Open Full Page
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Alemtuzumab Comparison with Rituximab and Leukemia Whole
Mechanism of Action of Type II, Glycoengineered, Anti-CD20 Monoclonal Antibody GA101 in B-Chronic Lymphocytic Leukemia Whole Blood Assays in This information is current as Comparison with Rituximab and of September 27, 2021. Alemtuzumab Luca Bologna, Elisa Gotti, Massimiliano Manganini, Alessandro Rambaldi, Tamara Intermesoli, Martino Introna and Josée Golay Downloaded from J Immunol 2011; 186:3762-3769; Prepublished online 4 February 2011; doi: 10.4049/jimmunol.1000303 http://www.jimmunol.org/content/186/6/3762 http://www.jimmunol.org/ Supplementary http://www.jimmunol.org/content/suppl/2011/02/04/jimmunol.100030 Material 3.DC1 References This article cites 44 articles, 24 of which you can access for free at: http://www.jimmunol.org/content/186/6/3762.full#ref-list-1 by guest on September 27, 2021 Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2011 by The American -

Alemtuzumab Comparison with Rituximab and Leukemia Whole
Mechanism of Action of Type II, Glycoengineered, Anti-CD20 Monoclonal Antibody GA101 in B-Chronic Lymphocytic Leukemia Whole Blood Assays in This information is current as Comparison with Rituximab and of September 29, 2021. Alemtuzumab Luca Bologna, Elisa Gotti, Massimiliano Manganini, Alessandro Rambaldi, Tamara Intermesoli, Martino Introna and Josée Golay Downloaded from J Immunol 2011; 186:3762-3769; Prepublished online 4 February 2011; doi: 10.4049/jimmunol.1000303 http://www.jimmunol.org/content/186/6/3762 http://www.jimmunol.org/ Supplementary http://www.jimmunol.org/content/suppl/2011/02/04/jimmunol.100030 Material 3.DC1 References This article cites 44 articles, 24 of which you can access for free at: http://www.jimmunol.org/content/186/6/3762.full#ref-list-1 by guest on September 29, 2021 Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2011 by The American -

Horizon Scanning Status Report June 2019
Statement of Funding and Purpose This report incorporates data collected during implementation of the Patient-Centered Outcomes Research Institute (PCORI) Health Care Horizon Scanning System, operated by ECRI Institute under contract to PCORI, Washington, DC (Contract No. MSA-HORIZSCAN-ECRI-ENG- 2018.7.12). The findings and conclusions in this document are those of the authors, who are responsible for its content. No statement in this report should be construed as an official position of PCORI. An intervention that potentially meets inclusion criteria might not appear in this report simply because the horizon scanning system has not yet detected it or it does not yet meet inclusion criteria outlined in the PCORI Health Care Horizon Scanning System: Horizon Scanning Protocol and Operations Manual. Inclusion or absence of interventions in the horizon scanning reports will change over time as new information is collected; therefore, inclusion or absence should not be construed as either an endorsement or rejection of specific interventions. A representative from PCORI served as a contracting officer’s technical representative and provided input during the implementation of the horizon scanning system. PCORI does not directly participate in horizon scanning or assessing leads or topics and did not provide opinions regarding potential impact of interventions. Financial Disclosure Statement None of the individuals compiling this information have any affiliations or financial involvement that conflicts with the material presented in this report. Public Domain Notice This document is in the public domain and may be used and reprinted without special permission. Citation of the source is appreciated. All statements, findings, and conclusions in this publication are solely those of the authors and do not necessarily represent the views of the Patient-Centered Outcomes Research Institute (PCORI) or its Board of Governors. -

Cancer Drug Shortages: Who's Minding the Store?
✽ ✽ [ News ✽ Analysis ✽ Commentary ✽ Controversy ] February 25, 2011 Vol. 33 No. 4 oncology-times.com Publishing for O33 Years NCOLOGY The Independent TIMES Hem/Onc News Source Cancer Drug Shortages: Who’s Minding the Store? he recent shortages of certain chemotherapy agents and other key drugs raise Tquestions about who’s in charge of the national drug supply and how to ensure availability when there are limited fi nancial incentives and no mandates that manu- facturers notify the FDA about upcoming shortages. Here’s what experts are saying. Page 25 iStockphoto.com/klenova ASCO: For Patients with Advanced Cancer, Start Frank Talks about Options Soon after Diagnosis p.22 iStockphoto.com ODAC Backs FDA on Post-Marketing Medical Home Concept Comes Studies for Accelerated-Approval to Oncology p.45 Drugs p.8 [ ALSO ] SHOP TALK . 4 JOE SIMONE: The Self-Referral Boom . .15 MIKKAEL SEKERES: On (cology) Language . .16 Colorectal Cancer: Best to Start Chemo by 4 Weeks After Surgery . 18 Breast Cancer: 4 Cycles of Adjuvant Chemo Usually Suffi cient . 36 WENDY HARPHAM: ‘It’s OK’. 40 POETRY BY CANCER CAREGIVERS . 47 Ph+ ALL: Early Use of Imatinib Extends Long-Term Survival. 49 Twitter.com/OncologyTimes PERIODICALS bitly.com/oncologytimes 9 oncology times Saturating Liver Cancers with Chemotherapy Found to Extend Survival & Decrease Toxicity athing liver tumors in chemo- The study included 93 patients: said Charles Nutting, DO, FSIR, an Btherapy increases survival, accord- 44 received PHP and 49 had interventional radiologist at Swedish ing to a Phase III trial reported at the standard treatment (typically systemic Medical Center in Denver. -

Structure–Function Relationships of the Variable Domains of Monoclonal
Critical Reviews in Oncology/Hematology 64 (2007) 210–225 Structure–function relationships of the variable domains of monoclonal antibodies approved for cancer treatment Charlotte Magdelaine-Beuzelin a,b, Quentin Kaas c, Vanessa Wehbi a, Marc Ohresser a, Roy Jefferis d, Marie-Paule Lefranc c, Herve´ Watier a,b,∗ a Universit´eFran¸cois Rabelais de Tours, EA 3853 “Immuno-Pharmaco-G´en´etique des Anticorps th´erapeutiques”, France b CHRU de Tours, Laboratoire d’Immunologie, France c IMGT, Laboratoire d’ImmunoG´en´etique Mol´eculaire, LIGM, Institut de G´en´etique Humaine, UPR CNRS 1142, Montpellier, France d Immunity and Infection, University of Birmingham, United Kingdom Accepted 20 April 2007 Contents 1. Chimeric and humanized antibodies .................................................................................... 211 2. IMGT Collier de Perles ............................................................................................... 217 3. Antibody/antigen interactions.......................................................................................... 219 4. Variable domain genetic analysis....................................................................................... 220 5. Immunogenicity...................................................................................................... 222 Reviewers ........................................................................................................... 223 Acknowledgements.................................................................................................. -

Whither Radioimmunotherapy: to Be Or Not to Be? Damian J
Published OnlineFirst April 20, 2017; DOI: 10.1158/0008-5472.CAN-16-2523 Cancer Perspective Research Whither Radioimmunotherapy: To Be or Not To Be? Damian J. Green1,2 and Oliver W. Press1,2,3 Abstract Therapy of cancer with radiolabeled monoclonal antibodies employing multistep "pretargeting" methods, particularly those has produced impressive results in preclinical experiments and in utilizing bispecific antibodies, have greatly enhanced the thera- clinical trials conducted in radiosensitive malignancies, particu- peutic efficacy of radioimmunotherapy and diminished its toxi- larly B-cell lymphomas. Two "first-generation," directly radiola- cities. The dramatically improved therapeutic index of bispecific beled anti-CD20 antibodies, 131iodine-tositumomab and 90yttri- antibody pretargeting appears to be sufficiently compelling to um-ibritumomab tiuxetan, were FDA-approved more than a justify human clinical trials and reinvigorate enthusiasm for decade ago but have been little utilized because of a variety of radioimmunotherapy in the treatment of malignancies, particu- medical, financial, and logistic obstacles. Newer technologies larly lymphomas. Cancer Res; 77(9); 1–6. Ó2017 AACR. "To be, or not to be, that is the question: Whether 'tis nobler in the pembrolizumab (anti-PD-1), which are not directly cytotoxic mind to suffer the slings and arrows of outrageous fortune, or to take for cancer cells but "release the brakes" on the immune system, arms against a sea of troubles, And by opposing end them." Hamlet. allowing cytotoxic T cells to be more effective at recognizing –William Shakespeare. and killing cancer cells. Outstanding results have already been demonstrated with checkpoint inhibiting antibodies even in far Introduction advanced refractory solid tumors including melanoma, lung cancer, Hodgkin lymphoma and are under study for a multi- Impact of monoclonal antibodies on the field of clinical tude of other malignancies (4–6). -

Monoclonal Antibodies
MONOCLONAL ANTIBODIES ALEMTUZUMAB ® (CAMPATH 1H ) I. MECHANISM OF ACTION Antibody-dependent lysis of leukemic cells following cell surface binding. Alemtuzumab is a recombinant DNA-derived humanized monoclonal antibody that is directed against surface glycoprotein CD52. CD52 is expressed on the surface of normal and malignant B and T lymphocytes, NK cells, monocytes, macrophages, a subpopulation of granulocytes, and tissues of the male reproductive system (CD 52 is not expressed on erythrocytes or hematopoietic stem cells). The alemtuzumab antibody is an IgG1 kappa with human variable framework and constant regions, and complementarity-determining regions from a murine monoclonal antibody (campath 1G). II. PHARMACOKINETICS Cmax and AUC show dose proportionality over increasing dose ranges. The overall average half-life is 12 days. Peak and trough levels of Campath rise during the first weeks of Campath therapy, and approach steady state by week 6. The rise in serum Campath concentration corresponds with the reduction in malignant lymphocytes. III. DOSAGE AND ADMINISTRATION Campath can be administered intravenously or subcutaneously. Intravenous: Alemtuzumab therapy should be initiated at a dose of 3 mg administered as a 2-hour IV infusion daily. When the 3 mg dose is tolerated (i.e., ≤ Grade 2 infusion related side effects), the daily dose should be escalated to 10mg and continued until tolerated (i.e., ≤ Grade 2 infusion related side effects). When the 10 mg dose is tolerated, the maintenance dose of 30 mg may be initiated. The maintenance dose of alemtuzumab is 30 mg/day administered three times a week on alternate days (i.e. Monday, Wednesday, and Friday), for up to 12 weeks. -

Hodgkin's Lymphoma Unresponsive to Rituximab Or a Rituximab
Clinical Development GSK1841157 Protocol OMB110918 / NCT01077518 A Randomized, Open Label Study of Ofatumumab and Bendamustine Combination Therapy Compared with Bendamustine Monotherapy in Indolent B-cell Non- Hodgkin’s Lymphoma Unresponsive to Rituximab or a Rituximab-Containing Regimen During or Within Six Months of Treatment Authors Document type Amended Protocol Version EUDRACT number 2008-004177-17 Version number 11 Development phase III Document status Final Release date 13-Apr-2017 Novartis internal reference number COMB157E2301 Property of Novartis Confidential May not be used, divulged, published, or otherwise disclosed without the consent of Novartis Novartis Confidential Page 2 Amended Protocol Version 11 Clean Protocol No. COMB157E2301/OMB110918 Amendment 9 (13-Apr-2017) Amendment rationale The purpose of amendment 9 is to revise the total number of events required for the primary analysis of the primary end point PFS. The primary analysis was planned after reaching 259 PFS events as determined by an Independent Review Committee (IRC). Based on the current status of the study and PFS event count by IRC, it is highly unlikely that the 259 PFS events will be achieved. The study has been ongoing since September 2010 when the first patient was enrolled and the study sponsorship changed in February 2016 from GSK to Novartis (Amendment 8 , dated 18Mar2016). Per protocol, Interim Analysis for efficacy and futility and IDMC review occurred (22Feb2016) after 180 PFS events by IRC were reached (31Oct2015). IDMC recommended to continue the study without changes. The interim analysis of PFS was performed by an independent Statistical Data Analysis Centre. As per IDMC charter, unblinded results were not communicated to the sponsor in order to maintain the integrity of the trial. -

A Novel Raji-Burkitt's Lymphoma Model for Preclinical and Mechanistic Evaluation of CD52-Targeted Immunotherapeutic Agents
Cancer Therapy: Preclinical A Novel Raji-Burkitt’s Lymphoma Model for Preclinical and Mechanistic Evaluation of CD52-Targeted Immunotherapeutic Agents Rosa Lapalombella,1Xiaobin Zhao,1, 2 Georgia Triantafillou,1Bo Yu,3,4 Yan Jin, 4 Gerard Lozanski,5 Carolyn Cheney,1Nyla Heerema,5 David Jarjoura,6 Amy Lehman,6 L. James Lee,3,4 Guido Marcucci,1Robert J. Lee,2,4 Michael A. Caligiuri,1 Natarajan Muthusamy,1and John C. Byrd1, 2 Abstract Purpose:Todate, efforts to study CD52-targeted therapies, such as alemtuzumab, have beenlim- ited due to the lack of stable CD52 expressing transformed B-cell lines and animal models.We describe generation and utilization of cell lines that stably express CD52 both in vitro and in vivo. Experimental Design: By limiting dilution, we have established several clones of Raji-Burkitt’s lymphoma cell line that express surface CD52. Immunophenotype and cytogenetic charac- terizationof these clones was done. In vivo usefulness of the CD52high cell line to evaluate the ther- apeuticefficacyofCD52-directedantibody wasinvestigatedusingaSCIDmousexenograftmodel. Results: Stable expression of CD52 was confirmed in cells cultured in vitro up to 52 weeks of continuous growth. The functional integrity of the expressed CD52 molecule was shown using alemtuzumab, which induced cytotoxic effects in vitro in the CD52high but not the CD52low clone. Compared with control antibody, alemtuzumab treatment in CD52high inoculated mice resulted in significantly increased median survival. Comparable levels of CD52-targeted direct cyto- toxicity, complement-dependent cytotoxicity, and antibody-dependent cytotoxicity and anti-CD52 immunoliposome-mediated delivery of synthetic oligodeoxyribo nucleotides in CD52high clone and primary B-chronic lymphocytic leukemia cells implicated potential in vivo application of this model for evaluation of CD52-targeted antibody and immunoliposomes encapsulating therapeutic agents. -

Cetuximab Promotes Anticancer Drug Toxicity in Rhabdomyosarcomas with EGFR Amplificationin Vitro
ONCOLOGY REPORTS 30: 1081-1086, 2013 Cetuximab promotes anticancer drug toxicity in rhabdomyosarcomas with EGFR amplificationin vitro YUKI YAMAMOTO1*, KAZUMASA FUKUDA2*, YASUSHI FUCHIMOTO4*, YUMI MATSUZAKI3, YOSHIRO SAIKAWA2, YUKO KITAGAWA2, YASUHIDE MORIKAWA1 and TATSUO KURODA1 Departments of 1Pediatric Surgery, 2Surgery and 3Physiology, Keio University School of Medicine, Tokyo 160-858; 4Division of Surgery, Department of Surgical Subspecialities, National Center for Child Health and Development, Tokyo 157-8535, Japan Received January 15, 2013; Accepted April 2, 2013 DOI: 10.3892/or.2013.2588 Abstract. Overexpression of human epidermal growth factor i.e., t(2;13) (q35;q14) in 55% of cases and t(1;13) (p36;q14) in receptor (EGFR) has been detected in various tumors and is 22% of cases (1). Current treatment options include chemo- associated with poor outcomes. Combination treatment regi- therapy, complete surgical resection and radiotherapy (3). mens with EGFR-targeting and cytotoxic agents are a potential However, the prognosis for patients with advanced-stage RMS therapeutic option for rhabdomyosarcoma (RMS) with EGFR is quite poor (4). The main problems with clinical treatments amplification. We investigated the effects of combination include metastatic invasion, local tumor recurrence and multi- treatment with actinomycin D and the EGFR-targeting agent drug resistance. Therefore, more specific, effective and less cetuximab in 4 RMS cell lines. All 4 RMS cell lines expressed toxic therapies are required. wild-type K-ras, and 2 of the 4 overexpressed EGFR, as Numerous novel anticancer agents are currently in early determined by flow cytometry, real-time PCR and direct phase clinical trials. Of these, immunotherapy with specific sequencing. -
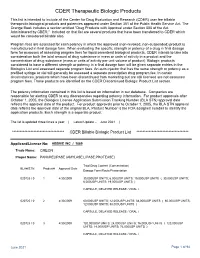
CDER Therapeutic Biologic Products List
CDER Therapeutic Biologic Products This list is intended to include all the Center for Drug Evaluation and Research (CDER) user fee billable therapeutic biological products and potencies approved under Section 351 of the Public Health Service Act. The Orange Book includes a section entitled "Drug Products with Approval under Section 505 of the Act Administered by CBER." Included on that list are several products that have been transferred to CDER which would be considered billable also. Program fees are assessed for each potency in which the approved (non-revoked, non-suspended) product is manufactured in final dosage form. When evaluating the specific strength or potency of a drug in final dosage form for purposes of assessing program fees for liquid parenteral biological products, CDER intends to take into consideration both the total amount of drug substance in mass or units of activity in a product and the concentration of drug substance (mass or units of activity per unit volume of product). Biologic products considered to have a different strength or potency in a final dosage form will be given separate entries in the Biologics List and assessed separate program fees. An auto-injector that has the same strength or potency as a prefilled syringe or vial will generally be assessed a separate prescription drug program fee. In certain circumstances, products which have been discontinued from marketing but are still licensed are not assessed program fees. Those products are identified on the CDER Discontinued Biologic Product List section. The potency information contained in this list is based on information in our database. -

Antibodies for the Treatment of Brain Metastases, a Dream Or a Reality?
pharmaceutics Review Antibodies for the Treatment of Brain Metastases, a Dream or a Reality? Marco Cavaco, Diana Gaspar, Miguel ARB Castanho * and Vera Neves * Instituto de Medicina Molecular, Faculdade de Medicina, Universidade de Lisboa, Av. Prof. Egas Moniz, 1649-028 Lisboa, Portugal * Correspondence: [email protected] (M.A.R.B.C.); [email protected] (V.N.) Received: 19 November 2019; Accepted: 28 December 2019; Published: 13 January 2020 Abstract: The incidence of brain metastases (BM) in cancer patients is increasing. After diagnosis, overall survival (OS) is poor, elicited by the lack of an effective treatment. Monoclonal antibody (mAb)-based therapy has achieved remarkable success in treating both hematologic and non-central-nervous system (CNS) tumors due to their inherent targeting specificity. However, the use of mAbs in the treatment of CNS tumors is restricted by the blood–brain barrier (BBB) that hinders the delivery of either small-molecules drugs (sMDs) or therapeutic proteins (TPs). To overcome this limitation, active research is focused on the development of strategies to deliver TPs and increase their concentration in the brain. Yet, their molecular weight and hydrophilic nature turn this task into a challenge. The use of BBB peptide shuttles is an elegant strategy. They explore either receptor-mediated transcytosis (RMT) or adsorptive-mediated transcytosis (AMT) to cross the BBB. The latter is preferable since it avoids enzymatic degradation, receptor saturation, and competition with natural receptor substrates, which reduces adverse events. Therefore, the combination of mAbs properties (e.g., selectivity and long half-life) with BBB peptide shuttles (e.g., BBB translocation and delivery into the brain) turns the therapeutic conjugate in a valid approach to safely overcome the BBB and efficiently eliminate metastatic brain cells.