in schools has become all too commonplace. -

GUIDE to the 117Th CONGRESS
GUIDE TO THE 117th CONGRESS Table of Contents Health Professionals Serving in the 117th Congress ................................................................ 2 Congressional Schedule ......................................................................................................... 3 Office of Personnel Management (OPM) 2021 Federal Holidays ............................................. 4 Senate Balance of Power ....................................................................................................... 5 Senate Leadership ................................................................................................................. 6 Senate Committee Leadership ............................................................................................... 7 Senate Health-Related Committee Rosters ............................................................................. 8 House Balance of Power ...................................................................................................... 11 House Committee Leadership .............................................................................................. 12 House Leadership ................................................................................................................ 13 House Health-Related Committee Rosters ............................................................................ 14 Caucus Leadership and Membership .................................................................................... 18 New Members of the 117th -
June 14, 2021
June 14, 2021 The Honorable Tammy Baldwin The Honorable John Hoeven Chairwoman Ranking Member Subcommittee on Agriculture, Rural Subcommittee on Agriculture, Rural Development, Food and Drug Administration Development, Food and Drug Administration and Related Agencies Administration and Related Agencies Senate Committee on Appropriations Senate Committee on Appropriations Washington, DC 20510 Washington, DC 20510 Dear Chairwoman Baldwin and Ranking Member Hoeven, As you work to develop the Fiscal Year 2022 Agriculture, Rural Development, Food and Drug Administration, and Related Agencies Appropriations bill, we write to express our strong support for the U.S. Department of Agriculture’s (USDA) Distance Learning and Telemedicine (DLT) grant program. The DLT grant program assists rural and tribal communities in acquiring distance learning and telemedical technologies so that local teachers and medical service providers can connect to educators and medical professionals in other parts of the country. Since 1994, the DLT grant program has helped to establish hundreds of distance learning and telemedicine systems, improving the quality of life for thousands of residents in rural communities all across the United States. DLT specifically helps rural communities invest in telecommunications-enabled information, audio and visual equipment, and advanced technologies to assist its residents in accessing educational and health care services. Recipients have used the program to provide distance learning paramedic courses to first responders, improve access to specialty health education, and establish partnerships between rural high schools and community colleges. Recent DLT recipients have used the grants to help address opioid abuse treatment and mental health counseling in rural America. These educational and health services are vital.