Renal & Electrolyte Disturbances
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

CARE PLAN Electrolyte and Fluid Imbalance
CARE PLAN Electrolyte and Fluid Imbalance . Related to: Check all that apply Endocrine dysfunction Treatment/Drug side effects Urinary difficulties Nutritional deficiency Tissue trauma Renal dysfunction Post-op complications Trauma Other _____________ Status: Achieved/ Progressing/Not Date/Select Outcome Select Interventions Met (comment for negative variances) Serum electrolytes, Perform initial/routine BUN, blood gases will assessments, assess be within desired limits for neurological manifestations indicating electrolyte imbalance. Report findings to clinician (MD, PA, NP) promptly. Implement therapeutic actions (i.e., appropriate diet, administer replacement electrolytes—sodium bicarb, mag sulfate, etc., as ordered) Assess/monitor serum levels of electrolytes; report finding to MD promptly Monitor for associated complications Absence of cardiac Assess/monitor cardiac dysrhythmias rhythm Published by Cinahl Information Systems, a division of EBSCO Information Services. Copyright©2016, Cinahl Information Systems. All rights reserved. No part of this may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the publisher. Cinahl Information Systems accepts no liability for advice or information given herein or errors/omissions in the text. It is merely intended as a general informational overview of the subject for the healthcare professional. Cinahl Information Systems, 1509 Wilson Terrace, -

Hormones and Fluid Balance During Pregnancy, Labor and Post Partum
!" #$%#&$'($ )&)#&%%&%)&( * * **+ &#(## !"# $ % # #&$ $ ' #( )*+$ , -, $* .%/**0 # % % */ * 123*"1 * *4-52366""162"26* +$ # $ $, , , % % *4 %$ % # % % $ # $ $ # # ,$ ## $ $# %$ ## % # * % , 784-/!% , $ 9* #6 , , % % ##6 % * +$ , % ,$ $ % , $ % % % * & , % * # , , $ % %% ## % , ## $ 6% * : ,$, % ' , % # ) ## $ , ,$ % #, ,$# % # *+$% ,$ , $ , $ $ $ *& # , $## $ # , % # */ , # , ## ,$ % # * - % ,$%$ % # % $ $$%$ ' ;8)$*4 %$,$$ % # $$%$% *4 # % % $ # # $ $ $ % % * & $ %# % % $ *& $ $ # % * % % % 6 $ % Integrativ Fysiologi, Box 571, %&'()*+ Sweden </ $.% 4--5="6== 4-52366""162"26 ! !!! 623'$ !;; **; > ? ! !!! 623) In memory of my beloved father Ove I lift up my eyes to the hills -- where does my help come from? My help comes from the Lord, the Maker of heaven and earth. He will not let your foot slip -- He who watches over you will not slumber; indeed, He who watches over Israel will neither slumber nor sleep. The Lord watches over you -- the Lord is your shade at your right hand; the sun will not harm you by day, nor the moon by night. The Lord will keep you from all harm He will watch over your life; the Lord will -

Refractory Hypoglycemia in T-Cell Lymphoma
Open Access Austin Oncology Case Reports Case Report Refractory Hypoglycemia in T-Cell Lymphoma Buyukaydina B1*, Tunca M1, Alayb M2, Kazanciogluc R3 and Reha E3 Abstract 1Bezmialem Vakif University, Department of Internal Hypoglycemia is commonly seen in diabetes mellitus patients; whereas it Medicine, Turkey is rarely seen in a healthy person. In this case, we reported a male patient 2Yuzuncu Yil University, Department of Endocrinology, with a treatment-resistant hypoglycemia. A 53 years old male patient admitted Turkey to our clinic with debility, nausea and vomiting. Physical examination revealed 3Bezmialem Vakif University, Department of Nephology, lymphadenopathies in the left axilla and inguinal regions; and presence of right Turkey upper quadrant tenderness. Biochemical results revealed severe hypoglycemia, *Corresponding author: Banu Buyukaydin, azotemia and elevation of liver enzymes. Histological result of the excisional Bezmialem Vakif University, Department of Internal lymph node biopsy was compatible with peripheral T cell lymphoma. In ward, Medicine, Turkey the patient has repeated recurrent hypoglycemia, which did not resolve with all treatment given. His general condition deteriorated and he died due to sepsis. Received: June 01, 2016; Accepted: July 10, 2016; This case highlighted the need to rule out hematologic malignancies; precisely Published: July 13, 2016 T-cell lymphoma in a patient who presented with resistant hypoglycemia in the presence of lymphadenopathy. Keywords: Hypoglycemia, Lymphoma, IGF-II Introduction approximately fifty percent of proliferation index. CD3 was positive. This finding was compatible to histological diagnosis of peripheral Hypoglycemia is defined as the occurrence of a variety of T-cell lymphoma with partial involvement of lymph ganglia. symptoms in association with plasma glucose concentration of 50mg/dl or less. -

Renal Physiology
Renal Physiology Integrated Control of Na Transport along the Nephron Lawrence G. Palmer* and Ju¨rgen Schnermann† Abstract The kidney filters vast quantities of Na at the glomerulus but excretes a very small fraction of this Na in the final urine. Although almost every nephron segment participates in the reabsorption of Na in the normal kidney, the proximal segments (from the glomerulus to the macula densa) and the distal segments (past the macula densa) play different roles. The proximal tubule and the thick ascending limb of the loop of Henle interact with the filtration apparatus to deliver Na to the distal nephron at a rather constant rate. This involves regulation of both *Department of Physiology and filtration and reabsorption through the processes of glomerulotubular balance and tubuloglomerular feedback. Biophysics, Weill- The more distal segments, including the distal convoluted tubule (DCT), connecting tubule, and collecting Cornell Medical duct, regulate Na reabsorption to match the excretion with dietary intake. The relative amounts of Na reabsorbed College, New York, in the DCT, which mainly reabsorbs NaCl, and by more downstream segments that exchange Na for K are variable, New York; and †Kidney Disease allowing the simultaneous regulation of both Na and K excretion. Branch, National Clin J Am Soc Nephrol 10: 676–687, 2015. doi: 10.2215/CJN.12391213 Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Introduction The precise adaptation of urinary Na excretion to di- Health, Bethesda, Daily Na intake in the United States averages approx- etary Na intake results from regulated processing of an Maryland imately 180 mmol (4.2 g) for men and 150 mmol (3.5 g) ultrafiltrate of circulating plasma by the renal tubular for women (1). -

Clinical and Histopathological Features of Renal Maldevelopment in Boxer Dogs: a Retrospective Case Series (1999–2018) †
animals Article Clinical and Histopathological Features of Renal Maldevelopment in Boxer Dogs: A Retrospective Case Series (1999–2018) † Maria Alfonsa Cavalera 1, Floriana Gernone 1, Annamaria Uva 1, Paola D’Ippolito 2, Xavier Roura 3 and Andrea Zatelli 1,* 1 Department of Veterinary Medicine, University of Bari, 70010 Valenzano, Italy; [email protected] (M.A.C.); fl[email protected] (F.G.); [email protected] (A.U.) 2 Veterinary diagnostic Lab ACV Triggiano, 70019 Triggiano, Italy; [email protected] 3 Hospital Clínic Veterinari, Universitat Autònoma de Barcelona, 08193 Bellaterra, Spain; [email protected] * Correspondence: [email protected]; Tel.: +39-080-4679804 † This study was partially presented as oral communication at the 11th ECVIM-CA/ESVIM Congress, Dublin (Ireland) as “Congenital nephrotic syndrome with renal glomerular immaturity in 7 Boxer dogs”. Zatelli, A., Domenech, O., Bussadori, C., Lubas, G., Del Piero, F. Simple Summary: This study describes clinical findings in Boxer dogs with renal maldevelopment and proposes a possible mode of inheritance. Medical records of 9 female Boxer dogs, older than 5 months and with a clinical diagnosis of proteinuric chronic kidney disease prior to one year of age, showed the presence of polyuria and polydipsia, decreased appetite, weight loss, lethargy and weakness in all affected dogs. Common laboratory findings were proteinuria and diluted urine, non- regenerative anemia, azotemia, hyperphosphatemia, hypoalbuminemia and hypercholesterolemia. Citation: Cavalera, M.A.; Gernone, Histopathology of the kidneys identified the presence of immature glomeruli in all dogs. In 7 out F.; Uva, A.; D’Ippolito, P.; Roura, X.; of 9 related dogs, the pedigree analysis showed that a simple autosomal recessive trait may be a Zatelli, A. -

Cerebrospinal Fluid in Critical Illness
Cerebrospinal Fluid in Critical Illness B. VENKATESH, P. SCOTT, M. ZIEGENFUSS Intensive Care Facility, Division of Anaesthesiology and Intensive Care, Royal Brisbane Hospital, Brisbane, QUEENSLAND ABSTRACT Objective: To detail the physiology, pathophysiology and recent advances in diagnostic analysis of cerebrospinal fluid (CSF) in critical illness, and briefly review the pharmacokinetics and pharmaco- dynamics of drugs in the CSF when administered by the intravenous and intrathecal route. Data Sources: A review of articles published in peer reviewed journals from 1966 to 1999 and identified through a MEDLINE search on the cerebrospinal fluid. Summary of review: The examination of the CSF has become an integral part of the assessment of the critically ill neurological or neurosurgical patient. Its greatest value lies in the evaluation of meningitis. Recent publications describe the availability of new laboratory tests on the CSF in addition to the conventional cell count, protein sugar and microbiology studies. Whilst these additional tests have improved our understanding of the pathophysiology of the critically ill neurological/neurosurgical patient, they have a limited role in providing diagnostic or prognostic information. The literature pertaining to the use of these tests is reviewed together with a description of the alterations in CSF in critical illness. The pharmacokinetics and pharmacodynamics of drugs in the CSF, when administered by the intravenous and the intrathecal route, are also reviewed. Conclusions: The diagnostic utility of CSF investigation in critical illness is currently limited to the diagnosis of an infectious process. Studies that have demonstrated some usefulness of CSF analysis in predicting outcome in critical illness have not been able to show their superiority to conventional clinical examination. -

Medicines That Affect Fluid Balance in the Body
the bulk of stools by getting them to retain liquid, which encourages the Medicines that affect fluid bowels to push them out. balance in the body Osmotic laxatives e.g. Lactulose, Macrogol - these soften stools by increasing the amount of water released into the bowels, making them easier to pass. Older people are at higher risk of dehydration due to body changes in the ageing process. The risk of dehydration can be increased further when Stimulant laxatives e.g. Senna, Bisacodyl - these stimulate the bowels elderly patients are prescribed medicines for chronic conditions due to old speeding up bowel movements and so less water is absorbed from the age. stool as it passes through the bowels. Some medicines can affect fluid balance in the body and this may result in more water being lost through the kidneys as urine. Stool softener laxatives e.g. Docusate - These can cause more water to The medicines that can increase risk of dehydration are be reabsorbed from the bowel, making the stools softer. listed below. ANTACIDS Antacids are also known to cause dehydration because of the moisture DIURETICS they require when being absorbed by your body. Drinking plenty of water Diuretics are sometimes called 'water tablets' because they can cause you can reduce the dry mouth, stomach cramps and dry skin that is sometimes to pass more urine than usual. They work on the kidneys by increasing the associated with antacids. amount of salt and water that comes out through the urine. Diuretics are often prescribed for heart failure patients and sometimes for patients with The major side effect of antacids containing magnesium is diarrhoea and high blood pressure. -

SIRS Is Valid in Discriminating Between Severe and Moderate Diabetic Foot Infections
Pathophysiology/Complications ORIGINAL ARTICLE SIRS Is Valid in Discriminating Between Severe and Moderate Diabetic Foot Infections 1 2 DANE K. WUKICH, MD KATHERINE MARIE RASPOVIC, DPM best of our knowledge, the use of SIRS 2 3 KIMBERLEE B. HOBIZAL, DPM BEDDA L. ROSARIO, PHD has not yet been validated as a method of discriminating between moderate and severe DFI. OBJECTIVEdThis retrospective, single-center study was designed to distinguish severe di- The aim of this study was to classify abetic foot infection (DFI) from moderate DFI based on the presence or absence of systemic fl infectionseverityinagroupofhospital- in ammatory response syndrome (SIRS). ized diabetic patients based on the pres- RESEARCH DESIGN AND METHODSdThe database of a single academic foot and ence or absence of SIRS. The reason for ankle program was reviewed and 119 patients were identified. Severe DFI was defined as local hospitalization in this group of patients infection associated with manifestation of two or more objective findings of systemic toxicity was their DFI. Our hypotheses are that using SIRS criteria. patients with DFI who manifest SIRS (i.e., severe infection) will have longer hospital RESULTSdPatients with severe DFI experienced a 2.55-fold higher risk of any amputation – – stays and higher rates of major amputa- (95% CI 1.21 5.36) and a 7.12-fold higher risk of major amputation (1.83 41.05) than patients tion than patients who don’tmanifest with moderate DFI. The risk of minor amputations was not significantly different between the two groups (odds ratio 1.02 [95% CI 0.51–2.28]). The odds of having a severe DFI was 7.82 SIRS (i.e., moderate infection). -

Electrolyte Imbalance in Children with Severe Acute Malnutrition at a Tertiary Care Hospital in Pakistan: a Cross-Sectional Study
Open Access Original Article DOI: 10.7759/cureus.10541 Electrolyte Imbalance in Children With Severe Acute Malnutrition at a Tertiary Care Hospital in Pakistan: A Cross-Sectional Study Mohammad Raza 1, 2 , Sohail Kumar 3 , Muzamil Ejaz 2 , Dua Azim 3 , Saad Azizullah 2 , Azhar Hussain 4, 5 1. Pediatrics, The Indus Hospital, Karachi, PAK 2. Pediatrics, Dow Medical College, Dr. Ruth K. M. Pfau Civil Hospital, Karachi, PAK 3. Internal Medicine, Dow Medical College, Dr. Ruth K. M. Pfau Civil Hospital, Karachi, PAK 4. Healthcare Administration, Franklin University, Columbus, USA 5. Medicine, Xavier University School of Medicine, Oranjestad, ABW Corresponding author: Mohammad Raza, [email protected] Abstract Background Malnutrition is a significant public health concern and a leading contributor to the global burden of children’s diseases, affecting 50 to 150 million children under the age of five years worldwide. Globally, undernutrition accounts for approximately 33% of the deaths among under-fives. South Asia alone contributes to 50% and 38.8% of the world’s population of wasted and stunted children, respectively. In Pakistan, malnutrition is the leading cause of childhood mortality, accounting for nearly 35% of all deaths under five years of age. Severe acute malnutrition (SAM), the most severe form of malnutrition, is often associated with electrolyte imbalances. This study aimed to determine the frequency of electrolyte imbalance in children with SAM admitted at a tertiary care hospital. Methods This cross-sectional study includes 184 patients with SAM aged between 6 and 60 months, who were admitted at the inpatient Department of Pediatrics, Dr. Ruth K. -

Hormonal and Thirst Modulated Maintenance of Fluid Balance in Young Women with Different Levels of Habitual Fluid Consumption
nutrients Article Hormonal and Thirst Modulated Maintenance of Fluid Balance in Young Women with Different Levels of Habitual Fluid Consumption Evan C. Johnson 1,2,*, Colleen X. Muñoz 1,3, Liliana Jimenez 4, Laurent Le Bellego 4, Brian R. Kupchak 1,5, William J. Kraemer 1,6, Douglas J. Casa 1, Carl M. Maresh 1,6 and Lawrence E. Armstrong 1 1 Human Performance Laboratory, Department of Kinesiology, University of Connecticut, Storrs, CT 06269, USA; [email protected] (C.X.M.); [email protected] (B.R.K.); [email protected] (W.J.K.); [email protected] (D.J.C.); [email protected] (C.M.M.); [email protected] (L.E.A.) 2 Division of Kinesiology and Health, University of Wyoming, Laramie, WY 82071, USA 3 Department of Health Sciences and Nursing, University of Hartford, West Hartford, CT 06117, USA 4 Hydration & Health Department, Danone Research, Palaiseau 91767, France; [email protected] (L.J.); [email protected] (L.L.B.) 5 Department of Military and Emergency Medicine, Uniformed Services University of the Health Sciences, Bethesda, MD 20814, USA 6 Department of Human Sciences, the Ohio State University, Columbus, OH 43210, USA * Correspondence: [email protected]; Tel.: +1-307-766-5282; Fax: +1-307-766-4098 Received: 22 February 2016; Accepted: 11 May 2016; Published: 18 May 2016 Abstract: Background: Surprisingly little is known about the physiological and perceptual differences of women who consume different volumes of water each day. The purposes of this investigation were to (a) analyze blood osmolality, arginine vasopressin (AVP), and aldosterone; (b) assess the responses of physiological, thirst, and hydration indices; and (c) compare the responses of individuals with high and low total water intake (TWI; HIGH and LOW, respectively) when consuming similar volumes of water each day and when their habitual total water intake was modified. -
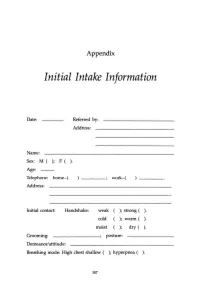
Initial Intake Information
Appendix Initial Intake Information Date: Referred by: Address: Name: Sex: M ( ); F ( ). Age: Telephone: home-( work-( Address: Initial contact: Handshake: weak ); strong ( ). cold ); warm ( ). moist ); dry ( ). Grooming: ________; posture: Demeanor/attitude: Breathing mode: High chest shallow ( ); hyperpnea ( ). 307 308 APPENDIX Sighing: frequent ( ); occasional ( ); absent ( ). Occupation: Contact with: dust ( ); fibers (); paints ( ); solvents ( ); sprays ( ); detergents ( ). Other chemicals or airborne particles: Status: Married ( ); single ( ); divorced ( ); other: children: No. Boys ( ); No. Girls ( ). Physician(s) of record: Last medical examination: _________,199__ Diagnos(e)s: 'Ireatmentts): Medication(s): Do you now have, have you ever had, or has any family member related to you by blood (mother, father, sister, brother, familial grandparents or uncles and aunts) had: ( ) High blood pressure () Heart disease APPENDIX 309 ) Low blood pressure ) Angina ) Diabetes (insulin-dependent) ) Anemia ) Diabetes (non-insulin- ) Allergies dependent) ) Dermatitis ) Colitis ) Muscle spasms ) Gastritis ) Tingling in hands and/or feet ) Ulcer ) Fainting (syncope) ) Shortness of breath ) Dizziness (vertigo) ) Asthma ) Stroke ) Emphysema ) Headache ) Hyperventilation ) TMJlbruxism ) Mitral valve prolapse ) Chronic low backache ) Other heart murmur ) EB virus (mononucl.) ) Heart arrhythmia ) PMS ) Chronic vaginal yeast ) Chronic tiredness ) Cystitis ) Menstrual irregul. ) Raynaud's disease ) Tinnitus ) Chronic pain ) Hyperthyroid ) Eating disorder -

Basic Skills in Interpreting Laboratory Data, 5Th Edition
CHAPTER 1 DEFINITIONS AND CONCEPTS KAREN J. TIETZE This chapter is based, in part, on the second edition chapter titled “Definitions and Concepts,” which was written by Scott L. Traub. Objectives aboratory testing is used to detect disease, guide treatment, monitor response Lto treatment, and monitor disease progression. However, it is an imperfect sci ence. Laboratory testing may fail to identify abnormalities that are present (false After completing this chapter, negatives [FNs]) or identify abnormalities that are not present (false positives, the reader should be able to [FPs]). This chapter defines terms used to describe and differentiate laboratory • Differentiate between accuracy tests and describes factors that must be considered when assessing and applying and precision laboratory test results. • Distinguish between quantitative, qualitative, and semiqualitative DEFINITIONS laboratory tests Many terms are used to describe and differentiate laboratory test characteristics and • Define reference range and identify results. The clinician should recognize and understand these terms before assessing factors that affect a reference range and applying test results to individual patients. • Differentiate between sensitivity and Accuracy and Precision specificity, and calculate and assess Accuracy and precision are important laboratory quality control measures. Labora these parameters tories are expected to test analytes with accuracy and precision and to document the • Identify potential sources of quality control procedures. Accuracy of a quantitative assay is usually measured in laboratory errors and state the terms of an analytical performance, which includes accuracy and precision. Accuracy impact of these errors in the is defined as the extent to which the mean measurement is close to the true value.