Incidence and Method of Suicide in Hospitals in the United States
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Association Between Suicide Reporting in the Media and Suicide: Systematic Review and Meta-Analysis
BMJ 2020;368:m575 doi: 10.1136/bmj.m575 (Published 18 March 2020) Page 1 of 17 Research BMJ: first published as 10.1136/bmj.m575 on 18 March 2020. Downloaded from RESEARCH Association between suicide reporting in the media and suicide: systematic review and meta-analysis OPEN ACCESS Thomas Niederkrotenthaler associate professor 1 2, Marlies Braun postgraduate researcher 1 2, Jane Pirkis professor 3, Benedikt Till associate professor 1 2, Steven Stack professor 4, Mark Sinyor associate professor 5 6, Ulrich S Tran senior lecturer 2 7, Martin Voracek professor 2 7, Qijin Cheng assistant professor 8, Florian Arendt assistant professor 2 9, Sebastian Scherr assistant professor 10, Paul S F Yip professor 11, Matthew J Spittal associate professor 3 1Unit Suicide Research and Mental Health Promotion, Department of Social and Preventive Medicine, Centre for Public Health, Medical University of Vienna, Kinderspitalgasse 15, A-1090 Vienna, Austria; 2Wiener Werkstaette for Suicide Research, Vienna, Austria; 3Centre for Mental Health, Melbourne School of Population and Global Health, University of Melbourne, Melbourne, VIC, Australia; 4Department of Criminology and Department of Psychiatry, Wayne State University, Detroit, MI, USA; 5Department of Psychiatry, Sunnybrook Health Sciences Centre, Toronto, ON, Canada; 6Department of Psychiatry, University of Toronto, Toronto, ON, Canada; 7Department of Basic Psychological Research and Research Methods, http://www.bmj.com/ School of Psychology, University of Vienna, Vienna, Austria; 8Department of Social Work, Chinese University of Hong Kong, Hong Kong, China; 9Department of Communication, University of Vienna, Vienna, Austria; 10School for Mass Communication Research, KU Leuven, Leuven, Belgium; 11Centre for Suicide Research and Prevention, and Department of Social Work and Social Administration, University of Hong Kong, Hong Kong, China Abstract 1-8 days) for a one article increase in the number of reports on suicide. -

A 10-Year Ecological Study of the Methods of Suicide Used by Brazilian Adolescents
ARTIGO ARTICLE A 10-year ecological study of the methods of suicide used by Brazilian adolescents Estudo ecológico de 10 anos sobre os métodos de suicídio usados por adolescentes brasileiros Estudio ecológico abarcando 10 años sobre los métodos de suicidio practicados por Denisse Claudia Jaen-Varas 1 adolescentes brasileños Jair J. Mari 1,2 Elson Asevedo 1,3 Rohan Borschmann 4,5 Elton Diniz 1 Carolina Ziebold 1,2 Ary Gadelha 1,2 doi: 10.1590/0102-311X00104619 Abstract Correspondence D. C. Jaen-Varas Universidade Federal de São Paulo. Suicide among adolescents has become a major public health problem world- Rua Major Maragliano 241, São Paulo, SP 04017-030, Brasil. wide. Our study sought to describe the most commonly used methods of sui- [email protected] cide among adolescents aged 10 to 19 years in Brazil between 2006 and 2015. Complete data were obtained from the Brazilian Health Informatics Depart- 1 Universidade Federal de São Paulo, São Paulo, Brasil. 2 ment (DATASUS) and coded into seven categories of suicide methods. The fol- Instituto Nacional de Psiquiatria do Desenvolvimento para Crianças e Adolescentes, São Paulo, Brasil. 2 lowing statistical analyzes were performed: chi-square (χ ) tests to examine 3 Global Mental Health Program, Columbia University, New the association between the frequency of each suicide method and the year; York, U.S.A. odds ratios (OR) and 95% confidence intervals (95%CI) compared the rela- 4 Melbourne School of Psychological Sciences; University of tive chances of each suicide method occurring between boys and girls. In total, Melbourne, Melbourne, Australia. 5 Centre for Adolescent Health, Murdoch Children’s Research 8,026 suicides among Brazilian adolescents were registered over the analyzed Institute, Melbourne, Australia. -

Preventing Suicide: a Global Imperative
PreventingPreventing suicidesuicide A globalglobal imperativeimperative PreventingPreventing suicidesuicide A globalglobal imperativeimperative WHO Library Cataloguing-in-Publication Data Preventing suicide: a global imperative. 1.Suicide, Attempted. 2.Suicide - prevention and control. 3.Suicidal Ideation. 4.National Health Programs. I.World Health Organization. ISBN 978 92 4 156477 9 (NLM classification: HV 6545) © World Health Organization 2014 All rights reserved. Publications of the World Health Organization are The mention of specific companies or of certain manufacturers’ available on the WHO website (www.who.int) or can be purchased products does not imply that they are endorsed or recommended by from WHO Press, World Health Organization, 20 Avenue Appia, the World Health Organization in preference to others of a similar 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 nature that are not mentioned. Errors and omissions excepted, the 4857; e-mail: [email protected]). names of proprietary products are distinguished by initial capital letters. Requests for permission to reproduce or translate WHO publications –whether for sale or for non-commercial distribution– should be All reasonable precautions have been taken by the World Health addressed to WHO Press through the WHO website Organization to verify the information contained in this publication. (www.who.int/about/licensing/copyright_form/en/index.html). However, the published material is being distributed without warranty of any kind, either expressed or implied. The responsibility The designations employed and the presentation of the material in for the interpretation and use of the material lies with the reader. In this publication do not imply the expression of any opinion no event shall the World Health Organization be liable for damages whatsoever on the part of the World Health Organization concerning arising from its use. -
Suicide Methods in Virginia: Patterns by Race, Gender, Age, and Birthplace a Report from the Virginia Violent Death Reporting System
Suicide Methods in Virginia: Patterns by Race, Gender, Age, and Birthplace A Report from the Virginia Violent Death Reporting System 2003-2008 Commonwealth of Virginia Virginia Department of Health Office of the Chief Medical Examiner April, 2011 Suicide Methods in Virginia: Patterns by Race, Gender, Age, and Birthplace A Report from the Virginia Violent Death Reporting System 2003-2008 Published April, 2011 by Marc E. Leslie, MS VVDRS Coordinator (804) 205-3855 [email protected] Surveillance Coordinators: Richmond Baker Debra A. Clark Tidewater District Central District Rachael M. Luna Jennifer P. Burns Western District Northern District Project Manager: Virginia Powell, PhD VVDRS Principal Investigator Suggested citation : Virginia Violent Death Reporting System (VVDRS), Office of the Chief Medical Examiner, Virginia Department of Health. Suicide Methods in Virginia: Patterns by Race, Gender, Age, and Birthplace (2003-2008) . April, 2011. The research files for this report were created on November 9, 2010. Data may continue to be entered and altered in VVDRS after this date. The publication was supported by Award Number U17/CE001315 from the Centers for Disease Control and Prevention. Its contents are solely the responsibility of the author and do not necessarily represent the official views of the Centers for Disease Control and Prevention. Virginia Department of Health, Office of the Chief Medical Examiner i Acknowledgements This report is possible through the support and efforts of those who generously contribute their time and expertise to the VVDRS. We gratefully acknowledge the ongoing contributions of our Forensic Pathologists and Pathology Fellows whose expertise adds depth to our knowledge. We acknowledge the contributions of the OCME State and District Administrators who support the project’s human resources requirements. -

ENGAGE LETHAL.Pdf
ENGAGE Engage: Reducing Access to Lethal Means Reducing access to lethal means is an essential step in safety planning. Overview: Reducing Access to Lethal Means Works A key component of Zero Suicide and other effective suicide prevention strategies is reducing access to methods that could be used for suicidal acts and, if possible, restricting access during an acute suicidal crisis. Reducing ac- cess to lethal means—particularly those with greater lethality—is essential in safety planning. Studies around the world have demonstrated that the overall rate of suicide drops when access to commonly-used, highly lethal suicide methods is reduced.1,2,3 In the late 1950s, the United Kingdom switched from coal gas to natural gas, which is free from carbon monoxide.1 Suicide deaths decreased, saving thousands of lives over the next 10 years. A study in Australia found a decrease in suicide by firearms and in the overall national suicide rate following a 1998 ban on private gun ownership.3 Every safety plan should address reducing access to any lethal means that are available to the patient. Limiting ac- cess to medications and chemicals and removing or securing firearms, other weapons, and ligatures are important actions to keep patients safe. This is particularly important in light of findings about the impulsivity of many suicide attempts. Among people who made near-lethal suicide attempts, 24 percent reported taking less than five minutes between the decision to kill themselves and the actual attempt. 70 percent took less than an hour.4 Based on this evidence, it is clearly possible to increase the chance of surviving an attempt if an individual at risk for suicide has reduced access to lethal means in their moment of crisis. -

The Most Common Method of Suicide in Tehran 2000–2004
See discussions, stats, and author profiles for this publication at: https://www.researchgate.net/publication/23182135 The Most Common Method of Suicide in Tehran 2000–2004 Article in Crisis The Journal of Crisis Intervention and Suicide Prevention · February 2008 DOI: 10.1027/0227-5910.29.3.164 · Source: PubMed CITATIONS READS 7 69 4 authors, including: Mohsen Rezaeian Rafsanjan University of Medical Sciences 240 PUBLICATIONS 1,176 CITATIONS SEE PROFILE Some of the authors of this publication are also working on these related projects: Suicide Mortality in Kermanshah Province View project nasal carriage of s. aureus among health workers in Iran View project All content following this page was uploaded by Mohsen Rezaeian on 11 December 2015. The user has requested enhancement of the downloaded file. M. Razaeian et al.: Method© 2008 ofCrisis Suicide Hogrefe2008; in Tehran Vol.& Huber 29(3):164–166 2000–2004 Publishers Short Report The Most Common Method of Suicide in Tehran 2000–2004 Implications for Prevention Mohsen Razaeian1,2, Maryam Mohammadi2, Malihe Akbari2, and Maryam Maleki2 1Social Medicine Department, School of Medicine, Rafsanjan University of Medical Sciences 2Public Health Department, School of Health, Shaheed Beheshti University of Medical Sciences, both Tehran, Iran Abstract. The likelihood of completing suicide depends to some extent on knowledge of effective means and also on the availability and/or acceptability of such methods. Since studying suicide methods may have an implication for prevention, the focus of this study was on the most favored method of suicide in Tehran, Iran. The study uses confirmed suicide data provided by the Beheshet Zahra Organization (BZO), which gathers all mortality data within Tehran and enters them into a computerized database, from which the relevant information for all the recorded suicide cases during the year 2000 to 2004 were obtained and analyzed. -
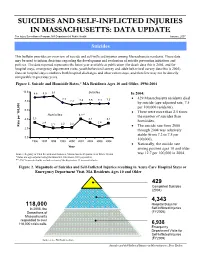
Suicides and Self-Inflicted Injuries in Massachusetts: Data Update
SSUUIICCIIDDEESS AANNDD SSEELLFF--IINNFFLLIICCTTEEDD IINNJJUURRIIEESS IINN MMAASSSSAACCHHUUSSEETTTTSS:: DDAATTAA UUPPDDAATTEE The Injury Surveillance Program, MA Department of Public Health January, 2007 Suicides This bulletin provides an overview of suicide and self-inflicted injuries among Massachusetts residents. These data may be used to inform decisions regarding the development and evaluation of suicide prevention initiatives and policies. The data reported represents the latest year available at publication (for death data this is 2004, and for hospital stays, emergency department visits, youth behavioral survey and adult behavioral survey data this is 2005). Data on hospital stays combines both hospital discharges and observation stays, and therefore may not be directly comparable to previous years. Figure 1. Suicide and Homicide Rates,* MA Residents Ages 10 and Older, 1996-2004 10.0 8.8 8.9 9.1 Suicides In 2004: 7.7 • 429 Massachusetts residents died 8.0 7.2 7.4 7.5 7.4 7.5 by suicide (age-adjusted rate, 7.5 per 100,000 residents). 6.0 • There were more than 2.5 times Homicides 4.1** the number of suicides than 4.0 3.3 3.2 3.1 2.4 2.4 homicides. 2.1 2.2 2.2 100,000 per Rate • The suicide rate from 2000 2.0 through 2004 was relatively stable (from 7.2 to 7.5 per 0.0 100,000). 1996 1997 1998 1999 2000 2001 2002 2003 2004 • Nationally, the suicide rate Year among persons ages 10 and older Source: Registry of Vital Records and Statistics, Massachusetts Department of Public Health was 12.7 per 100,000 in 2004. -

Age Differences in Suicide Methods
Forensic Research & Criminology International Journal Research Article Open Access Age differences in suicide methods Abstract Volume 6 Issue 6 - 2018 Objective: There is not adequate research on suicide methods by age in Turkey. The purpose of the present study is to investigate whether there is any change in suicide methods Mustafa Demir by age over time and whether suicide methods significantly differ by age. State University of New York at Plattsburgh, USA Method: Secondary data about suicide from 2007 to 2015 were obtained from the Turkish Correspondence: Mustafa Demir, State University of New Statistical Institute. The number of suicide cases was 25,696. Direct standardization method York at Plattsburgh, USA, Tel +15185643305, was used to calculate suicide rates. Line charts were plotted to reveal the trends in suicide Email methods by age. Then, one-way anova (ANOVA) test was conducted to test whether suicide methods significantly differed by age. Received: June 05, 2017 | Published: December 11, 2018 Results: Among all ages, hanging was the most common suicide method, followed by firearm, jumping, intoxication, and cutting/burning among all age groups. Moreover, all of the other suicide methods increased except for cutting/burning among those aged 15- 24 years, except for firearm among those aged 25-44 years, except for hanging among those aged 45-64 years. Among those aged 65 and older, suicide by hanging decreased, however, suicide by other methods overall remained stable. The results also showed that with increasing age, suicide by hanging, jumping, and cutting increased, while suicide by firearm and intoxication decreased. In addition, the results of ANOVA test indicated that except for intoxication, all other suicide methods differed significantly by age groups. -

Responding to Murder Suicide and Suicide Clusters
Responding to murder suicide and suicide clusters Guidance document April 2011 Final Version - 18 April 2011GD 1 Contents 1. Foreword 2. Executive Summary 3. Background: rationale membership 4. Prevention – key elements 5. Murder Suicide & Suicide Clusters – some definitions 6. Suicide Mortality 7. Research evidence 8. Learning from our own and others’ experience 9. Guidance for the management of suicide and suicide clusters at local HSE level. 10. Implementing the Plan 11. Role of the media 12. Appendices Appendix 1 – National Working Group Terms of Reference and Membership Appendix 2 - Media guidelines for reporting suicide Appendix 3 – Websites and information resources. Final Version - 18 April 2011GD 2 1. Foreword Suicide remains a significant public health issue in Ireland. However in the last few years in Ireland the relatively rare events of murder suicide and suicide clusters have become more prevalent. When such events occur they have often attracted high profile media coverage. There is therefore a need for a consistent and coordinated health and social care response. This guidance document is designed to be an accessible resource for local service managers when responding to such tragic events as murder-suicide and suicide clusters. Murder suicides occur when one person, or persons, kill others and then take their own lives. Suicide clusters emerge when a number of apparent suicides, which may appear to be unrelated, occur in a particular area over a particular time period and have common or similar method. These are sometimes referred to as ‘copycat’ suicides. Whilst the HSE has a significant and often lead role to play there are many other organisations, both statutory and voluntary, which can make an important contribution. -

Lethality of Firearms Relative to Other Suicide Methods: a Population Based Study E D Shenassa, S N Catlin, S L Buka
J Epidemiol Community Health: first published as 10.1136/jech.57.2.120 on 1 February 2003. Downloaded from 120 RESEARCH REPORT Lethality of firearms relative to other suicide methods: a population based study E D Shenassa, S N Catlin, S L Buka ............................................................................................................................. J Epidemiol Community Health 2003;57:120–124 Objectives: (1) To quantify lethality of firearms relative to other suicide methods, (2) to quantify the extent to which suicide mortality may be reduced by limiting access to firearms. Methods: Data on suicides and hospitalised para-suicides that occurred in the state of Illinois from 1990 to 1997 were combined. Total number of episodes for each suicide method was estimated as See end of article for the sum of the number of suicides and the number of para-suicides for that method. Gender and suicide authors’ affiliations method were used as proxies for intention to die, and estimated lethality of suicide methods within ....................... method-gender groups (for example, male firearm users). Logistic regression was used to quantify the Correspondence to: lethality of firearms relative to other suicide methods. Excess mortality associated with the use of fire- Dr E D Shenassa, Centers arms was estimated by conservatively assuming that in the absence of firearms the next most lethal for Behavioral and suicide method would be used. Preventive Medicine, One Results: From January 1990 to December 1997, among individuals 10 years or older in the state of Hoppin Street, Suite 500, Illinois, there were 37 352 hospital admissions for para-suicide and 10 287 completed suicides. Fire- Providence, RI 02903, USA; arms are the most lethal suicide method. -

Epidemiology of Suicide in Cuba, 1987–2014
Original Research Epidemiology of Suicide in Cuba, 1987–2014 Beatriz Corona-Miranda MD MS, Karen Alfonso-Sagué, Mariela Hernández-Sánchez MD MS, Paula Lomba-Acevedo MD MS ABSTRACT RESULTS A total of 51,113 deaths by suicide were reported (annual average 1825), of which 34,671 (67.8%) were among men. The sex INTRODUCTION Suicide is a health problem infl uenced by biological, ratio was 2.1:1 for the entire study period, and 3.9:1 for 2011–2014. genetic, psychological, social and economic factors. It is responsible Over the course of the period studied, age-standardized suicide for 50% of violent deaths in the male population, worldwide, and 71% rates decreased from 23.9 to 10.8 per 100,000 population (54.8% in the female. In the Americas, 65,000 deaths by suicide occur every reduction). The group aged ≥60 years had the highest average age- year. It is the ninth most frequent cause of death in Cuba, and third standardized rate, 44.6 per 100,000 population. The highest suicide among people aged 10–19. burden by age was in the group aged 20–59 years (60.5%). By skin color, the highest burden was in those recorded as white, 68.9%. By OBJECTIVE Characterize the epidemiology of suicide in Cuba from marital status, the highest burden was in persons with a stable partner 1987 to 2014. (46.7%), and by employment status/occupation, in retired (25.9%). The most commonly used method was hanging (59.4%). METHODS A retrospective descriptive study was conducted. The information comprised all records of death by suicide from CONCLUSIONS Over the course of about three decades, suicide January 1, 1987 to December 31, 2014, in the Cuban Ministry of mortality rates have declined by almost half and they are still slightly Public Health’s National Statistics Division database. -

Full Main Text 2008.Pmd
A Search for Death: How the Internet Is Used as a Suicide Cookbook Rheana Murray Literature Review While reasons for suicides have long been analyzed, the Internet presents a comparatively unexamined influence. Recent news stories have begun to direct attention to the emergence of chat rooms, message boards and other resources on the web as a possible factor in the rise of suicide rates. As the Internet has become an increasingly vital technological development, some people have begun to worry about “suicide websites,” a term that refers to websites that promote, encourage and/or offer methods to commit suicide. Alao and colleagues (2006) address the role of the Internet on suicides in a manuscript composed of three parts. The first describes how the Internet can help users commit suicide; the second looks at cases in which this has happened; and the last explores how the Internet could be used to help suicidal users back to stable mental health. The authors include interesting and pertinent information about suicide websites, and they report that there are more than 100,000 of them that deal with suicide methods. Some sites do not allow entrance to anyone intending to persuade users to not commit suicide. Suicide notes, death certificates, color photographs of people committing suicide, messages supporting suicide or encouraging individuals to carry out planned suicides can all be found on these websites. Some of the websites are very graphic, even including “the best way to point a gun into the mouth for maximum effect,” according to the journal article (Alao 490). The article “Cybersuicide: Review of the Role of the Internet on Suicide” also acknowledges that chat rooms, as well as Chrestomathy: Annual Review of Undergraduate Research, School of Humanities and Social Sciences, School of Languages, Cultures, and World Affairs, College of Charleston Volume 7, 2008: pp.