Ambient and Controlled Particle Exposures As Triggers for Acute
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Town of Farmington Planning Board Meeting Minutes—APPROVED December 5, 2018
Page 1 of 47 Town of Farmington Planning Board Meeting Minutes—APPROVED December 5, 2018 Town of Farmington 1000 County Road 8 Farmington, New York 14425 PLANNING BOARD Wednesday, December 5, 2018, 2018, 7:00 p.m. MINUTES—APPROVED The following minutes are written as a summary of the main points that were made and are the official and permanent record of the actions taken by the Town of Farmington Planning Board. Remarks delivered during discussions are summarized and are not intended to be verbatim transcriptions. An audio recording of the meeting is made in accordance with the Planning Board adopted Rules of Procedure. The audio recording is retained for 12 months. ______________________________________________________________________________ Clerk’s Note: This meeting was held at the Farmington Highway Garage, 985 Hook Road, to ac- commodate the large number of attendees. ______________________________________________________________________________ Board Members Present: Edward Hemminger, Chairperson Adrian Bellis Shauncy Maloy Mary Neale Douglas Viets Staff Present: Lance S. Brabant, CPESC, Town of Farmington Engineer, MRB Group, D.P.C. Ronald L. Brand, Town of Farmington Director of Development and Planning David Degear, Town of Farmington Water and Sewer Superintendent Dan Delpriore, Town of Farmington Code Enforcement Officer Don Giroux, Town of Farmington Highway and Parks Superintendent Jeffrey D. Graff, Esq., Town of Farmington Attorney Jamie Kincaid, Town of Farmington Fire Marshal Donna LaPlant, Town of Farmington Assessor James Morse, Town of Farmington Code Enforcement Officer Collin Sowinski, MRB Group, D.P.C. John Weidenborner, Assistant Chief, Farmington Volunteer Fire Association Applicants Present: Daniel Compitello, Solar Project Developer, Delware River Solar, 130 North Winton Road, #10526, Rochester, N.Y. -

Street Scape Design Guidelines Route 96 Corridor
STREET SCAPE DESIGN GUIDELINES ROUTE 96 CORRIDOR December 2019 Adopted #______ of 2019 Resolution #______ of 2019 Town of Farmington Route 96 Main Street Corridor Streetscape Design Guidelines Table of Contents A. Purpose Page 1 B. Intent Page 1 C. Streetscape Requirements Page 2 D. General Landscaping Requirements Page 3 E. Street Trees Page 5 F. Landscaped Areas at Property Lines Page 6 G. Foundation Plantings Page 6 H. Buffering Dissimilar Uses Page 7 Appendices Appendix A: Streetscape Products Appendix B: Streetscape Corridor Map Appendix C: Streetscape Renderings Town of Farmington Streetscape Design Guidelines N:\0610.12001.000\REPORTS\Street Scape\Streetscape Design Guidelines - DRAFT.docx December 2019 i Town of Farmington Streetscape Design Guidelines A. Purpose The purpose of these Guidelines is to provide minimum criteria for the design and construction of visual and pedestrian oriented site improvements associated with all development located along the Route 96 Main Street Corridor within the Town of Farmington. The Main Street Corridor is defined as properties fronting along both the north and south sides of New York State Route 96, commencing on the west at the Farmington/Victor Town Line and continuing east to the intersection of Route 96 with Hook Road and Beaver Creek Road, and extending further along Route 96 to Fairdale Glen on the north side only. The information contained in this document is to be used in conjunction with the subdivision and site plan regulations provided in the Town Code. B. Intent The intent of these guidelines is to implement an appropriate transportation network as called for in Chapter 3, Goals and Policies, of the adopted 2011 Edition of the Town of Farmington Comprehensive Plan, in particular “…prepare a Streetscape Plan as part of the Town Transportation Plan including guidelines for landscaping, light standards, bus stops, curbing and other elements of the streetscape.” [page 3- 27 dated July 26, 2011]. -

Appendix a – Traffic Volumes
Appendix A – Traffic Volumes Saugerties Area Mobility Analysis Town of Saugerties, New York Village of Saugerties, New York Town of Ulster, New York Appendix B – Parking Studies Saugerties Area Mobility Analysis Town of Saugerties, New York Village of Saugerties, New York Town of Ulster, New York Sawyer Bank Lot T S M L E M LAFA A YETT R E ST T K S E T S S S O T R C U L ST ER A V E IRVING ST 2 LIV N I NG D S P T A O S 1S N R T TI ST T T Village Lot S I O T N J O S H T N W A S S T H B U MAIN ST J R A N M W T E E S A R S S R T H I N G JANE S T T O M & T Bank Lot N A V E C E D A R DIVISION ST S T C E N T E R RUSSELL ST S T POST ST Aerial Map: Saugerties Village HILTON PL MONT ROSS ST Municipal Lot W B R M I C D S a u g e r t i e s A r e a M D G O T E S N S E T A S CLERMON R L T ST E D A D L N ST L Y E M (Downtown) Parking Survey Areas N S o b i l i t y A n a l y s i s T MONTGOMERY ST DO CK ST Areas Surveyed R D E Metered Parking S U Non-Metered ParkingO TH H IG Public Parking L L 05001,000A T H A 250 Private Parking M C I R December, 2005 Feet Downtown Saugerties Parking Survey On-Street Parking Occupancies Summary Surveys Taken on Saturdays 10/29/05 & 7/8/2006 Total # 9:30 AM 10:30AM 11:30AM 12:30PM 1:30PM 2:30PM 3:30PM 4:30PM 5:30PM Average of to to to to to to to to to Occ & Block/Location Parking Type Spaces 10:30 AM 11:30 AM 12:30 PM 1:30 PM 2:30PM 3:30PM 4:30PM 5:30PM 6:30PM Occ Rate Metered 119 70 88 104 109 105 98 81 78 72 89 59% 74% 87% 92% 88% 82% 68% 66% 61% 75% Unregulated 165 37 51 53 60 71 56 65 68 78 60 Oct-05 22% 31% 32% -

Town of Perinton Comprehensive Plan Update May 2011
Town of Perinton Comprehensive Plan Update May 2011 Prepared for: Town of Perinton, New York Prepared By: 2011 COMPREHENSIVE PLAN UPDATE TOWN OF PERINTON New York May 2011 2011 COMPREHENSIVE PLAN UPDATE TOWN OF PERINTON New York Prepared For: Town of Perinton Comprehensive Plan Update & Advisory Committees Prepared By: ACKNOWLEDGMENTS The 2011 Comprehensive Plan Update was made possible thanks to the time, input, support and dedication provided by the following individuals: TOWN OF PERINTON COMPREHENSIVE PLAN UPDATE COMMITTEE Town Board x Mark Anderson | Planning Board x John Beck | Deputy Director, Code Enforcement & Development James Smith, Town Supervisor x Thomas Beck | Commissioner, Department of Public Works Patricia Knapp, Town Council x James Brasley | Planning Board x Michael Doser | Director, Code Enforcement & Development Carolyn Saum, Town Council x Christine Fredette | Conservation Board Joseph LaFay, Town Council x Joseph LaFay | Town Board x John Moose | Zoning Board of Appeals Peg Havens, Town Council x Jeffrey Myers | Commissioner, Recreation and Parks x Robert Place | Town Attorney x Carolyn Saum | Town Board x David Schaeffer | Recreation and Parks Board x James Smith | Town Supervisor x Eric Williams | Assistant to Commissioner, Department of Public Works TOWN OF PERINTON COMPREHENSIVE PLAN ADVISORY COMMITTEE x Vincent Arcarese | Zoning Board of Appeals x David Belaskas | Conservation Board x Van Cardilli | Chamber of Commerce x John Colaruotolo | Business Owner x Samuel DiPrima | Business Owner x Friedrich Grasberger -

Earthen Embankment Integrity Program SEQR Draft Generic Environmental Impact Statement
Earthen Embankment Integrity Program SEQR Draft Generic Environmental Impact Statement March 2021 Prepared for: New York State Canal Corporation 30 South Pearl Street Albany, New York 12207-2058 (518) 449-6000 Prepared by: Bergmann and New York Power Authority Date of Issuance: ___________________________ Date by which comments must be submitted: _____________________ Contact Person: James Candiloro, P.E., Director, Environment, Health & Safety, New York State Canal Corporation, 30 South Pearl Street, Albany, New York 12207-2058 (518) 433-6841 NEW YORK STATE CANAL CORPORATION Earthen Embankment Integrity Program SEQR Draft Generic Environmental Impact Statement Table of Contents 1 SEQRA and Description of the Proposed Action.................................................................................1-1 1.1 Project Background ................................................................................................................................1-1 1.2 New York State Environmental Quality Review Act..................................................................1-4 1.3 Project Description ..................................................................................................................................1-6 2 Alternatives Considered .................................................................................................................................2-1 2.1 Null or No-Action Alternative ............................................................................................................2-1 2.2 -

Town of Covert Personnel Policy and Procedures
TOWN OF COVERT PERSONNEL POLICY AND PROCEDURES REVISED AND APPROVED BY THE TOWN BOARD ON January 9, 2017 The policy shall be reviewed by the Covert Town Board each January at the organizational meeting 1 INTRODUCTION In order to have a properly functioning organization that meets the needs of both the employees of the Town of Covert and the Taxpayers who really are their employers, a set of policies and rules are needed. The following set of policies shall apply to all full-time, part-time, permanent, elected, and appointed employees of the Town of Covert. If there is any question concerning the application of any provision, the employee should take the matter up with their immediate supervisor. If there is no immediate supervisor or the problem cannot be resolved at that level, the problem should be referred to the Town of Covert Supervisor who will bring it to the attention of the Town of Covert Board. The decision of the Board shall be final unless there is a proper legal challenge that can be made. All new employees shall be given a written copy of the Personnel Policy and Procedures. It shall be the responsibility of the employee to become familiar with the provisions of the policy. Employees shall abide by the policies as a condition of employment. Failure to comply with these policies shall be subject to sanctions, up to and including dismissal where warranted. 2 TABLE OF CONTENTS Introduction Welcome message from Supervisor &Town Board Section 1-1 Our Town Section 1-2 Town Meetings Section 1-3 Land Use Ordinance Section 1-4 Town -

商户 酒店品牌 所在城市 酒店名称 门店地址 Hilton Condominium Myrtle Beach Myrtle Beach-Kingston Plantation, SC 9800 Queensway Boulevard
商户 酒店品牌 所在城市 酒店名称 门店地址 Hilton Condominium Myrtle Beach Myrtle Beach-Kingston Plantation, SC 9800 Queensway Boulevard Hilton Conrad Chicago Chicago, IL 101 East Erie Street Internationa Hilton Conradl Indianapolis Indianapolis, IN 50 West Washington Street Internationa Hilton Conradl Miami Miami, FL 1395 Brickell Avenue Internationa Hilton Conradl New York New York, NY 102 North End Avenue Internationa Hilton Curiol Boston Ames Boston Hotel, MA 1 Court Street Hilton Curio Grand Rapids Amway Grand Plaza, Grand Rapids, MI 187 Monroe NW Hilton Curio Coronado Beach Village at The Del, CA 1277 R.H. Dana Place Hilton Curio Scottsdale Boulders Resort & Spa Scottsdale, AZ 34631 N. Tom Darlington Drive Hilton Curio Cupertino Cupertino, CA 10050 S. De Anza Boulevard Hilton Curio Hollywood Diplomat Hollywood, FL 3555 South Ocean Drive Hilton Curio Rapid City Hotel Alex Johnson Rapid City, SD 523 Sixth Street Hilton Curio Coronado Hotel del Coronado, CA 1500 Orange Ave Hilton Curio La Jolla Hotel La Jolla, CA 7955 La Jolla Shores Drive Hilton Curio Kansas City Hotel Phillips Kansas City, MO 106 W 12th Street Hilton Curio Roanoke Hotel Roanoke & Conference 110 Shenandoah Avenue Center,Curio Hilton Curio Chicago LondonHouse Chicago, IL 85 E Wacker Drive Hilton Curio Madison Madison, CT 94 West Wharf Road Hilton Curio Indian Wells Miramonte Indian Wells Resort & Spa, 45000 Indian Wells Lane CA Hilton Curio Baltimore Pier 5 Hotel Baltimore, MD 711 Eastern Avenue Hilton Curio Providence Providence Biltmore, RI 11 Dorrance Street Hilton Curio Birmingham Redmont Hotel Birmingham, AL 2101 5th Avenue North Hilton Curio St Louis St. Louis Union Station Hotel, MO 1820 Market St. -
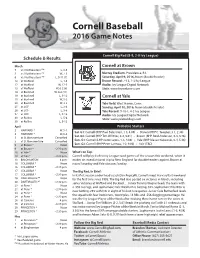
Cornell Baseball 2016 Game Notes
Cornell Baseball 2016 Game Notes Cornell Big Red (8-9, 2-0 Ivy League) Schedule & Results March Cornell at Brown 5 vs. Northeastern RMI L, 0-6 5 vs. Northeastern RMI W, 7-5 Murray Stadium, Providence, R.I. 6 vs. Northeastern RMI L, 0-11 (7) Saturday, April 9, 2016, Noon (doubleheader) 12 at Wofford L, 1-5 Brown Record: 7-13, 1-3 Ivy League 12 at Wofford W, 12-5 Audio: Ivy League Digital Network 13 at Wofford W, 6-2 (8) Stats: www.brownbears.com 18 at Bucknell W, 8-6 (11) 19 at Bucknell L, 3-12 Cornell at Yale 19 at Bucknell W, 5-2 20 at Bucknell W, 3-2 Yale Field, West Haven, Conn. 25 at UCF L, 3-4 Sunday, April 10, 2016, Noon (doubleheader) 26 at UCF L, 3-8 Yale Record: 9-18-1, 4-2 Ivy League 27 at UCF L, 0-16 Audio: Ivy League Digital Network 30 at Rollins L, 5-6 Stats: www.yalebulldogs.com 30 at Rollins L, 5-13 April Probable Starters 2 HARVARD * W, 5-1 Sat. G1: Cornell (RHP Paul Balestrieri, 1-3, 4.08) • Brown (RHP C. Taugner, 3-1, 2.38) 2 HARVARD * W, 6-4 Sat. G2: Cornell (RHP Tim Willittes, 2-2, 5.61) • Brown (RHP Reid Anderson, 0-3, 5.76) 5 at St. Bonaventure Cancelled 5 at St. Bonaventure Cancelled Sun. G1: Cornell (LHP Justin Lewis, 1-3, 4.08) • Yale (RHP Mason Kukowski, 0-4, 5.46) 9 at Brown * Noon Sun. G2: Cornell (RHP Peter Lannoo, 1-2, 9.00) • Yale (TBD) 9 at Brown * ~2:30 p.m. -

Town of Farmington Planning Board Meeting Minutes—APPROVED November 7, 2018
Page 1 of 43 Town of Farmington Planning Board Meeting Minutes—APPROVED November 7, 2018 Town of Farmington 1000 County Road 8 Farmington, New York 14425 PLANNING BOARD Wednesday, November 7, 2018, 2018, 7:00 p.m. MINUTES—APPROVED The following minutes are written as a summary of the main points that were made and are the official and permanent record of the actions taken by the Town of Farmington Planning Board. Remarks delivered during discussions are summarized and are not intended to be verbatim transcriptions. An audio recording of the meeting is made in accordance with the Planning Board adopted Rules of Procedure. The audio recording is retained for 12 months. ______________________________________________________________________________ Clerk’s Note 1: The Planning Board meeting of October 17, 2018, was cancelled due to having no applications or board business on the agenda. ______________________________________________________________________________ Board Members Present: Edward Hemminger, Chairperson Adrian Bellis Shauncy Maloy Mary Neale Douglas Viets Staff Present: Lance S. Brabant, CPESC, Town of Farmington Engineer, MRB Group, D.P.C. Ronald L. Brand, Town of Farmington Director of Development and Planning David Degear, Town of Farmington Water and Sewer Superintendent Dan Delpriore, Town of Farmington Code Enforcement Officer Don Giroux, Town of Farmington Highway and Parks Superintendent James Morse, Town of Farmington Code Enforcement Officer John Weidenborner, Assistant Chief, Farmington Volunteer Fire Association Applicants Present: Daniel Compitello, Solar Project Developer, Delware River Solar, 130 North Winton Road, #10526, Rochester, N.Y. 14610 Melissa Kiefer, Oldcastle Lawn & Garden Inc., Environmental Director, Oldcastle Lawn and Garden, 900 Ashwood Parkway, Suite 600, Atlanta, Georgia 30338 Patrick S. -

Site Development Plans for N/F Lake Edge Llc Tax Account No
HORIZONTAL SCALE 80 00 40 80 160 SITE DEVELOPMENT PLANS FOR SCALE: 1"=80' PASSERO ASSOCIATES VICTOR CDR+J engineering architecture DRAWING INDEX C 101 COVER TOWN OF VICTOR, ONTARIO COUNTY, NEW YORK C 102 EXISTING CONDITIONS AND DEMOLITION C 103 SITE P.N. 20182259.0001 C 104 UTILITY C 105 GRADING AND EROSION S87°47'31"W166.13' N18°52'29"W CONTROL PROPERTY LINE PER BILESCHI MAP # 32435 49.49' & PER LARUE MAP # 13715 C 106 LANDSCAPE S 43°47'17" E TAX ACCOUNT NO. 028.000-001-081 N/F JEFFREY CODY C 107 LIGHTING MCMAHON ROAD C 108 PROFILES N 08°12'26" W 216.71' C 200 NOTES C 201-205 DETAILS 245.74' S 00°17'43" W 00°17'43" S (234.14' MAP) (234.14' FEDERAL WETLAND 220.91' MEAS. 220.91' TAX ACCOUNT NO. 028.000-001-032.1 N 01°37'53" E 01°37'53" N N/F TOWN OF FARMINGTON #1216 MCMAHON ROAD SITE DATA 66.87' 1. TAX ACCOUNT NUMBER: 028.012-1-36 & 028.012-1-41.21 Town of Victor 2. PARCEL ADDRESS: 6484 STATE ROUTE 96 LOCATION SKETCH 3. TOTAL PARCEL AREA: ±10.897 ACRES OR 474,667 S.F. N.T.S. S 88°56'11" E TOTAL DISTURBED AREA: ±6.655 ACRES 180.97' MEAS. S88°56'11"E 319.91' Client: N 04°29'13" W 4. EXISTING ZONING: COMMERCIAL - LIGHT INDUSTRIAL 5. EXISTING USE: VACANT/RESIDENTIAL HOME VICTOR CDR & J STORMWATER MANAGEMENT AREA 6. PROPOSED USE: CAR DEALERSHIP REGULATION NO. -

Route 96 Corridor Plan
Route 96 Transformative Corridor Strategic Infrastructure Plan Prepared by: Prepared for the in association with Community of Victor March 2018 David A. Riley Route 96 Transformative Corridor Strategic Infrastructure Plan Financial assistance for the preparation of this report was provided by the Town of Victor, the Federal Highway Administration through the Genesee Transportation Council, and Empire State Development. The Town of Victor – as the lead agency – is solely responsible for its content and the views and opinions expressed herein do not necessarily reflect the official views or policy of the U.S. Department of Transportation. GTC’s Commitment to the Public The Genesee Transportation Council assures that no person shall, on the grounds of race, color, national origin, disability, age, gender, or income status, be excluded from participation in, be denied the benefits of, or be otherwise subjected to discrimination under any program or activity. GTC further assures every effort will be made to ensure nondiscrimination in all of its programs activities, whether those programs and activities are federally funded or not. En Español El Consejo Genesee del Transporte asegura completa implementación del Título VI de la Ley de Derechos Civiles de 1964, que prohibe la discriminación por motivo de raza, color de piel, origen nacional edad, género, discapacidad, o estado de ingresos, en la provisión de beneficios y servicios que sean resultado de programas y actividades que reciban asistencia financiera federal. Route 96 Transformative -

October 7, 2020
Page 1 of 84 Town of Farmington Planning Board Meeting Minutes—APPROVED October 7, 2020 Town of Farmington 1000 County Road 8 Farmington, New York 14425 PLANNING BOARD Wednesday, October 7, 2020 • 7:00 p.m. MINUTES—APPROVED The following minutes are written as a summary of the main points that were made and are the official and permanent record of the actions taken by the Town of Farmington Planning Board. Remarks delivered during discussions are summarized and are not intended to be verbatim transcriptions. An audio recording of the meeting is made in accordance with the Planning Board adopted Rules of Procedure. The audio recording is retained for 12 months. ______________________________________________________________________________ In response to the conditions in New York State that were created by the Coronavirus (COVID- 19) pandemic and the directives issued by the New York State Governor, the Ontario County Administrator and the Town of Farmington Supervisor, the Planning Board meeting this evening was held in accordance with New York State Governor Andrew M. Cuomo’s Executive Order No. 202.1: Continuing Temporary Suspension and Modification of Laws Relating to the Disaster Emergency, dated March 12, 2020, and extended by Executive Order 202.48 through November 3, 2020: Suspension of law allowing the attendance of meetings telephonically or other similar service: Article 7 of the Public Officers Law, to the extent necessary to permit an public body to meet and take such actions authorized by the law without permitting in public in-person access to meetings and authorizing such meetings to be held re- motely by conference call or similar service, provided that the public has the ability to view or listen to such proceeding and that such meetings are recorded and later transcribed.