Decidualized Endometrial Stromal Cells Present with Altered Androgen Response in PCOS
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Identification of BBX Proteins As Rate-Limiting Co-Factors of HY5
1 Identification of BBX proteins as rate-limiting co-factors of HY5. 2 Katharina Bursch1, Gabriela Toledo-Ortiz2, Marie Pireyre3, Miriam Lohr1, Cordula Braatz1, Henrik 3 Johansson1* 4 1. Institute of Biology/Applied Genetics, Dahlem Centre of Plant Sciences (DCPS), Freie Universität 5 Berlin, Albrecht-Thaer-Weg 6. D-14195 Berlin, Germany. 6 2. Lancaster Environment Centre, Lancaster University, Lancaster LA1 4YQ, UK 7 3. Department of Botany and Plant Biology, Section of Biology, Faculty of Sciences, University of 8 Geneva, 30 Quai E. Ansermet, 1211 Geneva 4, Switzerland 9 *E-mail [email protected] 10 Abstract 11 As a source of both energy and environmental information, monitoring the incoming light is crucial for 12 plants to optimize growth throughout development1. Concordantly, the light signalling pathways in 13 plants are highly integrated with numerous other regulatory pathways2,3. One of these signal 14 integrators is the bZIP transcription factor HY5 which holds a key role as a positive regulator of light 15 signalling in plants4,5. Although HY5 is thought to act as a DNA-binding transcriptional regulator6,7, the 16 lack of any apparent transactivation domain8 makes it unclear how HY5 is able to accomplish its many 17 functions. Here, we describe the identification of three B-box containing proteins (BBX20, 21 and 22) 18 as essential partners for HY5 dependent modulation of hypocotyl elongation, anthocyanin 19 accumulation and transcriptional regulation. The bbx202122 triple mutant mimics the phenotypes of 20 hy5 in the light and its ability to suppress the cop1 mutant phenotype in darkness. Furthermore, 84% 21 of genes that exhibit differential expression in bbx202122 are also HY5 regulated, and we provide 22 evidence that HY5 requires the B-box proteins for transcriptional regulation. -
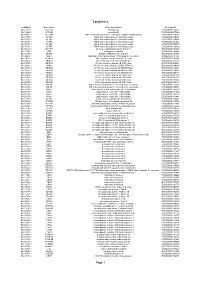
Epigenetics Page 1
Epigenetics esiRNA ID Gene Name Gene Description Ensembl ID HU-13237-1 ACTL6A actin-like 6A ENSG00000136518 HU-13925-1 ACTL6B actin-like 6B ENSG00000077080 HU-14457-1 ACTR1A ARP1 actin-related protein 1 homolog A, centractin alpha (yeast) ENSG00000138107 HU-10579-1 ACTR2 ARP2 actin-related protein 2 homolog (yeast) ENSG00000138071 HU-10837-1 ACTR3 ARP3 actin-related protein 3 homolog (yeast) ENSG00000115091 HU-09776-1 ACTR5 ARP5 actin-related protein 5 homolog (yeast) ENSG00000101442 HU-00773-1 ACTR6 ARP6 actin-related protein 6 homolog (yeast) ENSG00000075089 HU-07176-1 ACTR8 ARP8 actin-related protein 8 homolog (yeast) ENSG00000113812 HU-09411-1 AHCTF1 AT hook containing transcription factor 1 ENSG00000153207 HU-15150-1 AIRE autoimmune regulator ENSG00000160224 HU-12332-1 AKAP1 A kinase (PRKA) anchor protein 1 ENSG00000121057 HU-04065-1 ALG13 asparagine-linked glycosylation 13 homolog (S. cerevisiae) ENSG00000101901 HU-13552-1 ALKBH1 alkB, alkylation repair homolog 1 (E. coli) ENSG00000100601 HU-06662-1 ARID1A AT rich interactive domain 1A (SWI-like) ENSG00000117713 HU-12790-1 ARID1B AT rich interactive domain 1B (SWI1-like) ENSG00000049618 HU-09415-1 ARID2 AT rich interactive domain 2 (ARID, RFX-like) ENSG00000189079 HU-03890-1 ARID3A AT rich interactive domain 3A (BRIGHT-like) ENSG00000116017 HU-14677-1 ARID3B AT rich interactive domain 3B (BRIGHT-like) ENSG00000179361 HU-14203-1 ARID3C AT rich interactive domain 3C (BRIGHT-like) ENSG00000205143 HU-09104-1 ARID4A AT rich interactive domain 4A (RBP1-like) ENSG00000032219 HU-12512-1 ARID4B AT rich interactive domain 4B (RBP1-like) ENSG00000054267 HU-12520-1 ARID5A AT rich interactive domain 5A (MRF1-like) ENSG00000196843 HU-06595-1 ARID5B AT rich interactive domain 5B (MRF1-like) ENSG00000150347 HU-00556-1 ASF1A ASF1 anti-silencing function 1 homolog A (S. -

HMGB1 in Health and Disease R
Donald and Barbara Zucker School of Medicine Journal Articles Academic Works 2014 HMGB1 in health and disease R. Kang R. C. Chen Q. H. Zhang W. Hou S. Wu See next page for additional authors Follow this and additional works at: https://academicworks.medicine.hofstra.edu/articles Part of the Emergency Medicine Commons Recommended Citation Kang R, Chen R, Zhang Q, Hou W, Wu S, Fan X, Yan Z, Sun X, Wang H, Tang D, . HMGB1 in health and disease. 2014 Jan 01; 40():Article 533 [ p.]. Available from: https://academicworks.medicine.hofstra.edu/articles/533. Free full text article. This Article is brought to you for free and open access by Donald and Barbara Zucker School of Medicine Academic Works. It has been accepted for inclusion in Journal Articles by an authorized administrator of Donald and Barbara Zucker School of Medicine Academic Works. Authors R. Kang, R. C. Chen, Q. H. Zhang, W. Hou, S. Wu, X. G. Fan, Z. W. Yan, X. F. Sun, H. C. Wang, D. L. Tang, and +8 additional authors This article is available at Donald and Barbara Zucker School of Medicine Academic Works: https://academicworks.medicine.hofstra.edu/articles/533 NIH Public Access Author Manuscript Mol Aspects Med. Author manuscript; available in PMC 2015 December 01. NIH-PA Author ManuscriptPublished NIH-PA Author Manuscript in final edited NIH-PA Author Manuscript form as: Mol Aspects Med. 2014 December ; 0: 1–116. doi:10.1016/j.mam.2014.05.001. HMGB1 in Health and Disease Rui Kang1,*, Ruochan Chen1, Qiuhong Zhang1, Wen Hou1, Sha Wu1, Lizhi Cao2, Jin Huang3, Yan Yu2, Xue-gong Fan4, Zhengwen Yan1,5, Xiaofang Sun6, Haichao Wang7, Qingde Wang1, Allan Tsung1, Timothy R. -

Rationale for the Development of Alternative Forms of Androgen Deprivation Therapy
248 S Kumari, D Senapati et al. New approaches to inhibit 24:8 R275–R295 Review AR action Rationale for the development of alternative forms of androgen deprivation therapy Sangeeta Kumari1,*, Dhirodatta Senapati1,* and Hannelore V Heemers1,2,3 1Department of Cancer Biology, Cleveland Clinic, Cleveland, Ohio, USA Correspondence 2Department of Urology, Cleveland Clinic, Cleveland, Ohio, USA should be addressed 3Department of Hematology/Medical Oncology, Cleveland Clinic, Cleveland, Ohio, USA to H V Heemers *(S Kumari and D Senapati contributed equally to this work) Email [email protected] Abstract With few exceptions, the almost 30,000 prostate cancer deaths annually in the United Key Words States are due to failure of androgen deprivation therapy. Androgen deprivation f androgen receptor therapy prevents ligand-activation of the androgen receptor. Despite initial remission f prostate cancer after androgen deprivation therapy, prostate cancer almost invariably progresses while f nuclear receptor continuing to rely on androgen receptor action. Androgen receptor’s transcriptional f coregulator output, which ultimately controls prostate cancer behavior, is an alternative therapeutic f transcription target, but its molecular regulation is poorly understood. Recent insights in the molecular f castration mechanisms by which the androgen receptor controls transcription of its target genes f hormonal therapy are uncovering gene specificity as well as context-dependency. Heterogeneity in the Endocrine-Related Cancer Endocrine-Related androgen receptor’s transcriptional output is reflected both in its recruitment to diverse cognate DNA binding motifs and in its preferential interaction with associated pioneering factors, other secondary transcription factors and coregulators at those sites. This variability suggests that multiple, distinct modes of androgen receptor action that regulate diverse aspects of prostate cancer biology and contribute differentially to prostate cancer’s clinical progression are active simultaneously in prostate cancer cells. -

Transcriptional and Post-Transcriptional Regulation of ATP-Binding Cassette Transporter Expression
Transcriptional and Post-transcriptional Regulation of ATP-binding Cassette Transporter Expression by Aparna Chhibber DISSERTATION Submitted in partial satisfaction of the requirements for the degree of DOCTOR OF PHILOSOPHY in Pharmaceutical Sciences and Pbarmacogenomies in the Copyright 2014 by Aparna Chhibber ii Acknowledgements First and foremost, I would like to thank my advisor, Dr. Deanna Kroetz. More than just a research advisor, Deanna has clearly made it a priority to guide her students to become better scientists, and I am grateful for the countless hours she has spent editing papers, developing presentations, discussing research, and so much more. I would not have made it this far without her support and guidance. My thesis committee has provided valuable advice through the years. Dr. Nadav Ahituv in particular has been a source of support from my first year in the graduate program as my academic advisor, qualifying exam committee chair, and finally thesis committee member. Dr. Kathy Giacomini graciously stepped in as a member of my thesis committee in my 3rd year, and Dr. Steven Brenner provided valuable input as thesis committee member in my 2nd year. My labmates over the past five years have been incredible colleagues and friends. Dr. Svetlana Markova first welcomed me into the lab and taught me numerous laboratory techniques, and has always been willing to act as a sounding board. Michael Martin has been my partner-in-crime in the lab from the beginning, and has made my days in lab fly by. Dr. Yingmei Lui has made the lab run smoothly, and has always been willing to jump in to help me at a moment’s notice. -

Epigenetic Services Citations
Active Motif Epigenetic Services Publications The papers below contain data generated by Active Motif’s Epigenetic Services team. To learn more about our services, please give us a call or visit us at www.activemotif.com/services. Technique Target Journal Year Reference Justin C. Boucher et al. CD28 Costimulatory Domain- ATAC-Seq, Cancer Immunol. Targeted Mutations Enhance Chimeric Antigen Receptor — 2021 RNA-Seq Res. T-cell Function. Cancer Immunol. Res. doi: 10.1158/2326- 6066.CIR-20-0253. Satvik Mareedu et al. Sarcolipin haploinsufficiency Am. J. Physiol. prevents dystrophic cardiomyopathy in mdx mice. RNA-Seq — Heart Circ. 2021 Am J Physiol Heart Circ Physiol. doi: 10.1152/ Physiol. ajpheart.00601.2020. Gabi Schutzius et al. BET bromodomain inhibitors regulate Nature Chemical ChIP-Seq BRD4 2021 keratinocyte plasticity. Nat. Chem. Biol. doi: 10.1038/ Biology s41589-020-00716-z. Siyun Wang et al. cMET promotes metastasis and ChIP-qPCR FOXO3 J. Cell Physiol. 2021 epithelial-mesenchymal transition in colorectal carcinoma by repressing RKIP. J. Cell Physiol. doi: 10.1002/jcp.30142. Sonia Iyer et al. Genetically Defined Syngeneic Mouse Models of Ovarian Cancer as Tools for the Discovery of ATAC-Seq — Cancer Discovery 2021 Combination Immunotherapy. Cancer Discov. doi: doi: 10.1158/2159-8290 Vinod Krishna et al. Integration of the Transcriptome and Genome-Wide Landscape of BRD2 and BRD4 Binding BRD2, BRD4, RNA Motifs Identifies Key Superenhancer Genes and Reveals ChIP-Seq J. Immunol. 2021 Pol II the Mechanism of Bet Inhibitor Action in Rheumatoid Arthritis Synovial Fibroblasts. J. Immunol. doi: doi: 10.4049/ jimmunol.2000286. Daniel Haag et al. -

Original Article a Database and Functional Annotation of NF-Κb Target Genes
Int J Clin Exp Med 2016;9(5):7986-7995 www.ijcem.com /ISSN:1940-5901/IJCEM0019172 Original Article A database and functional annotation of NF-κB target genes Yang Yang, Jian Wu, Jinke Wang The State Key Laboratory of Bioelectronics, Southeast University, Nanjing 210096, People’s Republic of China Received November 4, 2015; Accepted February 10, 2016; Epub May 15, 2016; Published May 30, 2016 Abstract: Backgrounds: The previous studies show that the transcription factor NF-κB always be induced by many inducers, and can regulate the expressions of many genes. The aim of the present study is to explore the database and functional annotation of NF-κB target genes. Methods: In this study, we manually collected the most complete listing of all NF-κB target genes identified to date, including the NF-κB microRNA target genes and built the database of NF-κB target genes with the detailed information of each target gene and annotated it by DAVID tools. Results: The NF-κB target genes database was established (http://tfdb.seu.edu.cn/nfkb/). The collected data confirmed that NF-κB maintains multitudinous biological functions and possesses the considerable complexity and diversity in regulation the expression of corresponding target genes set. The data showed that the NF-κB was a central regula- tor of the stress response, immune response and cellular metabolic processes. NF-κB involved in bone disease, immunological disease and cardiovascular disease, various cancers and nervous disease. NF-κB can modulate the expression activity of other transcriptional factors. Inhibition of IKK and IκBα phosphorylation, the decrease of nuclear translocation of p65 and the reduction of intracellular glutathione level determined the up-regulation or down-regulation of expression of NF-κB target genes. -

Genome-Wide Identi Cation, Characterization and Evolution of BBX Gene Family in Cotton
Genome-Wide Identication, Characterization and Evolution of BBX Gene Family in Cotton Jun-Shan Gao ( [email protected] ) Anhui Agricultural University Pei-pei Wang Anhui Agricultural University Na Sun Anhui Agricultural University Jessica-Maguy Anhui Agricultural University MIENANDI NKODIA Anhui Agricultural University Yong Wu Anhui Agricultural University Ning Guo Anhui Agricultural University Da-Hui Li Anhui Agricultural University Research article Keywords: B-BOX, cotton, GhBBX, systematic analysis, proanthocyanidin Posted Date: December 11th, 2020 DOI: https://doi.org/10.21203/rs.3.rs-120586/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Page 1/25 Abstract Background: The B-BOX (BBX) proteins have important functions in the regulation of photomorphogenesis. The BBX gene family has been identied in several plants, such as rice, Arabidopsis and tomato. However, there still lack a genome-wide survey of BBX genes in cotton. Results: In our present study, 63 GhBBX genes were identied in cotton. The analyses of phylogenetic evolution and gene structure showed that the GhBBX genes were divided into ve subfamilies, and contained B-box conserved domains. qRT-PCR analysis releaved that both GhBBX27 and GhBBX33 had potential roles in proanthocyanidin synthesis of brown cotton bers. Conclusions: This study provides a genome-wide survey of the BBX gene family in cotton and highlights its role in proanthocyanidin synthesis. This result will help us to further understand the complexity of the BBX gene family and the functional characteristics of its members. Background The zinc nger protein is a member of the transcription factor family and has a large proportion in plants, which has been reported in rice, soybean and Arabidopsis[1]. -

Recurrent Inversion Toggling and Great Ape Genome Evolution
HHS Public Access Author manuscript Author ManuscriptAuthor Manuscript Author Nat Genet Manuscript Author . Author manuscript; Manuscript Author available in PMC 2020 December 15. Published in final edited form as: Nat Genet. 2020 August ; 52(8): 849–858. doi:10.1038/s41588-020-0646-x. Recurrent inversion toggling and great ape genome evolution David Porubsky1,2,9, Ashley D. Sanders3,9, Wolfram Höps3, PingHsun Hsieh1, Arvis Sulovari1, Ruiyang Li1, Ludovica Mercuri4, Melanie Sorensen1, Shwetha C. Murali1,5, David Gordon1,5, Stuart Cantsilieris1,6, Alex A. Pollen7, Mario Ventura4, Francesca Antonacci4, Tobias Marschall8, Jan O. Korbel3, Evan E. Eichler1,5,* 1Department of Genome Sciences, University of Washington School of Medicine, Seattle, Washington, USA. 2Max Planck Institute for Informatics, Saarland Informatics Campus E1.4, Saarbrücken, Germany. 3European Molecular Biology Laboratory (EMBL), Genome Biology Unit, Heidelberg, Germany. 4Dipartimento di Biologia, Università degli Studi di Bari “Aldo Moro”, Bari, Italy. 5Howard Hughes Medical Institute, University of Washington, Seattle, Washington, USA. 6Centre for Eye Research Australia, Department of Surgery (Ophthalmology), University of Melbourne, Royal Victorian Eye and Ear Hospital, East Melbourne, Victoria, Australia. 7Department of Neurology, University of California, San Francisco (UCSF), San Francisco, California, USA. 8Institute for Medical Biometry and Bioinformatics, Medical Faculty, Heinrich Heine University Düsseldorf, Germany. 9These authors contributed equally to this work. Abstract Inversions play an important role in disease and evolution but are difficult to characterize because their breakpoints map to large repeats. We increased by six-fold the number (n = 1,069) of previously reported great ape inversions using Strand-seq and long-read sequencing. We find that the X chromosome is most enriched (2.5-fold) for inversions based on its size and duplication content. -

In-Silico Discovery of Cancer-Specific Peptide-HLA Complexes for Targeted Therapy Ankur Dhanik*, Jessica R
Dhanik et al. BMC Bioinformatics (2016) 17:286 DOI 10.1186/s12859-016-1150-2 RESEARCH ARTICLE Open Access In-silico discovery of cancer-specific peptide-HLA complexes for targeted therapy Ankur Dhanik*, Jessica R. Kirshner, Douglas MacDonald, Gavin Thurston, Hsin C. Lin, Andrew J. Murphy and Wen Zhang Abstract Background: Major Histocompatibility Complex (MHC) or Human Leukocyte Antigen (HLA) Class I molecules bind to peptide fragments of proteins degraded inside the cell and display them on the cell surface. We are interested in peptide-HLA complexes involving peptides that are derived from proteins specifically expressed in cancer cells. Such complexes have been shown to provide an effective means of precisely targeting cancer cells by engineered T-cells and antibodies, which would be an improvement over current chemotherapeutic agents that indiscriminately kill proliferating cells. An important concern with the targeting of peptide-HLA complexes is off-target toxicity that could occur due to the presence of complexes similar to the target complex in cells from essential, normal tissues. Results: We developed a novel computational strategy for identifying potential peptide-HLA cancer targets and evaluating the likelihood of off-target toxicity associated with these targets. Our strategy combines sequence-based and structure-based approaches in a unique way to predict potential off-targets. The focus of our work is on the complexes involving the most frequent HLA class I allele HLA-A*02:01. Using our strategy, we predicted the off-target toxicity observed in past clinical trials. We employed it to perform a first-ever comprehensive exploration of the human peptidome to identify cancer-specific targets utilizing gene expression data from TCGA (The Cancer Genome Atlas) and GTEx (Gene Tissue Expression), and structural data from PDB (Protein Data Bank). -

View a Copy of This Licence, Visit
Robertson et al. BMC Biology (2020) 18:103 https://doi.org/10.1186/s12915-020-00826-z RESEARCH ARTICLE Open Access Large-scale discovery of male reproductive tract-specific genes through analysis of RNA-seq datasets Matthew J. Robertson1,2, Katarzyna Kent3,4,5, Nathan Tharp3,4,5, Kaori Nozawa3,5, Laura Dean3,4,5, Michelle Mathew3,4,5, Sandra L. Grimm2,6, Zhifeng Yu3,5, Christine Légaré7,8, Yoshitaka Fujihara3,5,9,10, Masahito Ikawa9, Robert Sullivan7,8, Cristian Coarfa1,2,6*, Martin M. Matzuk1,3,5,6 and Thomas X. Garcia3,4,5* Abstract Background: The development of a safe, effective, reversible, non-hormonal contraceptive method for men has been an ongoing effort for the past few decades. However, despite significant progress on elucidating the function of key proteins involved in reproduction, understanding male reproductive physiology is limited by incomplete information on the genes expressed in reproductive tissues, and no contraceptive targets have so far reached clinical trials. To advance product development, further identification of novel reproductive tract-specific genes leading to potentially druggable protein targets is imperative. Results: In this study, we expand on previous single tissue, single species studies by integrating analysis of publicly available human and mouse RNA-seq datasets whose initial published purpose was not focused on identifying male reproductive tract-specific targets. We also incorporate analysis of additional newly acquired human and mouse testis and epididymis samples to increase the number of targets identified. We detected a combined total of 1178 genes for which no previous evidence of male reproductive tract-specific expression was annotated, many of which are potentially druggable targets. -
Bioinformatic Pipeline for Whole Exome Sequence (WES) Analysis
SUPPLEMENT Supplement contents: Supplementary Methods Supplementary Figure 1: Bioinformatic pipeline for whole exome sequence (WES) analysis. Supplementary Figure 2: Pedigrees and HomozygosityMapper output for families with single variants identified, in addition to those shown in Figure 2. Supplementary Figure 3: Spatiotemporal expression of ID genes in human development using RNA sequencing data. Supplementary Figure 4: Developmental expression pattern of ID genes in the human prefrontal cortex. Supplementary Table 1: Family statistics Supplementary Table 2: Homozygosity-by-descent/autozygosity shared regions, as defined using HomozygosityMapper, cross-referenced with FSuite. Supplementary Table 3: Mutations identified per family. A. Single homozygous variant identified. B. Two to four variants identified. C. Dominant/de novo mutation identified. Supplementary Table 4: Pathogenic CNVs and variants of unknown significance identified by microarray analysis. Supplementary Table 5: BioGRID protein interaction and gene ontology analysis. (separate Excel file) Supplementary Table 6: Gene Ontology Pathway analysis. Supplementary Table 7: Gene List for anatomic/temporal transcription analyses. Supplementary Table 8: Top anatomical regions for ID gene expression. Supplementary Methods HBD/Autozygosity mapping Both of the below methods and the hg19 version of the genome were used to ensure a consistent and uniform genotyping. Genotyping data was uploaded to the HomozygosityMapper server to determine putative homozygous-by- descent (HBD) regions based on the allele frequencies of the markers uploaded to the server from previous studies. HBD regions were identified by manual curation and only HBD regions larger than 1 Mb shared between all affected members (and not unaffected members) of the family were chosen. These regions were extracted based on SNP RS numbers and these dbSNP identifiers were converted to a genomic position for used to represent genomic regions with NGS data.