Space-Time Patterns, Change, and Propagation of COVID-19 Risk Relative to the Intervention Scenarios in Bangladesh
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

12. FORMULATION of the URBAN TRANSPORT MASTER PLAN Development of the RSTP Urban Transportation Master Plan (1) Methodology
The Project on The Revision and Updating of the Strategic Transport Plan for Dhaka (RSTP) Final Report 12. FORMULATION OF THE URBAN TRANSPORT MASTER PLAN Development of the RSTP Urban Transportation Master Plan (1) Methodology The development of the RSTP Urban Transportation Master Plan adopted the following methodology (see Figure 12.1): (i) Elaborate the master plan network through a screen line analysis by comparing the network capacity and future demand. (ii) Identify necessary projects to meet future demand at the same time avoiding excessive capacity. (iii) Conducts economic evaluation of each project to give priority on projects with higher economic return. (iv) Conduct preliminary environmental assessment of every project and consider countermeasures against environmental problems, if any. (v) Make a final prioritization of all physical projects by examining their respective characteristics from different perspectives. (vi) Classify the projects into three categories, namely short-, medium- and long-term projects, by considering the financial constraints. (vii) Prepare an action plan for short-term projects together with “soft” measures. Mid-term Project Source: RSTP Study Team Figure 12.1 Development Procedure for the Master Plan 12-1 The Project on The Revision and Updating of the Strategic Transport Plan for Dhaka (RSTP) Final Report (2) Output of the Transportation Network Plan The RSTP urban transportation network plan was developed based on a review and a modification of the STP network plan. The main points of the modification or adoption of the STP network master plan are as follows: i. Harmonization with future urban structure, land-use plan and development of network plan. -
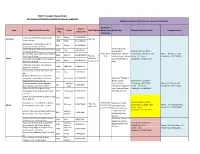
BRAC Transport Department Information of Pick & Drop Vehicle for Special Assignment Additional Vehicles Plan & Concern Person Information
BRAC Transport Department Information of Pick & Drop Vehicle for special assignment Additional vehicles plan & Concern person Information Additional Vehicle Driver's Area Regular PnD Route Plan Driver Staff Vehicle Vehicle from Route Plan Vehicle No & Driver Info Concern Person Reg. Contact No. Outsource Tongi Dottopara-Army Stadium-Start 1127 Shokat 01729070685 Dattapara *Bus: 02 Time: 7:45 am 1128 Mizan 01727920441 Abdullahpur-Khilkhet-Banani-Army 539 Raihan 01714062691 Stadium-Start Time: 7:45 am Uttara Ranabola-Khilkhet-Army Stadium- Route # 01*Tongi 9755 Tipu 1939115219 Start Time: 7:45 am College Gate- Starting Time : 07:30 am Baratero Mor, Jasimuddin-Army Stadium- 01 Bus (From Abdullahpur- Airport- Vehicle Reg. : DM-SA-11-218 Name : Mr. Rasel-1, BU 9286 Donesh 017130348237 Start Time: 7:45 am *Bus:01 * BU) Khilkhet-Army Stadium Name : Mr. Rejaul Mobile No : 01947706553 Uttara BRAC Polli 3, Kachabazar-Army Stadium- Micro: 05 * (As per Staff Pick Up Mobile No : 01719755469 5205 Ripon 01729070513 Start Time: 7:45 am Sedan Car: 01 time) Uttara Sec-13,Airport-Army Stadium - 5208 Abdul Jalil 1729070791 Start Time: 7:45 am Uttara-Army Stadium- Start time: 7:45 1416 Dipa 1729070604 am Al Arafah Bank-City Club-Purobi Mor- Sangbadik Colony-Kalshi-ECB-Army 0141 Saiful Islam 01729070566 Route # 02 * Mirpur 1- Stadium-Start Time:7:50 am Bangla College- Starting Time : 07:50 am Al Helal Hospital-Kajipara-Agargaon- Humaun Technical Mor- Vehicle Reg : BRTC-5395 Name : Mr. Mustafa ,BU 211 1713052822 Army Stadium-Start Time:7:50 am Kabir Kallayanpur-Agargaon- Name : Mr. Mizan Mobile No : 01941548063 Mirpur Model Thana-Ansar Camp- Army Stadium (As per Mobile No : 01798289307 Kallayanpur-Army Stadium-Start Time: 0123 Dilip Nayek 01713052743 Staff Pick Up time) 7:45 am Sheyal bari-Stadium-Army Stadium- Start 4147 Parimal 1704120689 Time: 8:00 am Starting Time : 07:50 am Shiyalbari mor, Proshikha Mor- 60feet- 03 Buses (02 Route # 03 *Heart 5204 Ali Azom 01745774663 * Bus- 03 Vehicle Reg : 11-9682 (BU) Name : Mr. -
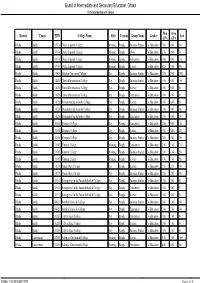
Board of Intermediate and Secondary Education, Dhaka SVG Information of Colleges
Board of Intermediate and Secondary Education, Dhaka SVG Information of Colleges District Thana EIIN College Name Shift Version Group Name Gender Min Own Seat GPA GPA Dhaka Badda 107974 Dhaka Imperial College Morning Bangla Business Studies Co-Education 3.00 0.00 650 Dhaka Badda 107974 Dhaka Imperial College Morning Bangla Music Co-Education 2.50 0.00 50 Dhaka Badda 107974 Dhaka Imperial College Morning Bangla Humanities Co-Education 3.00 0.00 120 Dhaka Badda 107974 Dhaka Imperial College Morning Bangla Science Co-Education 4.25 0.00 900 Dhaka Badda 131904 Gulshan Commerce College Day Bangla Business Studies Co-Education 2.00 0.00 1000 Dhaka Badda 134620 Harvard International College Day Bangla Business Studies Co-Education 1.00 0.00 100 Dhaka Badda 134620 Harvard International College Day Bangla Science Co-Education 1.00 0.00 50 Dhaka Badda 134620 Harvard International College Day Bangla Humanities Co-Education 1.00 0.00 50 Dhaka Badda 134228 Mohammedbag Adorsho College Day Bangla Science Co-Education 1.00 0.00 50 Dhaka Badda 134228 Mohammedbag Adorsho College Day Bangla Business Studies Co-Education 1.00 0.00 100 Dhaka Badda 134228 Mohammedbag Adorsho College Day Bangla Humanities Co-Education 1.00 0.00 100 Dhaka Badda 136858 Monpura College Day Bangla Humanities Co-Education 2.00 0.00 150 Dhaka Badda 136858 Monpura College Day Bangla Science Co-Education 3.00 0.00 150 Dhaka Badda 136858 Monpura College Day Bangla Business Studies Co-Education 2.00 0.00 200 Dhaka Badda 131945 National College Morning Bangla Humanities Co-Education 2.00 -

127 Branches
মেটলাইফ পলললির প্রিপ্রিয়াি ও অꇍযাꇍয মপমেন্ট বযা廬ক এপ্রিয়ার িকল শাখায় ꇍগদে প্রদান কমর তাৎক্ষপ্রিকভাদব বমু ে লনন ররপ্রভপ্রꇍউ স্ট্যাম্প ও সীলসহ রিটলাইদের প্ররপ্রসট এই িলু বধা পাওয়ার জনয গ্রাহকমক মকান অলিলরক্ত লফ অথবা স্ট্যাম্প চাজ জ প্রদান করমি হমব না Sl. No. Division District Name of Branches Address of Branch 1 Barisal Barisal Barishal Branch Fakir Complex 112 Birshrashtra Captain Mohiuddin Jahangir Sarak 2 Barisal Bhola Bhola Branch Nabaroon Center(1st Floor), Sadar Road, Bhola 3 Chittagong Chittagong Agrabad Branch 69, Agrabad C/ A, Chittagong 4 Chittagong Chittagong Anderkilla Branch 184, J.M Sen Avenue Anderkilla 5 Chittagong Chittagong Bahadderhat Branch Mamtaz Tower 4540, Bahadderhat 6 Chittagong Chittagong Bank Asia Bhaban Branch 39 Agrabad C/A Manoda Mansion (2nd Floor), Holding No.319, Ward No.3, College 7 Chittagong Comilla Barura Branch Road, Barura Bazar, Upazilla: Barura, District: Comilla. 8 Chittagong Chittagong Bhatiary Branch Bhatiary, Shitakunda 9 Chittagong Brahmanbaria Brahmanbaria Branch "Muktijoddha Complex Bhaban" 1061, Sadar Hospital Road 10 Chittagong Chittagong C.D.A. Avenue Branch 665 CDA Avenue, East Nasirabad 1676/G/1 River City Market (1st Floor), Shah Amant Bridge 11 Chittagong Chaktai Chaktai Branch connecting road 12 Chittagong Chandpur Chandpur Branch Appollo Pal Bazar Shopping, Mizanur Rahman Road 13 Chittagong Lakshmipur Chandragonj Branch 39 Sharif Plaza, Maddho Bazar, Chandragonj, Lakshimpur 14 Chittagong Noakhali Chatkhil Branch Holding No. 3147 Khilpara Road Chatkhil Bazar Chatkhil 15 Chittagong Comilla Comilla Branch Chowdhury Plaza 2, House- 465/401, Race Course 16 Chittagong Comilla Companigonj Branch Hazi Shamsul Hoque Market, Companygonj, Muradnagar J.N. -

Division Zila Upazila Name of Upazila/Thana 10 10 04 10 04
Geo Code list (upto upazila) of Bangladesh As On March, 2013 Division Zila Upazila Name of Upazila/Thana 10 BARISAL DIVISION 10 04 BARGUNA 10 04 09 AMTALI 10 04 19 BAMNA 10 04 28 BARGUNA SADAR 10 04 47 BETAGI 10 04 85 PATHARGHATA 10 04 92 TALTALI 10 06 BARISAL 10 06 02 AGAILJHARA 10 06 03 BABUGANJ 10 06 07 BAKERGANJ 10 06 10 BANARI PARA 10 06 32 GAURNADI 10 06 36 HIZLA 10 06 51 BARISAL SADAR (KOTWALI) 10 06 62 MHENDIGANJ 10 06 69 MULADI 10 06 94 WAZIRPUR 10 09 BHOLA 10 09 18 BHOLA SADAR 10 09 21 BURHANUDDIN 10 09 25 CHAR FASSON 10 09 29 DAULAT KHAN 10 09 54 LALMOHAN 10 09 65 MANPURA 10 09 91 TAZUMUDDIN 10 42 JHALOKATI 10 42 40 JHALOKATI SADAR 10 42 43 KANTHALIA 10 42 73 NALCHITY 10 42 84 RAJAPUR 10 78 PATUAKHALI 10 78 38 BAUPHAL 10 78 52 DASHMINA 10 78 55 DUMKI 10 78 57 GALACHIPA 10 78 66 KALAPARA 10 78 76 MIRZAGANJ 10 78 95 PATUAKHALI SADAR 10 78 97 RANGABALI Geo Code list (upto upazila) of Bangladesh As On March, 2013 Division Zila Upazila Name of Upazila/Thana 10 79 PIROJPUR 10 79 14 BHANDARIA 10 79 47 KAWKHALI 10 79 58 MATHBARIA 10 79 76 NAZIRPUR 10 79 80 PIROJPUR SADAR 10 79 87 NESARABAD (SWARUPKATI) 10 79 90 ZIANAGAR 20 CHITTAGONG DIVISION 20 03 BANDARBAN 20 03 04 ALIKADAM 20 03 14 BANDARBAN SADAR 20 03 51 LAMA 20 03 73 NAIKHONGCHHARI 20 03 89 ROWANGCHHARI 20 03 91 RUMA 20 03 95 THANCHI 20 12 BRAHMANBARIA 20 12 02 AKHAURA 20 12 04 BANCHHARAMPUR 20 12 07 BIJOYNAGAR 20 12 13 BRAHMANBARIA SADAR 20 12 33 ASHUGANJ 20 12 63 KASBA 20 12 85 NABINAGAR 20 12 90 NASIRNAGAR 20 12 94 SARAIL 20 13 CHANDPUR 20 13 22 CHANDPUR SADAR 20 13 45 FARIDGANJ -

Shariff Phd Thesis.Pdf
SHAHBAG, A CRITICAL SOCIAL MOMENT: A COLLECTIVE AGENCY CAPABILITIES ANALYSIS By Razia Shariff Canterbury Christ Church University Thesis submitted For the Degree of Doctor of Philosophy 2019 ii ABSTRACT This thesis sets out an approach to understanding the impact of change oriented ‘social moments’ on social practices and structures. The empirical case on which the thesis draws to develop this argument is the Shahbag protests in Bangladesh. At the theoretical level, the thesis suggests that ‘Social Moments’ oriented to change (as differentiated from social movements) can be triggered by latent injustices occurring within a given society. Using a Critical Theoretical lens and the Capability Approach, the thesis sets out a Being-Doing-Impact Model oriented to an understanding of the conditions necessary for a Social Moment to occur. These moments occur where individuals from different parts of the social habitus come together, to create a scene, as a critical mass in order to effect change. Such moments can lead to shifts in systems and practices, and ultimately to a more just society. The research assesses in detail the conditions that made the Shahbag Moment possible. These conditions include: the presence of the necessary agency capabilities of individuals; the effective mobilisation of instrumental freedoms; the substantive presence of networks of social support and solidarity (all of which bring into play an important affective dimension). The wider social context is also viewed as a crucial component. The thesis shows how, for example, the atmosphere at Shahbag can be considered as cultural, positive and safe. It also shows a willingness on the part of Government to listen and respond to the will of the people. -

The Business Review - Special Issue Volume 5, Special Issue, 2016, ISSN 1996-3637
rhe BUSInGSS Reuieur Journal of School of Business Volume 5, SPecial lssue,2016 UrtaRAUxrvERsrTY The Business Review - Special Issue Volume 5, Special Issue, 2016, ISSN 1996-3637 Chief Patron Patron Professor Dr. M Azizur Rahman Professor Dr. Eaysmin Ara Lekha Vice Chancellor, Uttara University Pro-Vice Chancellor, Uttara University Dhaka, Bangladesh Dhaka, Bangladesh International Advisory Board Dr. Luka Powanga Dr. Serajul Islam Bhuiyan Professor Professor & Head of the DePartment, School of Management, Regis University School of Liberal Arts Denver, Colaado, USA Auburn University Alabama, USA Dr. Prithvi Yadav Dr. Haripada Bhattacharjee Professor & Director Professor, Departrnent of Marketing Birla Institute of Management Technology University of Dhaka, Bangladesh Vhubaneswar, Udidha, India Dr. Anwar Hossain Dr. Raliqul Islam Professor of Business Management & Vice-Chancellor Professor, Northern University Department of Banking and Insurance Dhaka, Bangladesh University of Dhaka, Bangladesh Dr. Shaliqur Rahman Dr.Ezaz Ahmed Vice-President Head of Discipline, HRM Australian Academy of Business Leadership (AABL) Central Queensland University, Australia Australia Editorial Board Guest Editor: ProfessorDr. Ziaul Huq, University ofNebraska at Omaha, USA Dr. Nazrul Islam, Professor of Management and Dean, School of Business, Uttara University Chief Editor Dr. DNR Paul, Professor of Statistics, School of Business, Uttara University Member Dr. ASM Shahabuddin, Professor of Management, School of Business, Uttara University Member Dr. Sharmina Afrin, Associate Professor of Management, School of Business, Uttara University Member Dr. Zamanur Rahman, Associate Professor of Accounting, School of Business, Uttara University Member Mahamudul Hasan, Associate Professor of Marketing, School of Business, Uttara University Member Dr. Golam Morshed, Assistant Professor of Accounting, School of Business, Uttara University Member Mr. -

Dedicated COVID-19 Hospital Both in Government and Private Setup In
Dedicated COVID-19 Hospital both in government and private setup in Dhaka City Government Hospital Private Hospital Name, Hospital Name Isolation Name, Designation Isolation Designation ICU Remarks Hospital name ICU Remarks Beds with Contact No Beds with Contact No Bangladesh Kuwait DrShihab Uddin 25+ Regent Hospital, Moitree Hospital, 200 1711307069 50 3 1980222211 5Dia Uttara Uttara, Dhaka Superintendent Chairman/MD 250 Bed Sheikh Prof Dr Faruq Ahmed 16+ Regent Hospital, RaselGastroliver 250 1819221115 50 3 2Dia Mirpur Institute & Hospital Director DrFazlulHaqu DrAlamgir Sajida Foundation Railway Hospital, 5+ e 100 0 Hospital, 50 Kamolapur 1Dia 1711535042 Narayanganj, Kachpur 1737299248 Superintendent Mohanagar General Director 150 0 Hospital, Babubazar 1718884476 Mirpur Lalkuthi Director 200 0 Hospital 1720427959 Kurmitola General 27+ Brig General Jamil 500 hospital 32Dia 1769010201 Total beds in Govt Total beds in Pvt 1400 68 150 11 setup in Dhaka City setup in Dhaka Grand total Isolation beds (both government and private) 1550 Grand total ICU beds (both government and private) 79 Grand total Dialysis beds (both government and private) 40 Division wise dedicated COVID-19 hospital/Facility ICU S Name of Name of Beds for Name of Hospital/Facility be Remarks L Division District COVID-19 ds Doctors quarter, sheksaherakhatun MCH(50), Kashiani new hospital(5), 1 Gopalgonj Muktijiddhacomplex,moksedpur(5), 70 Tungipara UHC new building(5), Kotaliparasheklutfur Rahman adorshocolledge(5) 2 Faridpur Upazillasasthocomplex,salta (50) 50 3 Manikgonj -

A Critical Analysis of Housing Provision for Low Income Group at Uttara Model Town
A CRITICAL ANALYSIS OF HOUSING PROVISION FOR LOW INCOME GROUP AT UTTARA MODEL TOWN MAHFUJA AKTAR MASTER OF URBAN AND REGIONAL PLANNING DEPARTMENT OF URBAN AND REGIONAL PLANNING BANGLADESH UNIVERSITY OF ENGINEERING AND TECHNOLOGY DHAKA January, 2011 Thesis Acceptance Certificate The thesis titled “CRITICAL ANALYSIS OF HOUSING PROVISION FOR LOW INCOME GROUP AT UTTARA MODEL TOWN” submitted by Mahfuja Aktar, Roll No. 040515017P Session April 2005, has been accepted as satisfactory in partial fulfillment of the requirement of the degree of Master of Urban and Regional Planning (MURP) by Course and Thesis on January 2011. Board of Examiners Dr. Afsana Haque Chairman (Supervisor) Assistant Professor Department of Urban and Regional Planning BUET, Dhaka, Bangladesh Dr. Sarwar Jahan Member (Ex-officio) Head and Professor Department of Urban and Regional Planning BUET, Dhaka, Bangladesh Dr. Ishrat Islam Member Associate Professor Department of Urban and Regional Planning BUET, Dhaka, Bangladesh Dr. Akter Mahmud Member (External) Professor Jahangir Nagar University Savar, Dhaka, Bangladesh Candidate’s Declaration This thesis has been prepared for the partial fulfillment of the requirement of the degree of Master of Urban and Regional Planning (MURP) and no part of this thesis was used for any other purpose. ------------------------------------------ Mahfuja Aktar This thesis is dedicated to my Mother Chapter 1 INTRODUCTION Chapter 2 HOUSING POLICIES AND PROGRAMS FOR LOW INCOME PEOPLE: GLOBAL PERSPECTIVE Chapter 3 DEVELOPMENT PROFILE OF UTTARA MODEL -

Merchant/Company Name
Merchant/Company Name Zone Name Outlet Address VLCC Gulshan RM Centre (4th Floor), 101,Gulshan Avenue, Gulshan-2 K.L Sweden Tailors & Fabrics Gulshan Metropoliton Shopping Plaza, Plot#2, New(Old-10), Gulshan-2 Tokyo Express Gulshan House No: 16/B, Road No: 112, Dhaka 1213 Khazana Mithai Ltd. Gulshan Shop-122(Ground Floor), Taher Tower,Gulshan Circle-2,Dhaka Aamantran Kawran Bazar Bashundhara City, Level-08, Block-C, Shop-50,Panthapath Sports World Gulshan G-11, DCC Market Gulshan-2 1212 Dhaka, Dhaka Division, Bangladesh OASIS Mohammadpur Shahabuddin Plaza, Shop # 22-28, Ground Floor, Ring Road, Adabor,Mohammadpur Furnica Ltd. Mohammadpur 45 Probal Tower (1st Floor),Ring Road,Mohammadpur Multi Sports Tejgaon 247-248, Bir Uttam Mir Shawkat Sarak, Dhaka 1208 High Street Ltd.(Crimson Cup) Banani House-24, Road-11,Block-H, Bir Uttam Khademul Bashar Road,Dhaka High Street Ltd.(Crimson Cup Uttara) Uttara Quantam Mustofa Tower, 2nd Floor, 18 Gaus Ul Azam Avenue, Sector 13, Uttara Smart View Gulshan 112 Gulshan Avenue,Ground Floor,Gulshan CHATIME Banani 1st Floor, Bulu Ocean Tower,40 Kemal Ataturk Avenue,Banani Monsoon Rain Ltd. Elephant Road 54 NEW ELEPHANT RD,1ST FLR,MINITA PLAZA Absolute Thai Banani House 52, 1st Floor, Rd No 12A, Dhaka 1212 Guhaa The Cave Kitchen Dhanmondi 736, Rangs K.B. Square,Level-9,Dhanmondi The Dhaba Dhanmondi House 54, Road 10/A, Dhanmondi Maximum Dhanmondi ADC Empire Plaza, Level-1,Stamford Road,Dhanmondi,Dhaka Urban Haat Khulshi Salam Heights,Zakir Hossain Road Pinewood Cafee Banani House-48,Road 13/C, Block-E, Banani -

Analyzing Urban Population Density Gradient of Dhaka Metropolitan Area Using Geographic Information Systems (GIS) and Census Data
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by UKM Journal Article Repository GEOGRAFIA OnlineTM Malaysian Journal of Society and Space 11 issue 13 (1 - 13) 1 © 2015, ISSN 2180-2491 Analyzing urban population density gradient of Dhaka Metropolitan Area using Geographic Information Systems (GIS) and Census Data Hafiza Khatun1, Nishat Falgunee1, Md. Juel Rana Kutub2 1Geography and Environment Department, University of Dhaka, Bangladesh, 2Faujdarhat Cadet College, Chittagong, Bangladesh Correspondence: Md. Jueal Rana Kutub (email: [email protected]) Abstract Worldwide increase in urban population draws special attention to urban population density related research. Based on Thana level census data for the years 2001 and 2011, this study attempts to analyze the density gradient of urban population in Dhaka Metropolitan Area using Geographic Information Systems (GIS). Four mathematical functions have been considered to examine the change in population density with distance from CBD, after the classical work of Colin Clark in 1951. The density gradient appears to be following the negative exponential function. Result reveals that the density curve flattens over time, indicating greater increase of population density in the areas located further from the CBD than areas adjacent to it. GIS-based surface modeling using density contours shows the spatial pattern of population density has changed substantially. The study further corroborates that historical as well as economic factors are influencing the pattern and change of population density in Dhaka Metropolitan Area (DMA). Keywords: CBD, density curve, density gradient, Dhaka Metropolitan Area (DMA), Geographic Information Systems (GIS), population density Introduction More than fifty percent of global population is now urban and the rate of urbanization has been increasing over time (World Bank and BCAS, 1998; Zaman et al., 2010). -

Fire and Other Safety Incidents in the Bangladesh Garment Sector November 24, 2012-April 14, 2019
Fire and Other Safety Incidents in the Bangladesh Garment Sector November 24, 2012-April 14, 2019 AT LEAST 3,877 INJURIES / AT LEAST 1,304* DEATHS Safety Factory Incident Incidents Name Location Date Injuries Deaths Cause/Outcome Description 1 Tazreen 252, 253 & 258, 11/24/1 200 112 The fire, presumably caused by a short circuit, started on the ground floor of the nine-story factory, Fashions Ltd. Monoshontuspur, 2 trapping the workers on the floors above. Because of the large amount of fabric and yarn in the factory, Nishenantopur, the fire was able to quickly spread to other floors, complicating the firefighting operations. The fire Ashulia burned for more than seventeen hours before the firefighters were successful in extinguishing it. 2 Swan Dakkin 11/26/1 0 1 The fire originated from the warehouse of Swan Garments Ltd on the 1st floor of Afnan Plaza at Garments Khan,Uttara, 2 Mollartek around 9:30am. It was doused around 12:00 noon after hectic efforts by 13 firefighting units. Ltd Dhaka Except for the second floor, the blaze could not spread through the building. Some workers sustained minor injuries as they rushed to the main staircase to get out of the building. Bundles of threads and clothes kept in the warehouse were also gutted. 3 Al-Shahriar Palashbari, 11/27/1 0 0 Fire might have originated from an electrical short circuit at the warehouse. Fabrics was burnt. No Injury Fabric Ltd. Ashulia 2 4 Section Chittagong EPZ 11/28/1 50 0 Power generator of the factory caught fire due to a mechanical glitch.