Royal Berkshire Hospital Scheduled Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

THE OLD REDINGENSIAN Spring 2007
THE OLD REDINGENSIAN Spring 2007 Henry VII King of England Benefactor of Reading School 1486 The Presidentʼs Letter I am delighted to have been accepted as President of the OR Association for 2007 and to contribute to the institution that is Reading School. In so doing, I am conscious that, whilst I have been a Council member for the last two years, I have been very much “in absentia” due to work commitments. I would like to take this opportunity to introduce myself to the membership and outline my thoughts upon our direction for this coming year. For background, I was a pupil at Reading School from 1978-85 and infl uenced by several Masters who are now pillars of OR life such as John Oakes, Bob Lewis and Mike Evans. I ended my time at the School as Captain of West House and Cadet RSM of the CCF. Commissioned into the Army in 1987, I have served all over the World and currently command 13 Air Assault Support Regiment, The Royal Logistic Corps, based in Colchester. We are part of the Air Assault Brigade and deployed on operations in Afghanistan last summer. I am married to Jackie and have two children, Adam who currently attends Colchester Royal Grammar School, and Gemma, who will start at the Colchester Girls High School (also a grammar) this September. In my time on the Council I have been impressed by is very positive about harnessing our support along the selfl essness and commitment of a determined with Governors, parents and the Foundation to realise band of Association members who organise and further benefi ts for the School. -

Getting to the Royal Berkshire Hospital
Tel: 0118 322 5111 Web: www.royalberkshire.nhs.uk Web: 5111 322 0118 Tel: London Road, Reading RG1 5AN RG1 Reading Road, London Royal Berkshire NHS Foundation Trust Foundation NHS Berkshire Royal July 2006 July service information Patient www.busbook.co.uk Thames Travel: 01491 837988 837988 01491 Travel: Thames www.reading-buses.co.uk Reading Transport: 0118 959 4000 4000 959 0118 Transport: Reading www.traveline.org.uk Traveline Public Transport Information: 0870 608 2608 608 0870 Information: Transport Public Traveline Further information is available from available is information Further Craven Road. Craven N2a NightTrack from Reading to Woodley via via Woodley to Reading from NightTrack Craven Road Craven N3 NightTrack from Lower Earley to Reading via via Reading to Earley Lower from NightTrack Redlands Road (Thames Travel) (Thames Road Redlands Royal Berkshire Hospital Berkshire Royal 144 Reading to Wokingham via Craven Road and and Road Craven via Wokingham to Reading Redlands Road Redlands Getting to the the to Getting 42 Reading to Woodley via Craven Road and and Road Craven via Woodley to Reading 28 Redlands Road to Reading, Grovelands and Tilehurst and Grovelands Reading, to Road Redlands Reading station Reading 18 Lower Earley to Calcot via RBH South block and and block South RBH via Calcot to Earley Lower Road and Redlands Road Redlands and Road 9 Caversham Heights to Whitley Wood via Craven Craven via Wood Whitley to Heights Caversham Reading town centre town Reading A number of buses travel between the hospital and and hospital the between travel buses of number A Travelling by bus by Travelling Car parking Park & Ride During peak periods on weekdays, there is often difficulty During peak periods on weekdays, there are many finding a parking space. -

The Stoma Service
Suggestions and concerns How to contact us: We strive for excellence when caring for If you have any concerns regarding stoma patients and their families. If you your stoma, pouch, stoma output, have any concerns regarding your care, peristomal skin or your post-operative please talk to your stoma nurse in the first recovery, contact the team on: instance. We will try to resolve any problems as quickly and efficiently as or email 0118 322 7640 possible. [email protected] Alternatively, if you have any comments and Monday to Friday (excluding bank you would prefer to speak to someone holidays) between 8am and 4pm. outside of the Stoma Care Team, contact the Patient Advice and Liaison Service (PALS) on 0118 322 8338 or email If your call goes to answerphone, [email protected] please leave your name, contact We are constantly reviewing and updating details and a brief message, and your the service we offer, and are always looking query will be dealt with by the next to improve the support and advice we working day. provide. If you have any suggestions please feel free speak to your stoma care nurse at Out of hours, contact your GP or their any time. out of hours service. For emergencies, dial NHS 111, or To find out more about our Trust visit visit your nearest Walk-in Centre or www.royalberkshire.nhs.uk The Stoma Emergency Department (A&E). Please ask if you need this information Service in another language or format. Information for patients Stoma Care Nurses, April 2021 who have had a stoma Next review due: April 2023 formed If you are unable to attend your clinic then arrange for you to collect them. -

70 NHS Years: a Celebration of 70 Influential Nurses and Midwives
0 A celebration of 7 influential nurses NHS YEARS20 and midwives from 1948 to 18 In partnership with Seventy of the most influential nurses and midwives: 1948-2018 nursingstandard.com July 2018 / 3 0 7 years of nursing in the NHS Inspirational nurses and midwives who helped to shape the NHS Jane Cummings reflects on the lives of 70 remarkable As chief nursing officer for England, I am delighted figures whose contributions to nursing and to have contributed to this publication on behalf of midwifery are summarised in the following profiles, the CNOs in Northern Ireland, Scotland and Wales, and on the inspiration they provide as the profession identifying some of the most influential nurses and Jane Cummings meets today’s challenges midwives who have made a significant impact across chief nursing officer the UK and beyond. for England I would like to give special thanks to the RCNi As a nurse, when I visit front-line services and and Nursing Standard, who we have worked in meet with staff and colleagues across the country partnership with to produce this important reflection I regularly reflect on a powerful quote from the of our history over the past 70 years, and to its American author and management expert Ken sponsor Impelsys. Blanchard: ‘The key to successful leadership today is influence, not authority.’ Tireless work to shape a profession I am a firm believer that everyone in our Here you will find profiles of 70 extraordinary profession, whatever their role, wherever they work, nursing and midwifery leaders. Many of them have has the ability to influence and be influenced by the helped shape our NHS. -

St-James-Kennet-Island-Host-Brochure
ENJOY A LIFE LESS ORDINARY AT KENNET ISLAND THE WATERSIDE APARTMENTS Located a short distance from Reading town centre or a 26 minute train journey to Central London, Kennet Island by St James offers contemporary designed apartments and houses within beautifully landscaped grounds. Residents can enjoy peaceful walks near the Foudry Brook ecological corridor or down the tree-lined boulevards. At the centre of the development is the Piazza, which provides the Kennet Island community with a café, children’s day care nursery, local shop and gym. Alternatively, residents can take advantage of the facilities of the Hilton Hotel, which includes a swimming pool, steam room and sauna, all on the doorstep. Kennet Island combines luxury living within a thriving community close to Reading. CONTENTS 3 Introduction 18 Royal Berkshire Enjoy a life less ordinary So much to see and enjoy 4 Kennet Island 20 By Road or Rail Perfectly located London is within easy reach 6 Waterside Apartments 22 Site Plan Carefully considered Everything on your doorstep 8 The Piazza 24 Architecture At the heart of Kennet Island Considered design, beautiful views 10 Keeping Fit 26 Specification Work out and de-stress A high specification as standard 12 Open Space 30 Vision2020 The environmental side of Our commitment to sustainable living Kennet Island 32 St James 14 Shopping Designed for life With much more to offer 34 St James 16 Going Out Recent award success Buzzing bars to fine dining 36 Maps How to find us 4 KENNET ISLAND Kennet Island PERFECTLY LOCATED The Blade River Thames Oxford The Oracle Reading Train Station Reading Train Royal Berkshire Hospital Royal Berkshire University of Reading Brunel Retail Park Hilton Hotel Green Park Madejski Stadium Reading Gate Retail Park Junction 11 of M4 When living at Kennet Island, convenience comes as standard. -

Royal Berkshire NHS Foundation Trust Annual Report and Financial
Royal Berkshire NHS Foundation Trust Annual Report and Financial Statements for the year ended 31 March 2016 Presented to Parliament pursuant to Schedule 7, paragraph 25(4) of the National Health Service Act 2006 Royal Berkshire NHS Foundation Trust Annual Report and Financial Statements for the year ended 31 March 2016 ©2016 Royal Berkshire NHS Foundation Trust Annual Report 2015/16 Contents Page No Chairman’s and Chief Executive’s Introduction 5 Performance Report Overview of performance 8 Performance analysis 8 Accountability Report Directors’ Report 13 Statement as to disclosure to auditors Income disclosures Enhanced quality governance reporting Governance arrangements Remuneration Report 35 Annual statement on remuneration Senior managers’ remuneration policy Annual report on remuneration Staff Report 46 Introductory paragraph Staff survey Expenditure of consultancy/off payroll NHS Code of Governance 52 Regulatory Ratings 56 Statements of Accounting Officer’s Responsibilities 57 Annual Governance Statement 59 Quality Account 67 Annual Accounts 140 Chairman’s Report I am delighted to be part of the Royal Berkshire NHS Foundation Trust. I began with the organisation in August 2015 and wish to thank Janet Rutherford who acted as Chair for five months prior to my arrival. I would also like to acknowledge the Non-Executive Directors, Executives and Governors all of whom have through their various roles in driving the Trust forward and, for supporting me as I gain an understanding of the complexity surrounding the NHS. It has been a year of continual change and challenge. Like many trusts we continue to see unprecedented levels of demand on our Emergency Department as well as significant pressure on other services in all our locations. -
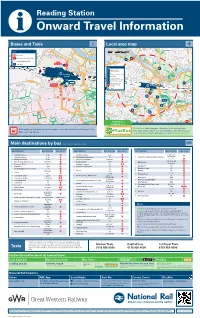
Reading Station I Onward Travel Information Buses and Taxis Local Area Map
Reading Station i Onward Travel Information Buses and Taxis Local area map km 0 0.5 Caversham Key 0 Miles 0.25 A Bus Stop Rail replacement Bus Stop H RL Station Entrance/Exit North NA Taxi Rank Interchange Key 1 NE CM 0 m C Reading Crown Court in CM u Christchurch Meadows t e H Hotel s w Reading HX The Hexagon Theatre/Arts Centre a l KM Kings Meadow k Station i n L Reading Central Library g d i M Reading Museum & Town Hall s WS t RL Rivermead Leisure Complex a RailAir n c Coach Stop SC Oracle Shopping & Leisure e KM South West H Royal Berkshire Hospital SA EK EL Reading Station Interchange Cycle routes EM SB EO Footpaths EP SC H SD H FN M FE FC H C L H HX CW SC Reading is a H PlusBus area Contains Ordnance Survey data © Crown copyright and database right 2018 & also map data © OpenStreetMap contributors, CC BY-SA Rail replacement buses/coaches depart from the North Interchange (Stop PlusBus is a discount price ‘bus pass’ that you buy with your train ticket. It gives you unlimited bus travel around your ND) see map above. chosen town, on participating buses. Visit www.plusbus.info Main destinations by bus (Data correct at September 2019) DESTINATION BUS ROUTES BUS STOP DESTINATION BUS ROUTES BUS STOP DESTINATION BUS ROUTES BUS STOP SA EP 3, 3b, 9, 10, Arborfield Cross 3, 3b Mortimer Village 2, 2a SA 19a/19b/19c Arborfield Green 3, 3b SA { Northumberland Avenue 5+ SC { University of Reading (Main Campus) 21+, 21a EK { Basingstoke Road 6+, 6a SC { Palmer Park Stadium 4/X4, 17+ EO X38, X39, X40 EL NA { Bath Road (towards Calcot) jet black1 -

Acute Frailty Pathway Royal Berkshire Hospital
Acute Frailty Pathway Royal Berkshire Hospital Dr Paul Wearing Consultant Interface Geriatrician Royal Berkshire NHS Foundation Trust “Working together to provide outstanding care for our community” Approx 500,000 patients in Berkshire and South Oxfordshire. 5 different Unitary Authorities & at least 6 CCGS Average of 1200 patients over the age of 75 attend ED every month. 130 Elderly Care beds across 6 wards. Approx 30 new elderly care admissions every twenty-four hour period. 2 Acute Frailty at the Royal Berks Emergency Department New Frailty Service & ED OT Team ECPOD Interface Geriatrics RACOP (& RACU) FFR RRAT Elderly Care wards Hip fracture unit & HFESD 3 RBH Acute area Emergency Department (27++) Ambulatory Emergency Care Unit ED Obs Ward (8+) Short Stay Unit (22) Acute Medical Unit (39) HMU (4) Older people in E.D. at RBH >300 patients per day 60 patients in ED at one time every day Only 27 bed spaces Priority to critically unwell, trauma, sepsis, stroke, chest pain Older patients attending ED increased by 25% in 4 years • Conversion rate >80% E.D. Obs ward – supposedly low risk patients only • Difficult to achieve • Admission rate 20% 5 RBH E.D. Clinical champion leading service improvement – Increased cognitive assessments – Enhanced medication in Parkinson’s disease – (identification & administration) New Frailty Friendly Front Door – Frailty screening/identification – Frailty Practitioners 6 The Frailty Friendly Front Door has gone live! Frailty Practitioners are now in the Emergency Department Bleep 579 8am – 8pm, 7 days a week The team will be carrying out parallel assessments alongside the Emergency Department doctors, to expedite prompt discharge home and/or referral to alternative pathways, for patients living with frailty. -

Formulary 12 Edition
Drug and Therapeutics Committee Formulary 12 th Edition Version14.1 May 2015 Compiled on behalf of the Drug and Therapeutics Committee by Eleanore Atkinson Medicines Information Pharmacist Formulary 12 th Edition [v14.1] Contents Introduction ..................................................................................................................................... 11 Purpose ............................................................................................................................................... 11 How to use this Formulary .................................................................................................................. 11 Prescribing Formulary drugs............................................................................................................... 11 Prescribing a non-Formulary drug ...................................................................................................... 11 Procedure for additions to and amendment of the Formulary ............................................................. 11 Prescribing information ....................................................................................................................... 12 Filling in prescription charts ............................................................................................................... 12 Intravenous antibiotics ........................................................................................................................ 12 Controlled drugs ................................................................................................................................ -
Work with Us Our Story So Far…
Work with us Our story so far… Candidate Information Pack Where we were Royal Berkshire Hospital (RBH) opened on 27th May 1839. The opening of the RBH was mainly to cope with numerous casualties during the construction of the Great Western railway, which at the time was forging its way towards Reading. The original hospital had 50 beds, and in the first five years 76 operations were performed - this was just prior to the discovery of anaesthesia (1846), and sterile surgery (1865). New wards were added to the original building in 1846 and 1850, and two new wings were built in 1861, followed by a third in 1912. The building, which is now the Berkshire Cancer Centre, included the King Edward VII Memorial Ward for children. Some nationally significant tiles in King Edward VII ward are still present today. During World War I, RBH remained a voluntary hospital, but also became a war hospital with more beds. In 1915, because of a meningitis epidemic, marquees were put on the back lawn to increase the bed numbers. Battle Hospital was designated as ‘War Hospital No. 1’. In 1967, the Maternity Unit was added to the site and services moved from Battle Hospital. Traditional long wards were replaced with bays, a model of care repeated with the addition of South Block in the 1970's. Early in the 21 st century, the two hospitals were consolidated; concluding with Battle Block in 2005. The old Battle Hospital closed in 2005, although the front gate house is listed and visible on the Oxford Road. -
Reading Station U C ELD E
READING PRISON exciting development opportunity READING PRISON Oracle Reading The River Broad Abbey Forbury A329 Forbury Reading Centre Borough Oracle Kennet Street Ruins Gardens Forbury Retail Station Parking Council Centre Mall Road Park THE OPPORTUNITY • An exceptional Freehold development opportunity extending to approximately 3.49 acres (1.41 hectares) in central Reading, in close proximity to a mainline train station. • Central to the site is the unique Grade II listed historic prison building arranged over part basement, ground and three upper floors. In addition there is an administrative building, amenities building, gym / workshop and a number of more modern buildings. • Pre-application response from Reading Borough Council emphasises the importance of re-using the listed building element and integrating the site redevelopment with the Abbey Quarter immediately to the west of the site. • Pre-application response from Historic England confirms the principle of new development around the listed prison is accepted, given the precedent set by modern prison buildings. • The site is offered with full vacant possession. • Offers are invited for our client’s Freehold interest. READING PRISON READING A PLACE TO LIVE, WORK & STUDY Reading, widely known as the ‘capital’ of the Thames Valley, is one of the most thriving urban centres in the South East offering waterside town centre living, a growing economy and easy access to both London and the surrounding countryside. The town is home to around 160,000 people, while Reading has a thriving economy and has become a the wider urban area includes more than 320,000 popular location for local, national and international people. -

South Reading Ccg Operational Plan 2014/16
Commissioning Plan South Reading Clinical Commissioning Group 2014-2016 Contents Page What is South Reading CCG? 4 Introduction from the Chair 5 Our Key Achievements 2013-14 6 Developing the Two Year Operational Plan 2014-16 8 Patients’ Rights – The NHS Constitution 10 The Health Needs of the Population 11 Our Five Clinical Areas of Focus 17 Listening to our Patients and the Public 20 Strategic Long Term Vision 2019 22 Our Local Areas of Focus 2014-2016 24 South Reading CCG – Plan on a Page 2014-2016 26 Delivering High Quality, Sustainable Health Care 27 1. Engagement with our Patients, the Public and Other Stakeholders 28 2. Wider Primary Care, Provided at Scale 31 3. Modern Model of Integration (Better Care Fund) 33 4. Access to Highest Quality Urgent and Emergency Care 33 5. A Step Change in Productivity of Elective Care (Planned Hospital Care) 35 2 6. Specialised Services Concentrated in Centres of Excellence 35 Other Enablers 36 1. Expert Clinical Advice 36 2. Workforce Development 36 3. Information Management &Technology 39 Quality & Patient Safety 40 Equality & Diversity 46 Financial Plans 47 Appendix 1 – Our GP Practices 50 Appendix 2 – Berkshire West Outcomes/Improvement Interventions 51 3 What is South Reading Clinical Commissioning Group? South Reading Clinical Commissioning Group (CCG), with a growing population of approximately 128,000, is made up of 20 GP practices (see appendix 1 for full list of our member practices) with an excellent track record of working together since 2006. The local population is younger than the national average, made up of a higher proportion of young children and also adults under 44 years whilst the proportion of over 60 years old is much lower.