Patient Pathway for Mtrts
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

OPERATIONAL GUIDANCE on HOSPITAL RADIOPHARMACY: a SAFE and EFFECTIVE APPROACH the Following States Are Members of the International Atomic Energy Agency
OPERATIONAL GUIDANCE ON HOSPITAL RADIOPHARMACY: A SAFE AND EFFECTIVE APPROACH The following States are Members of the International Atomic Energy Agency: AFGHANISTAN GUATEMALA PAKISTAN ALBANIA HAITI PALAU ALGERIA HOLY SEE PANAMA ANGOLA HONDURAS PARAGUAY ARGENTINA HUNGARY PERU ARMENIA ICELAND PHILIPPINES AUSTRALIA INDIA POLAND AUSTRIA INDONESIA PORTUGAL AZERBAIJAN IRAN, ISLAMIC REPUBLIC OF QATAR BANGLADESH IRAQ REPUBLIC OF MOLDOVA BELARUS IRELAND ROMANIA BELGIUM ISRAEL RUSSIAN FEDERATION BELIZE ITALY SAUDI ARABIA BENIN JAMAICA SENEGAL BOLIVIA JAPAN SERBIA BOSNIA AND HERZEGOVINA JORDAN SEYCHELLES BOTSWANA KAZAKHSTAN BRAZIL KENYA SIERRA LEONE BULGARIA KOREA, REPUBLIC OF SINGAPORE BURKINA FASO KUWAIT SLOVAKIA CAMEROON KYRGYZSTAN SLOVENIA CANADA LATVIA SOUTH AFRICA CENTRAL AFRICAN LEBANON SPAIN REPUBLIC LIBERIA SRI LANKA CHAD LIBYAN ARAB JAMAHIRIYA SUDAN CHILE LIECHTENSTEIN SWEDEN CHINA LITHUANIA SWITZERLAND COLOMBIA LUXEMBOURG SYRIAN ARAB REPUBLIC COSTA RICA MADAGASCAR TAJIKISTAN CÔTE D’IVOIRE MALAWI THAILAND CROATIA MALAYSIA THE FORMER YUGOSLAV CUBA MALI REPUBLIC OF MACEDONIA CYPRUS MALTA TUNISIA CZECH REPUBLIC MARSHALL ISLANDS TURKEY DEMOCRATIC REPUBLIC MAURITANIA UGANDA OF THE CONGO MAURITIUS UKRAINE DENMARK MEXICO UNITED ARAB EMIRATES DOMINICAN REPUBLIC MONACO UNITED KINGDOM OF ECUADOR MONGOLIA GREAT BRITAIN AND EGYPT MONTENEGRO NORTHERN IRELAND EL SALVADOR MOROCCO ERITREA MOZAMBIQUE UNITED REPUBLIC ESTONIA MYANMAR OF TANZANIA ETHIOPIA NAMIBIA UNITED STATES OF AMERICA FINLAND NEPAL URUGUAY FRANCE NETHERLANDS UZBEKISTAN GABON NEW ZEALAND VENEZUELA GEORGIA NICARAGUA VIETNAM GERMANY NIGER YEMEN GHANA NIGERIA ZAMBIA GREECE NORWAY ZIMBABWE The Agency’s Statute was approved on 23 October 1956 by the Conference on the Statute of the IAEA held at United Nations Headquarters, New York; it entered into force on 29 July 1957. The Headquarters of the Agency are situated in Vienna. -

Radiopharmaceuticals and Contrast Media – Oxford Clinical Policy
UnitedHealthcare® Oxford Clinical Policy Radiopharmaceuticals and Contrast Media Policy Number: RADIOLOGY 034.19 T0 Effective Date: January 1, 2021 Instructions for Use Table of Contents Page Related Policies Coverage Rationale ....................................................................... 1 • Cardiology Procedures Requiring Prior Definitions .................................................................................... 10 Authorization for eviCore Healthcare Arrangement Prior Authorization Requirements .............................................. 10 • Radiation Therapy Procedures Requiring Prior Applicable Codes ........................................................................ 10 Authorization for eviCore Healthcare Arrangement Description of Services ............................................................... 13 • Radiology Procedures Requiring Prior Authorization References ................................................................................... 13 for eviCore Healthcare Arrangement Policy History/Revision Information ........................................... 14 Instructions for Use ..................................................................... 14 Coverage Rationale eviCore healthcare administers claims on behalf of Oxford Health Plans for the following services that may be billed in conjunction with radiopharmaceuticals and/or contrast media: • Radiology Services: Refer to Radiology Procedures Requiring Prior Authorization for eviCore Healthcare Arrangement for additional information. -

Nuclear Pharmacy Quick Sample
12614-01_CH01-rev3.qxd 10/25/11 10:56 AM Page 1 CHAPTER 1 Radioisotopes Distribution for Not 1 12614-01_CH01-rev3.qxd 10/25/1110:56AMPage2 2 N TABLE 1-1 Radiopharmaceuticals Used in Nuclear Medicine UCLEAR Chemical Form and Typical Dosage P Distribution a b HARMACY Radionuclide Dosage Form Use (Adult ) Route Carbon C 11 Carbon monoxide Cardiac: Blood volume measurement 60–100 mCi Inhalation Carbon C 11 Flumazenil injection Brain: Benzodiazepine receptor imaging 20–30 mCi IV Q UICK Carbon C 11 Methionine injection Neoplastic disease evaluation in brain 10–20 mCi IV R Carbon C 11 forRaclopride injection Brain: Dopamine D2 receptor imaging 10–15 mCi IV EFERENCE Carbon C 11 Sodium acetate injection Cardiac: Marker of oxidative metabolism 12–40 mCi IV Carbon C 14 Urea Diagnosis of Helicobacter pylori infection 1 µCi PO Chromium Cr 51 Sodium chromate injection Labeling red blood cells (RBCs) for mea- 10–80 µCi IV suring RBC volume, survival, and splenic sequestration Cobalt Co 57 Cyanocobalamin capsules Diagnosis of pernicious anemia and 0.5 µCi PO Not defects of intestinal absorption Fluorine F 18 Fludeoxyglucose injection Glucose utilization in brain, cardiac, and 10–15 mCi IV neoplastic disease Fluorine F 18 Fluorodopa injection Dopamine neuronal decarboxylase activity 4–6 mCi IV in brain Fluorine F 18 Sodium fluoride injection Bone imaging 10 mCi IV Gallium Ga 67 Gallium citrate injection Hodgkin’s disease, lymphoma 8–10 mCi IV Acute inflammatory lesions 5 mCi IV Indium In 111 Capromab pendetide Metastatic imaging in patients with biopsy- -
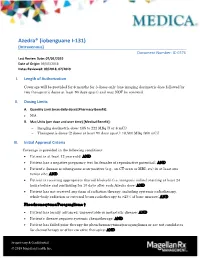
Azedra® (Iobenguane I‐131) (Intravenous) Document Number: IC‐0376 Last Review Date: 07/01/2019 Date of Origin: 09/05/2018 Dates Reviewed: 09/2018, 07/2019
Azedra® (iobenguane I‐131) (Intravenous) Document Number: IC‐0376 Last Review Date: 07/01/2019 Date of Origin: 09/05/2018 Dates Reviewed: 09/2018, 07/2019 I. Length of Authorization Coverage will be provided for 6 months for 3 doses only (one imaging dosimetric dose followed by two therapeutic doses at least 90 days apart) and may NOT be renewed. II. Dosing Limits A. Quantity Limit (max daily dose) [Pharmacy Benefit]: N/A B. Max Units (per dose and over time) [Medical Benefit]: Imaging dosimetric dose: 185 to 222 MBq (5 or 6 mCi) Therapeutic doses (2 doses at least 90 days apart): 18,500 MBq (500 mCi) III. Initial Approval Criteria Coverage is provided in the following conditions: Patient is at least 12 years old; AND Patient has a negative pregnancy test (in females of reproductive potential); AND Patient’s disease is iobenguane scan-positive (e.g., on CT-scan or MRI, etc) in at least one tumor site; AND Patient is receiving appropriate thyroid blockade (i.e. inorganic iodine) starting at least 24 hours before and continuing for 10 days after each Azedra dose; AND Patient has not received any form of radiation therapy, including systemic radiotherapy, whole-body radiation or external beam radiotherapy to >25% of bone marrow; AND Pheochromocytoma/Paraganglioma † Patient has locally advanced, unresectable or metastatic disease; AND Patient’s disease requires systemic chemotherapy; AND Patient has failed prior therapy for pheochromocytoma/paraganglioma or are not candidates for chemotherapy or other curative therapies; AND Proprietary & Confidential © 2019 Magellan Health, Inc. Patient has a life expectancy of at least 6 months; AND Patient has a Karnofsky Performance Status score ≥ 60; AND Patient does not have uncontrolled/unstable hypertension † FDA Approved Indication(s); ‡ Compendia recommended indication(s) IV. -

The Evolving Landscape of Therapeutic and Diagnostic Radiopharmaceuticals
ARTICLE THE EVOLVING LANDSCAPE OF THERAPEUTIC AND DIAGNOSTIC RADIOPHARMACEUTICALS Therapeutic and diagnostic approaches involving the use of radiation and radioactive compounds have a long- standing history in the fields of science and medicine. Radiotherapy was first used in cancer treatments in 1896.1 Since then, the field of radiation has advanced to further understand how radioactive compounds interact with biological tissues and how they can be used in both diagnostic and therapeutic applications. Radiopharmaceuticals are compounds used for medicinal purposes that contain radioactive isotopes (also known as radionuclides) and can be diagnostic or therapeutic in nature, or both.2 They represent a unique category of pharmaceuticals due to their radioactive properties. As such, there are specific guidelines and regulations that impact and direct the study and use of these compounds. Radiopharmaceutical drug development has rapidly expanded over the last decade. Radiopharmaceuticals are widely used in the field of imaging for diagnosis, staging, and follow up; in the realm of therapeutics, their use has increased, most notably, in the area of oncology. In a recent webinar, experts from Medpace’s radiation oncology, imaging, regulatory, and operational teams discussed the growing space of radiopharmaceutical development with respect to their biological use and application, regulatory frameworks that govern their evaluation in support of approvals, operational manufacturing considerations, and associated imaging approaches. BIOLOGICAL MECHANISMS OF ACTION OF RADIONUCLIDES According to Dr. Jess Guarnaschelli, Medical Director, Radiation Oncology, the radioactivity of radionuclides can be employed for both diagnostic and therapeutic medical uses. While external beam ionizing radiation involves radiation emitted in the form of electromagnetic waves or particles, radiopharmaceuticals use radionuclides to deliver localized radiation to specific targets. -

Mechanisms of Radiopharmaceutical Localization
.::VOLUME 16, LESSON 4::. Mechanisms of Radiopharmaceutical Localization Continuing Education for Nuclear Pharmacists And Nuclear Medicine Professionals By James A. Ponto, MS, RPh, BCNP Chief Nuclear Pharmacists, University of Iowa Hospitals and Clinics and Professor (Clinical), University of Iowa Hospitals and Clinics The University of New Mexico Health Sciences Center, College of Pharmacy is accredited by the Accreditation Council for Pharmacy Education as a provider of continuing pharmacy education. Program No. 0039-000-12-164- H04-P 2.5 Contact Hours or .25 CEUs. Initial release date: 7/19/2012 -- Intentionally left blank -- Mechanisms of Radiopharmaceutical Localization By James A. Ponto, MS, RPh, BCNP Editor, CENP Jeffrey Norenberg, MS, PharmD, BCNP, FASHP, FAPhA UNM College of Pharmacy Editorial Board Stephen Dragotakes, RPh, BCNP, FAPhA Michael Mosley, RPh, BCNP Neil Petry, RPh, MS, BCNP, FAPhA James Ponto, MS, RPh, BCNP, FAPhA Tim Quinton, PharmD, BCNP, FAPhA S. Duann Vanderslice, RPh, BCNP, FAPhA John Yuen, PharmD, BCNP Advisory Board Dave Engstrom, PharmD, BCNP Vivian Loveless, PharmD, BCNP, FAPhA Brigette Nelson, MS, PharmD, BCNP Brantley Strickland, BCNP Susan Lardner, BCNP Christine Brown, BCNP Director, CENP Administrator, CE & Web Publisher Kristina Wittstrom, MS, RPh, BCNP, FAPhA Christina Muñoz, M.A. UNM College of Pharmacy UNM College of Pharmacy While the advice and information in this publication are believed to be true and accurate at the time of press, the author(s), editors, or the publisher cannot accept any legal responsibility for any errors or omissions that may be made. The publisher makes no warranty, expressed or implied, with respect to the material contained herein. -

Marrakesh Agreement Establishing the World Trade Organization
No. 31874 Multilateral Marrakesh Agreement establishing the World Trade Organ ization (with final act, annexes and protocol). Concluded at Marrakesh on 15 April 1994 Authentic texts: English, French and Spanish. Registered by the Director-General of the World Trade Organization, acting on behalf of the Parties, on 1 June 1995. Multilat ral Accord de Marrakech instituant l©Organisation mondiale du commerce (avec acte final, annexes et protocole). Conclu Marrakech le 15 avril 1994 Textes authentiques : anglais, français et espagnol. Enregistré par le Directeur général de l'Organisation mondiale du com merce, agissant au nom des Parties, le 1er juin 1995. Vol. 1867, 1-31874 4_________United Nations — Treaty Series • Nations Unies — Recueil des Traités 1995 Table of contents Table des matières Indice [Volume 1867] FINAL ACT EMBODYING THE RESULTS OF THE URUGUAY ROUND OF MULTILATERAL TRADE NEGOTIATIONS ACTE FINAL REPRENANT LES RESULTATS DES NEGOCIATIONS COMMERCIALES MULTILATERALES DU CYCLE D©URUGUAY ACTA FINAL EN QUE SE INCORPOR N LOS RESULTADOS DE LA RONDA URUGUAY DE NEGOCIACIONES COMERCIALES MULTILATERALES SIGNATURES - SIGNATURES - FIRMAS MINISTERIAL DECISIONS, DECLARATIONS AND UNDERSTANDING DECISIONS, DECLARATIONS ET MEMORANDUM D©ACCORD MINISTERIELS DECISIONES, DECLARACIONES Y ENTEND MIENTO MINISTERIALES MARRAKESH AGREEMENT ESTABLISHING THE WORLD TRADE ORGANIZATION ACCORD DE MARRAKECH INSTITUANT L©ORGANISATION MONDIALE DU COMMERCE ACUERDO DE MARRAKECH POR EL QUE SE ESTABLECE LA ORGANIZACI N MUND1AL DEL COMERCIO ANNEX 1 ANNEXE 1 ANEXO 1 ANNEX -

Solution for Injection 1. NAME of the MEDICINAL PRODUCT MIBG
SUMMARY OF PRODUCT CHARACTERISTICS for MIBG (I-123), solution for injection 1. NAME OF THE MEDICINAL PRODUCT MIBG (I-123) 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Composition per ml, at activity reference date and time 123I as Iobenguane 74 MBq 3-iodobenzylguanidine sulphate 0.5 mg The radiochemical purity of the product at expiry date and time: 123I-Iobenguane: 95 % Meta-iodo (123I) benzylamine: 0.5 % Free iodide (123I): 5 % The radionuclidic purity of the product at expiry date and time: 123I : > 99.9 % 121Te : 500 Bq/MBq 123I is obtained by proton irradiation of enriched Xenon. Summary of the physical characteristics of the radioactive isotope in the active substance: 123I. Physical half-life 13.2 hours Most important radiation emitted Energy level Abundance - rays 159 keV 83.6 % Excipient: Sodium citrate For a full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Solution for injection MIBG+(I123)+Mallinckrodt Page 1 of 8 4. CLINICAL PARTICULARS 4.1 Therapeutic indications This medicinal product is for diagnostic use only. Diagnostic scintigraphic localisation of tumours originating in tissue that embryologically stems from the neural crest. These are pheochromocytomas, paragangliomas, chemodec- tomas and ganglioneuromas. Detection, staging and follow-up on therapy of neuroblastomas. Evaluation of the uptake of iobenguane. The sensitivity to diagnostic visualisation is dif- ferent for the listed pathologic entities. Pheochromocytomas and neuroblastomas are sensi- tive in approx. 90 % of patients, carcinoids in 70 % and MCT in only 35 %. Functional studies of the adrenal medulla (hyperplasia) and the myocardium (sympathetic innervation). 4.2 Posology and method of administration 123I-Iobenguane is administered according to the following dosage scheme: Children under 6 months: 4 MBq per kg body weight (max. -
Slides Report on Recent Factors Related to the T&E Report, and Are Not That of the Convened Subcommittee
Overview: 2019-2020 ACMUI Activities Darlene Metter, M.D. ACMUI Chair/Diagnostic Radiologist November 18, 2020 Today’s Agenda • A. Robert Schleipman, Ph.D. (ACMUI Vice-Chair) – ACMUI’s Comments on the Staff’s Evaluation of Training and Experience for Radiopharmaceuticals Requiring a Written Directive • Ms. Melissa Martin (ACMUI Nuclear Medicine Physicist) – ACMUI’s Comments on Extravasations 2 Today’s Agenda cont’d • Mr. Michael Sheetz (ACMUI Radiation Safety Officer) – ACMUI’s Comments on Patient Intervention and Other Actions Exclusive of Medical Events • Hossein Jadvar, M.D., Ph.D. (ACMUI Nuclear Medicine Physician) – Trending Radiopharmaceuticals 3 Overview of the ACMUI • ACMUI Role • Membership • 2019-2020 Topics • Current Subcommittees • Future 4 Role of the ACMUI • Advise the U.S. Nuclear Regulatory Commission (NRC) staff on policy & technical issues that arise in the regulation of the medical use of radioactive material in diagnosis & therapy. • Comment on changes to NRC regulations & guidance. • Evaluate certain non-routine uses of radioactive material. 5 Role of the ACMUI (cont’d) • Provide technical assistance in licensing, inspection & enforcement cases. • Bring key issues to the attention of the Commission for appropriate action. 6 ACMUI Membership (12 members) • Healthcare Administrator (Dr. Arthur Schleipman) • Nuclear Medicine Physician (Dr. Hossein Jadvar) • 2 Radiation Oncologists (Drs. Ronald Ennis & Harvey Wolkov) • Nuclear Cardiologist (Dr. Vasken Dilsizian) • Diagnostic Radiologist (Dr. Darlene Metter) • Nuclear Pharmacist (Mr. Richard Green) 7 7 ACMUI Membership (12 members) • 2 Medical Physicists Nuclear Medicine (Ms. Melissa Martin) Radiation Therapy (Mr. Zoubir Ouhib) • Radiation Safety Officer (Mr. Michael Sheetz) • Patients’ Rights Advocate (Mr. Gary Bloom*) • FDA Representative (Dr. Michael O’Hara) • Agreement State Representative (Ms. -

Radionuclides and Radiopharmaceuticals for 2005
NEWSLINE Radionuclides and Radiopharmaceuticals for 2005 he breakneck rate of change to which we have diagnosis of appendicitis in patients age 5 and over with become accustomed in the scientific world has not equivocal symptoms and signs. T been reflected in the number of changes in avail- Although PET agents such as 11C-carbon monoxide, able radionuclides and radiopharmaceuticals between my 11C-flumenazil, 11C-mespiperone, 11C-methionine, 11C- last compilation in 2003 (J Nucl Med. 2003;44[6]:27N– raclopride, 11C-acetate, 18F-fluorodopa, 13N-ammonia, and 31N) and the current lists. Economic and regulatory issues 15O-water are now being compounded under the state- have not kept pace with radiopharmaceutical science. regulated practice of medicine and pharmacy, these are Gone is radiolabeled hippuran (labeled with 123Ior not widely available outside of certain research institu- 131I), a stalwart of renal diagnosis since 1961, because of tions and so do not appear on the list. the excellent physical and biologic properties of 99mTc- I have added 2 radiopharmaceuticals classified as “de- mertiatide (MAG3). 99mTc-lidofenin has disappeared as a vices” for brachytherapy by the FDA: 90Y-microspheres hepatobiliary agent, leaving 99mTc-labeled disofenin and (for unresectable hepatocellular carcinoma) and 125I-3- mebrofenin on the market. iodo-4-hydroxybenzenesulfonate (for recurrent malignant 131I-tositumomab finally passed U.S. Food and Drug glioma). Administration (FDA) review as another labeled antibody A number of new radionuclides appear on this list, against lymphocyte antigen CD20 (as is 90Y-ibritumomab such as 7Be, 32Si, and 44Ti, produced by the U.S. Depart- tiuxetan) for the therapy of lymphoma. -

Federal Register / Vol. 60, No. 80 / Wednesday, April 26, 1995 / Notices DIX to the HTSUS—Continued
20558 Federal Register / Vol. 60, No. 80 / Wednesday, April 26, 1995 / Notices DEPARMENT OF THE TREASURY Services, U.S. Customs Service, 1301 TABLE 1.ÐPHARMACEUTICAL APPEN- Constitution Avenue NW, Washington, DIX TO THE HTSUSÐContinued Customs Service D.C. 20229 at (202) 927±1060. CAS No. Pharmaceutical [T.D. 95±33] Dated: April 14, 1995. 52±78±8 ..................... NORETHANDROLONE. A. W. Tennant, 52±86±8 ..................... HALOPERIDOL. Pharmaceutical Tables 1 and 3 of the Director, Office of Laboratories and Scientific 52±88±0 ..................... ATROPINE METHONITRATE. HTSUS 52±90±4 ..................... CYSTEINE. Services. 53±03±2 ..................... PREDNISONE. 53±06±5 ..................... CORTISONE. AGENCY: Customs Service, Department TABLE 1.ÐPHARMACEUTICAL 53±10±1 ..................... HYDROXYDIONE SODIUM SUCCI- of the Treasury. NATE. APPENDIX TO THE HTSUS 53±16±7 ..................... ESTRONE. ACTION: Listing of the products found in 53±18±9 ..................... BIETASERPINE. Table 1 and Table 3 of the CAS No. Pharmaceutical 53±19±0 ..................... MITOTANE. 53±31±6 ..................... MEDIBAZINE. Pharmaceutical Appendix to the N/A ............................. ACTAGARDIN. 53±33±8 ..................... PARAMETHASONE. Harmonized Tariff Schedule of the N/A ............................. ARDACIN. 53±34±9 ..................... FLUPREDNISOLONE. N/A ............................. BICIROMAB. 53±39±4 ..................... OXANDROLONE. United States of America in Chemical N/A ............................. CELUCLORAL. 53±43±0 -

FDA-Approved Radiopharmaceuticals
Medication Management FDA-approved radiopharmaceuticals This is a current list of all FDA-approved radiopharmaceuticals. USP <825> requires the use of conventionally manufactured drug products (e.g., NDA, ANDA) for Immediate Use. Nuclear medicine practitioners that receive radiopharmaceuticals that originate from sources other than the manufacturers listed in these tables may be using unapproved copies. Radiopharmaceutical Manufacturer Trade names Approved indications in adults (Pediatric use as noted) 1 Carbon-11 choline Various - Indicated for PET imaging of patients with suspected prostate cancer recurrence based upon elevated blood prostate specific antigen (PSA) levels following initial therapy and non-informative bone scintigraphy, computerized tomography (CT) or magnetic resonance imaging (MRI) to help identify potential sites of prostate cancer recurrence for subsequent histologic confirmation 2 Carbon-14 urea Halyard Health PYtest Detection of gastric urease as an aid in the diagnosis of H.pylori infection in the stomach 3 Copper-64 dotatate Curium Detectnet™ Indicated for use with positron emission tomography (PET) for localization of somatostatin receptor positive neuroendocrine tumors (NETs) in adult patients 4 Fluorine-18 florbetaben Life Molecular Neuraceq™ Indicated for Positron Emission Tomography (PET) imaging of the brain to Imaging estimate β amyloid neuritic plaque density in adult patients with cognitive impairment who are being evaluated for Alzheimer’s disease (AD) or other causes of cognitive decline 5 Fluorine-18