Genotoxicity of Nanomaterials: Advanced in Vitro Models and High Throughput Methods for Human Hazard Assessment—A Review
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Krifka Publikation Glanzlicht 09
This article appeared in a journal published by Elsevier. The attached copy is furnished to the author for internal non-commercial research and education use, including for instruction at the authors institution and sharing with colleagues. Other uses, including reproduction and distribution, or selling or licensing copies, or posting to personal, institutional or third party websites are prohibited. In most cases authors are permitted to post their version of the article (e.g. in Word or Tex form) to their personal website or institutional repository. Authors requiring further information regarding Elsevier’s archiving and manuscript policies are encouraged to visit: http://www.elsevier.com/copyright Author's personal copy Biomaterials 32 (2011) 1787e1795 Contents lists available at ScienceDirect Biomaterials journal homepage: www.elsevier.com/locate/biomaterials Activation of stress-regulated transcription factors by triethylene glycol dimethacrylate monomer Stephanie Krifka a, Christine Petzel a, Carola Bolay a, Karl-Anton Hiller a, Gianrico Spagnuolo b, Gottfried Schmalz a, Helmut Schweikl a,* a Department of Operative Dentistry and Periodontology, University of Regensburg, D-93042 Regensburg, Germany b Department of Oral and Maxillofacial Sciences, University of Naples “Federico II”, Italy article info abstract Article history: Triethylene glycol dimethacrylate (TEGDMA) is a resin monomer available for short exposure scenarios of Received 22 October 2010 oral tissues due to incomplete polymerization processes of dental composite materials. The generation of Accepted 14 November 2010 reactive oxygen species (ROS) in the presence of resin monomers is discussed as a common mechanism Available online 10 December 2010 underlying cellular reactions as diverse as disturbed responses of the innate immune system, inhibition of dentin mineralization processes, genotoxicity and a delayed cell cycle. -

Principles and Methods for the Risk Assessment of Chemicals in Food
WORLD HEALTH ORGANIZATION ORGANISATION MONDIALE DE LA SANTE EHC240: Principles and Methods for the Risk Assessment of Chemicals in Food SUBCHAPTER 4.5. Genotoxicity Draft 12/12/2019 Deadline for comments 31/01/2020 The contents of this restricted document may not be divulged to persons other than those to whom it has been originally addressed. It may not be further distributed nor reproduced in any manner and should not be referenced in bibliographical matter or cited. Le contenu du présent document à distribution restreinte ne doit pas être divulgué à des personnes autres que celles à qui il était initialement destiné. Il ne saurait faire l’objet d’une redistribution ou d’une reproduction quelconque et ne doit pas figurer dans une bibliographie ou être cité. Hazard Identification and Characterization 4.5 Genotoxicity ................................................................................. 3 4.5.1 Introduction ........................................................................ 3 4.5.1.1 Risk Analysis Context and Problem Formulation .. 5 4.5.2 Tests for genetic toxicity ............................................... 14 4.5.2.2 Bacterial mutagenicity ............................................. 18 4.5.2.2 In vitro mammalian cell mutagenicity .................... 18 4.5.2.3 In vivo mammalian cell mutagenicity ..................... 20 4.5.2.4 In vitro chromosomal damage assays .................. 22 4.5.2.5 In vivo chromosomal damage assays ................... 23 4.5.2.6 In vitro DNA damage/repair assays ....................... 24 4.5.2.7 In vivo DNA damage/repair assays ....................... 25 4.5.3 Interpretation of test results ......................................... 26 4.5.3.1 Identification of relevant studies............................. 27 4.5.3.2 Presentation and categorization of results ........... 30 4.5.3.3 Weighting and integration of results ..................... -

FDA Genetic Toxicology Workshop How Many Doses of an Ames
FDA Genetic Toxicology Workshop How many doses of an Ames- Positive/Mutagenic (DNA Reactive) Drug can be safely administered to Healthy Subjects? November 4, 2019 Enrollment of Healthy Subjects into First-In-Human phase 1 clinical trials • Healthy subjects are commonly enrolled into First-In-Human (FIH) phase 1 clinical trials of new drug candidates. • Studies are typically short (few days up to 2 weeks) • Treatment may be continuous or intermittent (e.g., washout period of 5 half- lives between doses) • Receive no benefits and potentially exposed to significant health risks • Patients will be enrolled in longer phase 2 and 3 trials • Advantages of conducting trials with healthy subjects include: • investigation of pharmacokinetics (PK)/bioavailability in the absence of other potentially confounding drugs • data not confounded by disease • Identification of maximum tolerated dose • reduction in patient exposure to ineffective drugs or doses • rapid subject accrual into a study 2 Supporting Nonclinical Pharmacology and Toxicology Studies • The supporting nonclinical data package for a new IND includes • pharmacology studies (in vitro and in vivo) • safety pharmacology studies (hERG, ECG, cardiovascular, and respiratory) • secondary pharmacology studies • TK/ADME studies (in vitro and in vivo) • 14- to 28-day toxicology studies in a rodent and non-rodent • standard battery of genetic toxicity studies (Ames bacterial reverse mutation assay, in vitro mammalian cell assay, and an in vivo micronucleus assay) • Toxicology studies are used to • select clinical doses that are adequately supported by the data • assist with clinical monitoring • Genetic toxicity studies are used for hazard identification • Cancer drugs are often presumed to be genotoxic and genetic toxicity studies are generally not required for clinical trials in cancer patients. -
S2(R1) Genotoxicity Testing and Data Interpretation for Pharmaceuticals Intended for Human Use
Guidance for Industry S2(R1) Genotoxicity Testing and Data Interpretation for Pharmaceuticals Intended for Human Use U.S. Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and Research (CDER) Center for Biologics Evaluation and Research (CBER) June 2012 ICH Guidance for Industry S2(R1) Genotoxicity Testing and Data Interpretation for Pharmaceuticals Intended for Human Use Additional copies are available from: Office of Communications Division of Drug Information, WO51, Room 2201 Center for Drug Evaluation and Research Food and Drug Administration 10903 New Hampshire Ave., Silver Spring, MD 20993-0002 Phone: 301-796-3400; Fax: 301-847-8714 [email protected] http://www.fda.gov/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/default.htm and/or Office of Communication, Outreach and Development, HFM-40 Center for Biologics Evaluation and Research Food and Drug Administration 1401 Rockville Pike, Rockville, MD 20852-1448 http://www.fda.gov/BiologicsBloodVaccines/GuidanceComplianceRegulatoryInformation/Guidances/default.htm (Tel) 800-835-4709 or 301-827-1800 U.S. Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and Research (CDER) Center for Biologics Evaluation and Research (CBER) June 2012 ICH Contains Nonbinding Recommendations TABLE OF CONTENTS I. INTRODUCTION (1)....................................................................................................... 1 A. Objectives of the Guidance (1.1)...................................................................................................1 -

Comparative Genotoxicity of Adriamycin and Menogarol, Two Anthracycline Antitumor Agents
[CANCER RESEARCH 43, 5293-5297, November 1983] Comparative Genotoxicity of Adriamycin and Menogarol, Two Anthracycline Antitumor Agents B. K. Bhuyan,1 D. M. Zimmer, J. H. Mazurek, R. J. Trzos, P. R. Harbach, V. S. Shu, and M. A. Johnson Departments of Cancer Research [B. K. B.. D. M. Z.], Pathology and Toxicology Research [J. H. M., R. J. T., P. R. H.], and Biostatist/cs [V. S. S., M. A. J.], The Upjohn Company, Kalamazoo, Michigan 49001 ABSTRACT murine tumors such as P388 and L1210 leukemias and B16 melanoma (13). However, the biochemical activity of Adriamycin Adriamycin and menogarol are anthracyclines which cause and menogarol were markedly different in the following respects, more than 100% increase in life span of mice bearing P388 (a) at cytotoxic doses, Adriamycin inhibited RNA synthesis much leukemia and B16 melanoma. Unlike Adriamycin, menogarol more than DNA synthesis in L1210 cells in culture (10). In does not bind strongly to ONA, and it minimally inhibits DNA and contrast, menogarol caused very little inhibition of RNA or DNA RNA synthesis at lethal doses. Adriamycin is a clinically active synthesis at cytotoxic doses (10); (b) Adriamycin interacted drug, and menogarol is undergoing preclinical toxicology at Na strongly with DNA, in contrast to the weak interaction seen with tional Cancer Institute. In view of the reported mutagenicity of menogarol (10); (c) cells in S phase were most sensitive to Adriamycin, we have compared the genotoxicity of the two Adriamycin as compared to maximum toxicity of menogarol to drugs. Our results show that, although Adriamycin and meno cells in Gì(5).These results collectively suggested that meno garol differ significantly in their bacterial mutagenicity (Ames garol acts through some mechanism other than the intercalative assay), they have similar genotoxic activity in several mammalian DNA binding proposed for Adriamycin. -

Development and Validation of a High-Throughput Transcriptomic Biomarker to Address 21St Century Genetic Toxicology Needs
Development and validation of a high-throughput PNAS PLUS transcriptomic biomarker to address 21st century genetic toxicology needs Heng-Hong Lia,b,1, Renxiang Chena,b,c, Daniel R. Hydukea,b, Andrew Williamsd, Roland Frötschle, Heidrun Ellinger-Ziegelbauerf, Raegan O’Loneg, Carole L. Yaukd, Jiri Aubrechth, and Albert J. Fornace Jr.a,b,1 aDepartment of Biochemistry and Molecular & Cellular Biology, Georgetown University Medical Center, Washington, DC 20057; bDepartment of Oncology, Georgetown University Medical Center, Washington, DC 20057; cTrevigen, Inc., Gaithersburg, MD 20877; dEnvironmental Health Science and Research Bureau, Health Canada, Ottawa, ON, Canada K1A 0K9; eFederal Institute for Drugs and Medical Devices, D-53175 Bonn, Germany; fInvestigational Toxicology, Drug Discovery, Pharmaceuticals, Bayer AG, 42096 Wuppertal, Germany; gHealth and Environmental Sciences Institute, International Life Sciences Institute, Washington, DC 20005; and hDrug Safety Research and Development, Pfizer Global Research and Development, Groton, CT 06340 Edited by James E. Cleaver, University of California, San Francisco, CA, and approved November 2, 2017 (received for review August 10, 2017) Interpretation of positive genotoxicity findings using the current in The differentiation of relevant from irrelevant in vitro results vitro testing battery is a major challenge to industry and regulatory is crucial for the interpretation of positive findings in the context agencies. These tests, especially mammalian cell assays, have high of risk to human health. Such irrelevant positive results typically sensitivity but suffer from low specificity, leading to high rates of require expensive and time-consuming follow-up tests involving irrelevant positive findings (i.e., positive results in vitro that are not animal testing. When cost is a consideration, or when animal relevant to human cancer hazard). -

Guidance for Industry S2B Genotoxicity: a Standard Battery for Genotoxicity Testing of Pharmaceuticals
Guidance for Industry S2B Genotoxicity: A Standard Battery for Genotoxicity Testing of Pharmaceuticals July 1997 ICH Guidance for Industry S2B Genotoxicity: A Standard Battery for Genotoxicity Testing of Pharmaceuticals Additional copies are available from: the Drug Information Branch (HFD-210), Center for Drug Evaluation and Research (CDER), 5600 Fishers Lane, Rockville, MD 20857 (Tel) 301-827-4573 http://www.fda.gov/cder/guidance/index.htm or Office of Communication, Training, and Manufacturers Assistance (HFM-40) Center for Biologics Evaluation and Research (CBER) 1401 Rockville Pike, Rockville, MD 20852-1448, http://www.fda.gov/cber/guidelines.htm (Fax) 888-CBERFAX or 301-827-3844 (Voice Information) 800-835-4709 or 301-827-1800 U.S. Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and Research (CDER) Center for Biologics Evaluation and Research (CBER) July 1997 ICH Table of Contents I. INTRODUCTION (1) ..................................................1 II. GENERAL PURPOSE OF GENOTOXICITY TESTING (2) ....................1 III. THE STANDARD TEST BATTERY FOR GENOTOXICITY (3) ................2 IV. MODIFICATIONS OF THE 3-TEST BATTERY (4) ..........................3 A. Limitations to the Use of Bacterial Test Organisms (4.1) ..................4 B. Compounds Bearing Structural Alerts for Genotoxic Activity (4.2) ...........4 C. Limitations to the Use of Standard in Vivo Tests (4.3) ....................4 D. Additional Genotoxicity Testing in Relation to the Carcinogenicity Bioassay (4.4) 4 V. -
Genotoxicity: Mechanisms, Testing Guidelines and Methods
Global journal of Pharmacy & pharmaceutical Science ISSN:2573-2250 Review Article Glob J Pharmaceu Sci Volume 1 Issue 5 - April 2017 DOI: 10.19080/GJPPS.2017.02.555575 Copyright © All rights are reserved by Rajendra SV Genotoxicity: Mechanisms, Testing Guidelines and Methods Mohamed SAKS, Sabita Upreti, Rajendra SV* and Raman Dang Krupanidhi College of Pharmacy, India Submission: March 08, 2017; Published: April 27, 2017 *Corresponding author: Rajendra SV, Department of Pharmacology, Krupanidhi College of Pharmacy, India, Tel: ; Email: Abstract Genotoxicity is one of the major causes for cancer. Genotoxins are agents that can cause the damage of DNA or chromosomal structure thereby causing mutations. It can be chemical or radiation. This damage in the somatic cells will lead to various diseases ranging to cancer prevent the potential damage that can be caused by these genotoxic agents. In this article we discuss about the basic of genotoxicity and the importancewhereas the of damage genotoxic to the studies. germ cell will lead to heritable diseases. Better identification and understanding of genotoxins would enable us to Keywords: Genotoxins, Mutagens, DNA Damage, Chromosomal mutation, Testing guidelines. Introduction [3,4] One of the best ways to control the damage due to mutagens Genotoxicity is a word used in genetics that describes the and carcinogens is to identify the substance or chemical, i.e. possession of substance that has destructive effect on the genetic antimutagens /anticlastogens (which suppress or inhibit the material of the cell (DNA, RNA) thus affecting the integrity of mutagenesis process by directly acting on the cell mechanism) the cell. Genotoxins are mutagens that can cause genotoxicity and demutagens (which destroy or inactivate the mutagens leading to the damage of DNA or chromosomal material thus partially or fully thereby affecting less population of cell) from causing mutation. -
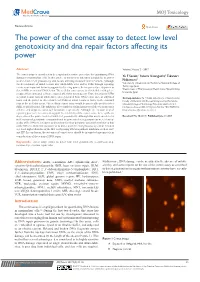
The Power of the Comet Assay to Detect Low Level Genotoxicity and Dna Repair Factors Affecting Its Power
MOJ Toxicology Review Article Open Access The power of the comet assay to detect low level genotoxicity and dna repair factors affecting its power Abstract Volume 3 Issue 2 - 2017 The comet assay is considered to be a rapid and sensitive procedure for quantitating DNA Yu F Sasaki,1 Satomi Kawaguchi,1 Takanori damage in mammalian cells. In this article, to interpret its outcomes adequately, its power 2 to detect low level genotoxicity and factors affecting its power were reviewed. Although Nakamura 1 the development of initial lesions into alkali-labile sites and/or SSBs through repairing Laboratory of Genotoxicity, Hachinohe National College of Technology, Japan events is an important factor to support its detecting power, their repair reduce its power to 2Department of Pharmaceutical Health Care, Himeji Dokkyo detect SSBs as an initial DNA lesion. The acellular comet assay, in which slides with gel are University, Japan prepared from untreated cells are exposed after lysis to test agents. Thus, detection of SSBs as initial lesions but not alkali-labile sites generated from DNA lesion such as alkylated Correspondence: Yu F Sasaki, Laboratory of Genotoxicity, bases and the power to detect low level SSBs as initial lesions is lower in the standard Faculty of Chemical and Biological Engineering, Hachinohe than in the acellular assay. The acellular comet assay would be practically used to detect National College of Technology, Tamonoki Uwanotai16-1, SSBs as initial lesions. The inhibitors of re-synthesis andincisionsteps of the excision repair Hachinohe, Aomori 039-1192, Japan, Tel/ fax +81178277296, enhance and suppress comet-tail formation, respectively. -

Measurements of Polycyclic Aromatic Hydrocarbons and Genotoxicity in Soot Deposited at a Toll Plaza Near Durban, South Africa
RESEARCH ARTICLE S.J. Godefroy, B.S. Martincigh and L.F. Salter, 61 S. Afr. J. Chem., 2005, 58, 61–66, <http://journals.sabinet.co.za/sajchem/>. Measurements of Polycyclic Aromatic Hydrocarbons and Genotoxicity in Soot Deposited at a Toll Plaza near Durban, South Africa Susan J. Godefroy, Bice S. Martincigh* and Leo F. Salter‡ School of Chemistry, University of KwaZulu-Natal, Howard College Campus, Durban, 4041 South Africa. Received 18 October 2004; revised and accepted 30 March 2005 ABSTRACT This research was designed to examine the presence of polycyclic aromatic hydrocarbons (PAHs) in soot deposited at the Mariannhill toll plaza situated on the N3 highway in KwaZulu-Natal, South Africa. Samples were collected from the toll plaza either by scraping the toll booth walls and surrounding areas, or by wiping the surfaces with cotton wool swabs. The organic component was separated by ultrasonic extraction into dichloromethane and analysed for PAHs by reverse phase high performance liquid chromatography with both fluorescence and ultraviolet detection. The genotoxicity was investigated by means of two bacterial assays: the Ames test and the SOS Chromotest. A number of PAHs were identified and genotoxic activity was observed in both of the assays. KEYWORDS Polycyclic aromatic hydrocarbons, toll plaza, genotoxicity. 1. Introduction mutagenicity.8–10 Since a toll plaza is an area of high traffic Polycyclic aromatic hydrocarbons (PAHs) are ubiquitous density, it is an ideal location for an investigation into the environmental pollutants that are of health concern because of build-up of particles emitted by vehicles, and for a study of the their mutagenic and carcinogenic properties. -

Guidance Document on Revisions to OECD Genetic Toxicology Test Guidelines TABLE of CONTENTS
Genetic Toxicology Guidance Document: Second Commenting Round. Nov 30, 2015 Guidance Document on Revisions to OECD Genetic Toxicology Test Guidelines TABLE OF CONTENTS 1 GENERAL INTRODUCTION (PREAMBLE) ........................................................................................................................................ 3 1.1 GENERAL BACKGROUND ............................................................................................................................................................. 3 1.2 HISTORY AND STATUS OF TGS ................................................................................................................................................... 4 2 AIM OF GENETIC TOXICOLOGY TESTING ......................................................................................................................................... 6 2.1 GENETIC TOXICOLOGY ENDPOINTS ............................................................................................................................................ 7 3 TEST GUIDELINES FOR GENETIC TOXICOLOGY .............................................................................................................................. 8 3.1 IN VITRO GENETIC TOXICOLOGY TESTS ....................................................................................................................................... 9 3.1.1 Tests for gene mutations ................................................................................................................................................ -

N-Acetylcysteine Promotes DNA Repair After Genotoxic Damage Induced by Copper Sulphate in Human Lymphocytes
Research Article ISSN: 2574 -1241 DOI: 10.26717/BJSTR.2020.29.004776 N-Acetylcysteine Promotes DNA Repair after Genotoxic Damage Induced by Copper Sulphate in Human Lymphocytes Edgardo Becerra, Karla Padilla, Laura C Berumen and Guadalupe García Alcocer* Faculty of Chemistry, Autonomous University of Querétaro, University Center, Mexico *Corresponding author: Guadalupe García Alcocer, Faculty of Chemistry, Autonomous University of Querétaro, University Center, Mexico ARTICLE INFO AbsTRACT Received: July 16, 2020 DNA damage may be induced by high reactive oxygen species levels and is related to cancer, amongst many diseases. Previous studies have shown that the excess of Published: August 03, 2020 copper in cells increases the reactive oxygen species. Moreover, oxidative stress also diminishes the DNA repair enzymes, activity, hence, increasing cancer risk. There are existing reports about the role of N-acetylcysteine in DNA protection related to Citation: Edgardo B, Karla P, Laura its antioxidant activity; however, its role in DNA repair has not been studied. In the C Berumen, Guadalupe García A. present work, the DNA repair by N-acetylcysteine was analyzed through the comet N-Acetylcysteine Promotes DNA Repair assay in human lymphocytes after inducing genotoxicity by means of copper sulphate. after Genotoxic Damage Induced by The gathered data indicates that N- acetylcysteine is innocuous at 1000 µM and Copper Sulphate in Human Lymphocytes. Biomed J Sci & Tech Res 29(2)-2020. BJSTR. treated with Cu2SO4, while N-acetylcysteine exerted