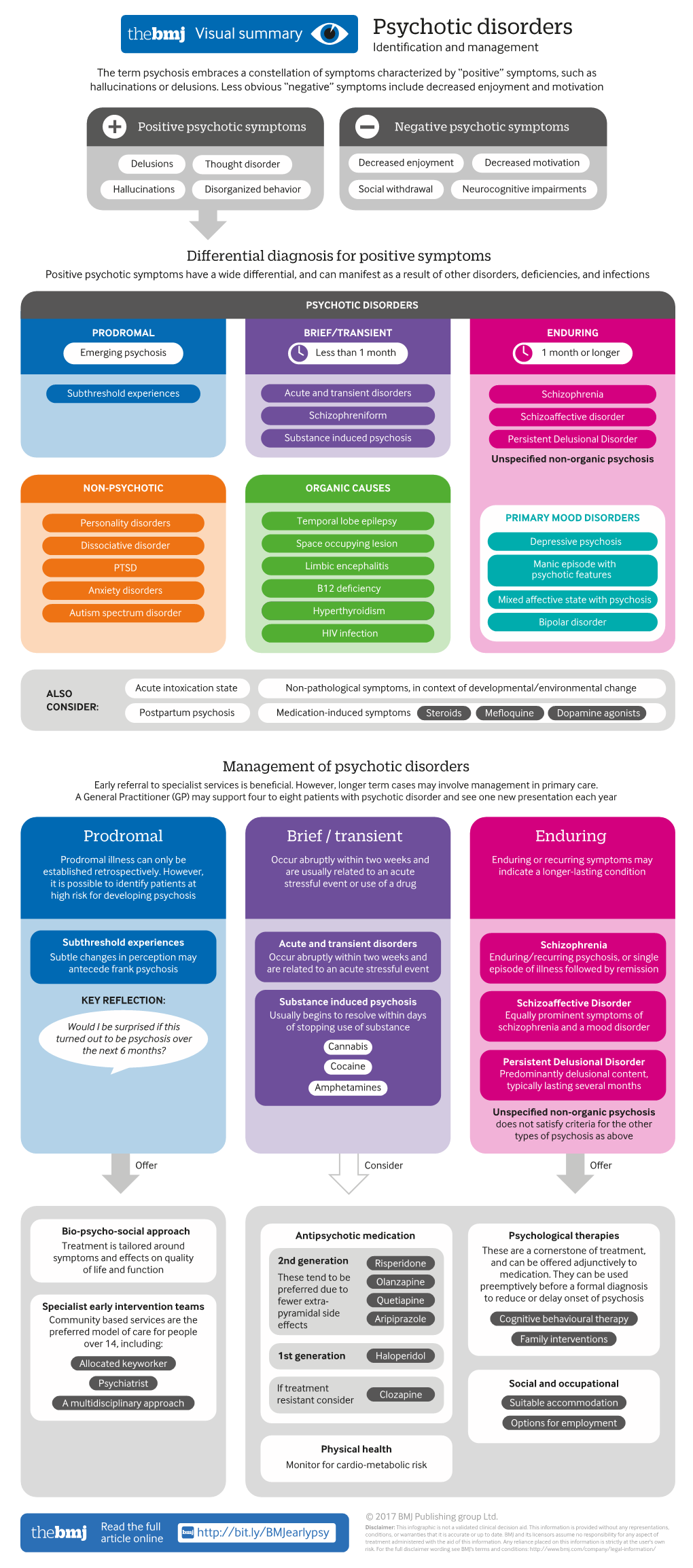
Psychotic Disorders Identification and Management
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

First Episode Psychosis an Information Guide Revised Edition
First episode psychosis An information guide revised edition Sarah Bromley, OT Reg (Ont) Monica Choi, MD, FRCPC Sabiha Faruqui, MSc (OT) i First episode psychosis An information guide Sarah Bromley, OT Reg (Ont) Monica Choi, MD, FRCPC Sabiha Faruqui, MSc (OT) A Pan American Health Organization / World Health Organization Collaborating Centre ii Library and Archives Canada Cataloguing in Publication Bromley, Sarah, 1969-, author First episode psychosis : an information guide : a guide for people with psychosis and their families / Sarah Bromley, OT Reg (Ont), Monica Choi, MD, Sabiha Faruqui, MSc (OT). -- Revised edition. Revised edition of: First episode psychosis / Donna Czuchta, Kathryn Ryan. 1999. Includes bibliographical references. Issued in print and electronic formats. ISBN 978-1-77052-595-5 (PRINT).--ISBN 978-1-77052-596-2 (PDF).-- ISBN 978-1-77052-597-9 (HTML).--ISBN 978-1-77052-598-6 (ePUB).-- ISBN 978-1-77114-224-3 (Kindle) 1. Psychoses--Popular works. I. Choi, Monica Arrina, 1978-, author II. Faruqui, Sabiha, 1983-, author III. Centre for Addiction and Mental Health, issuing body IV. Title. RC512.B76 2015 616.89 C2015-901241-4 C2015-901242-2 Printed in Canada Copyright © 1999, 2007, 2015 Centre for Addiction and Mental Health No part of this work may be reproduced or transmitted in any form or by any means electronic or mechanical, including photocopying and recording, or by any information storage and retrieval system without written permission from the publisher—except for a brief quotation (not to exceed 200 words) in a review or professional work. This publication may be available in other formats. For information about alterna- tive formats or other CAMH publications, or to place an order, please contact Sales and Distribution: Toll-free: 1 800 661-1111 Toronto: 416 595-6059 E-mail: [email protected] Online store: http://store.camh.ca Website: www.camh.ca Disponible en français sous le titre : Le premier épisode psychotique : Guide pour les personnes atteintes de psychose et leur famille This guide was produced by CAMH Publications. -

INTERVIEW with ROBERT BLOCH - 1 - by Jean-Marc Lofficier
INTERVIEW WITH ROBERT BLOCH - 1 - By Jean-Marc Lofficier INTERVIEW WITH ROBERT BLOCH Randy and Jean-Marc Lofficier RL: Who do you consider to be at the root of your inspiration for your writing of terror and horror fiction? RB: Well, I spent eleven years in an advertising agency! Actually, as a child I was interested in reading that sort of thing. But, I was more interested, and I think most imaginative children are, in the mysteries of death, age and cruelty. Why do these things happen? Why do people do these things to one another? An innocent child believes in the protection and security of his daddy and mama, his friends and his safe home environment. Then to read and learn about these things is a great shock. I've done a good deal of talking with many other contemporary writers of this sort of fiction, people like Stephen King, Peter Straub, Richard Matheson and half-a- dozen others. They all had the same experience; they all feel this was their motivation. Some kids don't think about these things particularly, but I did. Particularly when I was hiding under the bed or in the closet after seeing something like Lon Chaney in The Phantom of the Opera for the first time at the age of 8 or 9. I decided, as I guess most of these people did, if you can't lick ‘em, join ‘em. So, I learned the method of what it is that terrifies other people as well. Yet, I tried to do it in a way that is safe. -

Psychos' Haunting Memories: A(N) (Un)Common Literary
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Repositório Científico da Universidade de Évora Sanglap Vol. 1 No. 1 Psycho’s Haunting Memories Psychos’ Haunting Memories: A(n) (Un)common Literary Heritage Maria Antónia Lima // University of Évora Sanglap: Journal of Literary and Cultural Inquiry Issue: Terror and the Literary, Vol. I No. I Editors: Arka Chattopadhyay and Sourit Bhattacharya Email: [email protected] Link: http://sanglap-journal.in/ 0 Maria Antónia Lima Sanglap Vol. 1 No. 1 Psycho’s Haunting Memories Psychos’ Haunting Memories: A(n) (Un)common Literary Heritage In his homage to Edgar Allan Poe, Lou Reed attached a text to the album entitled Raven (2003), where he says: “Edgar Allan Poe is that most classical of American writers – a writer more peculiarly attuned to our new century’s heartbeat than he ever was to his own. Obsessions, paranoia, wilful acts of self-destruction surround us constantly. Though we age we still hear the cries of those for whom the attraction to mournful chaos is monumental.” Because of this common contemporary feeling, our age can be called, what Teresa Brennan has termed “the age of paranoia” (Brennan 20). Everything we experience seems to belong to a global world of technological information that gives us access to instantaneous “contact”, giving also the feeling that we live in a reality that does not exist, or only exists in our minds as a kind of imaginary construct, leading to what Freud called a fixation in a narcissistic state of being. -

The Birth of Haptic Cinema
The Birth of Haptic Cinema An Interactive Qualifying Project Submitted to the Faculty of WORCESTER POLYTECHNIC INSTITUTE In partial fulfillment of the requirements for the Degree of Bachelor of Science by Panhavuth Lau Jordan Stoessel Date: May 21, 2020 Advisor: Brian Moriarty IMGD Professor of Practice Abstract This project examines the history of The Tingler (1959), the first motion picture to incorporate haptic (tactile) sensations. It surveys the career of its director, William Castle, a legendary Hollywood huckster famous for his use of gimmicks to attract audiences to his low- budget horror films. Our particular focus is Percepto!, the simple but effective gimmick created for The Tingler to deliver physical “shocks” to viewers. The operation, deployment and promotion of Percepto! are explored in detail, based on recently-discovered documents provided to exhibitors by Columbia Pictures, the film’s distributor. We conclude with a proposal for a method of recreating Percepto! for contemporary audiences using Web technologies and smartphones. i Contents Abstract .......................................................................................................................................... i Contents ........................................................................................................................................ ii 1. Introduction .............................................................................................................................. 1 2. William Castle .......................................................................................................................... -

The Psychology of Satan Jennifer Putnam This Paper Was Written for Dr
The Psychology of Satan Jennifer Putnam This paper was written for Dr. Thomas! Milton course. It was presented at the 2009 Sigma Tau Delta International Convention. John Milton!s Satan is a psychologically complex character. Satan has qualities which make him a brilliant leader, but which also cause him great pain. He is a militant ruler with powerful speeches, and a cunning deceiver with rich disguises. The actions Satan takes, however, cause him great an- guish. It is through his soliloquies that Satan takes off his mask and reveals the troubled person he really is. John Milton in Paradise Lost portrays Satan as a proud, passionately manipulative, and complex character that endures an internal conflict from which he cannot escape. Though Milton begins his masterpiece in medias res, we must start from the beginning with Satan as the angel Lucifer. Lucifer enjoys his high stature in Heaven, until the Son is anointed instead of him, and he becomes jeal- ous. It is then that Lucifer draws emotionally away from God and Heaven. James Holley Hanford and James Taaffe show the results of this jealousy by commenting, “Following God!s announcement of the Son!s elevation, Satan initially defected from the angelic forces” (172). His defection is a result of be- ing too proud of being a servant, which leads to anger and thus, his rebellion. Royland Frye points out the irony of Satan!s refusal to become a slave in that Satan actually becomes a slave to his emotions. Frye says, “As a result of his choice, he becomes a slave to what would, psychologically, be called an "ego- deal,! an identification of the self with an impossible image,” (35). -

DREAMS and Occultisml 1 [The Topic of the Last Three Paragraphs Was First Raised by Freud in Chapters II and III of Beyond the Pleasure Principle (1920G)
Warning Concerning Copyright Restrictions The Copyright Law of the United States (Title 17, United States Code) governs the making of photocopies or other reproductions of copyrighted materials. Under certain conditions specified in the law, libraries and archives are authorized to furnish a photocopy or other reproduction. One of these specified conditions is that the photocopy or reproduction is not to be used for any purpose other than private study, scholarship, or research. If electronic transmission of reserve material is used for purposes in excess of what constitutes "fair use," that user may be liable for copyright infringement. THE STANDARD EDITION OF THE COMPLETE PSYCHOLOGICAL WORKS OF SIGMUND FREUD Translated from the German under the General Editorship of JAMES STRACHEY In Collaboration with ANNA FREUD Assisted by ALIX STRACHEY and ALAN TYSON VOLUME XXII (1932-36) New Introductory Lectures on Psycho-Analysis and Other Works SIGMUND FREUD IN 1929 LONDON THE HOGARTH PRESS AND THE INSTITUTE OF PSYCHO-ANALYSIS 30 NEW INTRODUCTORY LECTURES here offering us an extreme case; but we must admit that child hood experiences, too, are of a traumatic nature, and we need not be surprised if comparatively trivial interferences with the LECTURE XXX function of dreams may arise under other conditions as well,l DREAMS AND OCCULTISMl 1 [The topic of the last three paragraphs was first raised by Freud in Chapters II and III of Beyond the Pleasure Principle (1920g). Further LADIEs AND GENTLEMEN,-To-day we will proceed along a allusions to it will be found in Lecture XXXII, p. 106 below.] narrow path, but one which may lead us to a wide prospect. -

Psycho by Charles Taylor “The a List: the National Society of Film Critics’ 100 Essential Films,” 2002
Psycho By Charles Taylor “The A List: The National Society of Film Critics’ 100 Essential Films,” 2002 Reprinted by permission of the author The impact of Alfred Hitchcock’s “Psycho” owes so much to its two big surprises that when the film opened in 1960 Hitchcock not only refused to allow press screenings but had theaters hire Pinkerton security guards to prevent latecomers from entering the theater once the picture had started. He wanted to keep the people who hadn’t bought tickets from finding out that Janet Leigh’s Marion Crane is stabbed to death in the shower only forty-five minutes into the movie, and that the murderer is Antho- ny Perkins’s Norma Bates, who has succumbed to the personality of the mother he murdered years before. In many ways, “Psycho” seems like a death knell for the studio system that would lumber on for a few more years before collapsing later in the decade under the weight of filmmakers and audiences sick of the old stultified formu- Alfred Hitchcock holding a clapper on the set of “Psycho.” las. It isn’t just that Hitchcock made the film fast and on Courtesy Library of Congress the cheap (it cost only $800,000), using the crew from his television anthology series “Alfred Hitchcock Presents.” We are as anxious for Norman not to be found out cover- And it’s not just the shock of the shower murder, its bril- ing up “mother’s” crime as we were for Marion not to get liant and savage elisions heralding and in many cases sur- caught stealing the $40,000 that started her on the jour- passing the screen violence to come. -

Film Music: Hitchcock's Psycho Transcript
Film Music: Hitchcock's Psycho Transcript Date: Wednesday, 15 October 2008 - 12:00AM FILM MUSIC: HITCHCOCK'S PSYCHO Professor Roger Parker At the end of the last lecture, my first in this series about film music, we were in the early 1930s, in the company of an exuberantly screaming Fay Wray as she heralded the appearance of her exceptionally tall and exceptionally dark leading man. The musical accompaniment was an equally exuberant symphonic score by Max Steiner, one of the great composers of the period. As I said then, there are plenty of ways in whichKing Kong now looks dated in both visual and musical terms; but there are equally striking ways in which Steiner's score marks the appearance of a set of codes about how music was to interact with the visual element of films: codes that to some extent remain with us to this very day. One of the most obvious of these codes was in Steiner's use of what we in the music trade call leitmotifs: prominent themes that become attached to aspects of the unfolding drama and that then recur, sometimes with significant development, when those aspects recur in the narrative. And so, in King Kong, the gentle string theme that accompanied the heroine's onboard love scene comes back, played by the full orchestra and horribly distorted, as the camera settles on her, struggling to escape becoming the next sacrificial victim to the monster of Skull Island. This was, of course, an old trick borrowed (as were so many film-music devices) from opera: the obvious point of reference is the leitmotif system elaborated at huge length in Wagner's operas, but the technique goes back a good deal further. -

The Bates Motel a Case Study in the Importance of the Ordinary by Stephen Leonard and Keith A
The Bates Motel A case study in the importance of the ordinary By Stephen Leonard and Keith A. Sculle s is usually the case when people live near Aa significant historical H establishment or structure, they usually take it for granted or are ambivalent as to its importance. The familiarity of the structure causes people to take it for granted as they pass by it on a regular basis. They just do not view it as significant or important. This is under- standable. However, it is important and necessary to research and docu- ment such a structure and place it into the correct cultural and historical context. This is even more important for the community and surrounding area. The structure was placed at its Bates Motel. Courtesy Stacie Peecher. specific location for a reason. The helping anchor the small, unincorpo- because they were owner-managed, structure becomes apart of the fabric rated town of Bates’ business commu- these lodgings superseded the cabins, of the community. In a greater sense, nity since the dawn of the nation’s camps, cottages, or villages as roadside it may also represent an important surge in prosperity after World War 2. lodgings were known earlier in the historical theme within the state or Following the decade of the Great twentieth century. Motels offered nation. The structure itself does not Depression and, during the early- security and comfort in a domestic have to be a high end example of an 1940s self-sacrifice in international style familiar to post-war auto travelers. architectural style or place where war, most Americans experienced and Yet, the name motel was more mod- Lincoln slept. -

Psycho INDIANA UNIVERSITY PRESS FILMGUIDE SERIES Harry Geduld and Ronald Gottesman, General Editors Filmguide to Psycho
Filmguide. to Psycho INDIANA UNIVERSITY PRESS FILMGUIDE SERIES Harry Geduld and Ronald Gottesman, General Editors Filmguide to Psycho JAMES NAREMORE INDIANA UNIVERSITY PRESS Bloomington London Copyright© 1973 by Indiana University Press All rights reserved No part of this book may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying and recording, or by any information storage and retrieval system, without permission in writing from the publisher. The Association of American University Presses Resolution on Permissions constitutes the only exception to this prohibition. Published in Canada by Fitzhenry & Whiteside Limited, Don Mills, Ontario Library of Congress catalog card number: 72-88636 ISBN: 0-253-39307-8 cl. 0-253-39308-6 pa. Manufactured in. the United States of America 2 3 4 5 6 80 79 78 77 76 For Jay, who likes horror movies I would like to thank Harry Geduld and Ron Gottesman for giving me this opportunity. My thanks also to Murray Sperber and Charles Eckert, who spent hours talking with me about Psycho. J,N, contents 1 Credits 3 2 Outline 5 3 Aesthetics of Repression 9 4 The Production 19 5 Analysis 25 6 Summary Critique 72 A Hitchcock Filmography 81 Selected Bibliography 83 Rental Sources 87 vii -- Filmguide to Psycho ---- 1 . credits PSYCHO Paramount Pictures, 1960 Producer: Alfred Hitchcock Direction Alfred Hitchcock Screenplay Joseph Stephano, from the novel by Robert Bloch Photography John L. Russell, A.s.c. Special EfJects Clarence Champagne Art Direction Joseph Hurley, Robert Clatworthy Sets George Milo Music Bernard Herrmann Sound Engineering Waldon Watson, William Russell Title Design Saul Bass Editing George Tomasini Assistant Director Hilton Green Costumes Helen Colvig Time 109 minutes Filmed in Hollywood, partly on the lots of the old Universal Stu dios. -

The Acutely Psychotic Patient – Assessment and Initial Management
THEME Psychosis The acutely psychotic patient Assessment and initial management Nicholas Keks BACKGROUND MBBS, MPM, PHD, FRANZCP, Acute psychosis is a medical emergency; apart from distress and behavioural dysfunction, there may be danger to the is Professor, Monash patient and others. Urgent assessment and management is essential. Although involvement of specialist services is University, Delmont Hospital, usual, general practitioners may need to initiate initial treatment and, in more remote areas, provide complete care. and Mental Health Research Institute of Victoria. nicholas. OBJECTIVE [email protected] This article aims to update the GP about the initial management of the acutely psychotic patient. Grant Blashki DISCUSSION MD, FRACGP, is Senior General practitioners will frequently be the initial source of assistance for patients with acute psychosis and their Research Fellow, Department families. The patient with first episode psychosis may pose particular challenges, especially as insight about the of General Practice and need for treatment is often poor. The first step is to establish a therapeutic alliance, enabling history, examination and Program Evaluation Unit, University of Melbourne, and investigations. While it is necessary to establish the presence of psychosis, precise diagnosis is usually a secondary Honorary Senior Lecturer, consideration. Risk assessment must be carried out to decide whether the patient can be managed in the community or Health Services Research, needs inpatient care. Kings College London. Acute psychosis is the presence of the mental state It should be noted that psychosis often occurs only briefly where appreciation of reality is impaired, as evidenced during the course of the disorder, and patients suffering by the presence of psychotic symptoms such as from these disorders may not manifest any psychosis, delusions, hallucinations, mood disturbance, and especially if treated. -

PSYCHO NOTES 1. the Mother, Norma Bates, Is a Classic Super-Ego Character, Internalized by Norman. the Tension in the Film Comes
PSYCHO NOTES 1. The Mother, Norma Bates, is a classic super-ego character, internalized by Norman. The tension in the film comes from not knowing that she is actually dead and mummified. She is the ‘thing that refuses to die’ in the sense that Norman’s internalization of her keeps her alive and her body is not buried but treated as alive. 2. The house is a classic ‘uncanny’ house: Victorian, high on a hill, ‘empty’. The house contains the secret, and getting into the house stages the attempts to uncover the truth. 3. The theme of voyeurism is a perversion that is itself perverted. Instead of leading to sexual pleasure, Norman adopts the persona of his mother to kill Marion Crane. His pleasure is sadistic rather than sexual or, rather, he derives sexual pleasure from the stabbing — as God seems to do in the case of Sta. Theresa. 4. The drain and the eye dominate the shower scene; this is the Real! The camera wanders away, pausing to look at objects in the room, and then drifts out the window toward the house. 5. The role of the voice is key. Normal ventriloquizes his mother’s voice, staging conversations that the audience takes to be actual until they discover the mother’s corpse. Is there, like in Vertigo, a phrase? Possibly the shift in the role of the acousmatic voice is an indicator that Psycho is a different kind of ‘discourse’. 6. What is the meaning of the taxidermy theme, apart from the role it plays in explaining Norman’s anxiety to preserve the mother’s body.