Shaping Workflows in Digital and Remote Diabetes Care During the COVID-19 Pandemic Via Service Design Prospective, Longitudinal, Open-Label Feasibility Trial
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Braunprize 2012 Is Looking for Ingenious Solutions and Product Ideas to Make Our Everyday a Better Place
Our everyday has become an artificial environment of architecture and technology and while it seems that the quantity of products around us is consistently increasing, their level of quality is not. We have surrounded ourselves by many things we don´t really value, instead of focusing on fewer but better solutions to help us live our lives. With this in mind, the BraunPrize 2012 is looking for ingenious solutions and product ideas to make our everyday a better place. 4 5 4 Editorial 6 Index 8 About the BraunPrize 18 Jury Statements 34 Students 36 Finalists 44 Sustainability Awards 50 National Winners 68 Special Mentions 84 Professionals & Enthusiasts 86 Finalists 94 Sustainability Award 98 National Winners 116 Special Mentions 126 Appendix 6 7 BraunPrize Jury Statement Students Professionals Appendix Why do we promote design? When the BraunPrize was established in 1968, it was Germany’s first international competition to promote the importance of industrial design and the work of young When Erwin Braun, son of Braun founder Max Braun, established Germany´s first designers. Braun’s continuous commitment to this cause has been highly regarded international design prize in 1968 – the BraunPrize – it was originally introduced to by the design world and the design-aware public ever since. stimulate public debate about design, at a time when understanding and awareness of design and its positive benefits were largely unknown. The objective of the BraunPrize today is to promote the work of young and established Forty-four years later, the focus on promoting design itself is no longer the highest designers from all over the world, to value the work of design schools, design teams priority. -
[email protected] & [email protected]
[email protected] & [email protected] DESIGNIT… Oslo Stockholm Aarhus Copenhagen London Berlin New York Munich San Francisco Barcelona Madrid Tokyo Tel Aviv Bangalore Medellín Lima 17 550+ 40 Offices Employees Nationalities Sydney 3 F U T U R E S 5 DÉT DER BETYDER NOGET IMORGEN BLIVER BYGGET IDAG Vi lever lever I en teknologisk brydningstid. Forandring. disruption. Fart. Vi ved ikke, hvor vi ender - men vi kan påvirke retningen! F U T U R E S FUTURES ER EN LEGEPLADS. 2018: Prototyping Futures in Copenhagen F U T U R E S TRUSTING Hvordan kan vi bygge transparens og ansvarlighed ind INVISIBILITY i de systemer vi ikke kan se? PLAYFUL Hvordan kan vi bruge leg til at UNLEARNING reboote vores hjerner? ENHANCING Hvordan kan vi leve i symbiose HUMANITY med teknologien? F U T U R E S TRUSTING INVISIBILITY F U T U R E S VERDEN BESTÅR I STIGENDE GRAD AF USYNLIGE SYSTEMER 2 500 000 000 000 000 000 mb data hver dag 200 milliarder “smart devices” I 2020 I 2020, vil 85% af alle kundeinteraktioner blive administreret af en maskine F U T U R E S I 10 ud af 15 sektorer er tilliden konsekvent dalet i de senere år Stigende mistillid til politiske institutioner - globalt USA har oplevet det største fald på tillidsbarometret af alle vestlige lande TILLIDEN DALER. F U T U R E S TILLID ER ESSENTIELT F U T U R E S TILLID KAN DESIGNES - MEN HVORDAN? …er noget man gør sig fortjent til …handler om transparens …implicerer gensidighed …handler også om friktion …forudsætter empati F U T U R E S AI VR AR MR ADI ADD AE “Artificial empathy (AE) er udviklingen af AI systemer, som fx Robotter, der kan afkode og reagere på menneskelige følelser”. -

Media Release Singapore Is First City to Host INDEX: Award 2011 Exhibition on Global Tour
Media Release Singapore is First City to Host INDEX: Award 2011 Exhibition on Global Tour The biennial INDEX: Award, worth €500,000, is not only the biggest, but possibly the most important design award because of its focus on ‘Design to Improve Life’. INDEX: Award 2011 Exhibition has kicked off its global tour with Singapore as its first port of call. Singaporeans will be the first to see the winning designs and finalists of INDEX: Award 2011 from 4 – 19 February 2012 at the plaza in front of The Cathay building after its premiere in Copenhagen. 2. The Danish Ambassador to Singapore, His Excellency Ole Lisborg, will officially launch the INDEX: Award 2011 Exhibition in Singapore at The Cathay on 8 February 2012. “On behalf of Denmark, I am very pleased to welcome such an entrepreneurial and innovative collection of life-improving designs to Singapore,” said Mr Lisborg. He will be accompanied by Dr Lee Boon Yang, Chairman of Keppel Corporation, the main exhibition sponsor, and Mr Robert Tomlin, Chairman of the DesignSingapore Council, the exhibition organiser and host. (See Annex A for more details on the exhibition.) 3. INDEX: Award 2011 Exhibition features the winning designs and finalists of the biggest design award in the world. The biennial INDEX: Award, worth €500,000, is not only the biggest, but possibly the most important design award because of its focus on „Design to Improve Life‟. „Design to Improve Life‟ is a global movement about innovative designs that improve life for people around the world. Many around the world are using the same vocabulary, ideas and processes that are at the heart of INDEX:, which is to enlist creative people to work on urgent global challenges. -

Designit Spain Digital, S.L
DESIGNIT SPAIN DIGITAL, S.L. (Sole Shareholder Company) Annual Accounts corresponding to the financial year ending on March 31, 2021 TABLE OF CONTENTS ▪ Balance Sheet as of March 31, 2021 ▪ Profit and Loss Account corresponding to the period between April 1, 2020 and March 31, 2021. ▪ Statement of Changes to Equity corresponding to the period between April 1, 2020 and March 31, 2021. ▪ Cash Flow Statement corresponding to the period between April 1, 2020 and March 31, 2021. ▪ Annual Report corresponding to the period between April 1, 2020 and March 31, 2021. ▪ Management Report corresponding to the period between April 1, 2020 and March 31, 2021. Designit Spain Digital S.L (Sole shareholder company) Balance Sheet as of March 31, 2021 and as of March 31, 2020 (Expressed in Euros) Concept Note 31.03.2021 31.03.2020 ASSETS 1.228.673 3.716.532 NON-CURRENT ASSETS 386.709 2.559.591 Tangible Fixed Assets 5 160.737 232.103 Land & Buildings 0 0 Technical Installations and other fixed assets 160.737 232.103 Long-term Investments in Group Companies and Associates 6 197.904 1.773.253 Asset Instruments 197.904 1.773.253 Long term financial investments 6 28.068 38.188 Other investments 28.068 38.188 Assets due to deferred taxes 10 0 516.047 CURRENT ASSETS 841.964 1.156.941 Commercial Debtors and other receivables 6 499.725 824.997 Clients due to sales and provision of services 499.725 824.997 Clients for sales and provision of services in the short term 488.580 808.985 Clients companies of the group 11.145 16.012 Assets for current tax 0 0 Short term -

Dit2018as Pdf.Pdf
John Maeda Design in Tech Report 2018 https://designintechreport.wordpress.com Team Founding Team Report Contributors Report Translators Jackie Xu Aviv Gilboa Fatimah Kabba Bon Ku Ling Fan Sunil Malhotra Takram Medicine China India Japanese Justin Sayarath John Maeda Luis Arnal Latin America 2018 Design In Tech Report | Welcome 2 / 91 Welcome to a new format for the Design in Tech Report. For this year’s report, I Welcome took a stab at learning all the CSS/JS that I’ve always wanted to know, and then went after the task of making a fully responsive report. I’ve partially succeeded on my road there with this letterbox-only version — which is better than a PDF. And fortunately thanks to Takram's Shota Matsuda it is greatly improved. If you see Refresh Screen If Needed please refresh your window and a dynamic diagram is likely to reappear. Chrome seems to work best with this report. If you don’t like an interactive version like this, please visit the one** on Slideshare. Expect a video version on my new YouTube channel “John Maeda is Learning” some day that walks you through all these findings. —@johnmaeda 2018 Design In Tech Report | Welcome 4 / 91 Sections 1) TBD = Tech × Business × Design 2) Scaling Design How do technology, business, and design How do you scale the design function in a interrelate in the startup and corporate company to impact business at the speed of Overview ecosystems? Moore’s Law? 3) Computational Design: 1st Steps 4) Computational Design × A.I. What is “computational design” and why does it How does artificial intelligence -

Cxsummit Designit Shared
we’re Designit γεια σας 5 We are… Oslo Aarhus Stockholm Edinburgh Copenhagen …a global strategic design agency, making London Munich Tokyo New York innovation happen for some of the world’s most Madrid ambitious companies. San Francisco Barcelona Tel Aviv We grow businesses by designing desirable, Bangalore feasible and viable experiences. Medellin We merge strategy, design & technology to create products, services, systems and spaces. Lima Together, we are 550+ designers, business strategists and human needs experts in 16 global studios. We believe everything can and should be designed. And everything we design should matter. Products, services, systems and spaces – that people love. Design Because what matters to people, matters to business. what matters What we do… Products and Transformation Professional New services programs education ventures We design meaningful products, We help clients transform their We teach and develop design-driven We help clients of all sizes identify, services, systems and spaces, organisation, their way-of-work and mindsets within organisations to explore, launch and scale new that improve the way all of us their ability to continuously improve increase profit, spark creativity and businesses, disrupt industries and live, work, and do business. and innovate their entire business. boost innovation efforts. create new revenue streams. Use the grid as a guide. Clients we’ve worked with. Our Approach We typically work from insights to implementation. Our five-step framework is user-centric, experience-led and co-creative. Disruptive Future Experience Experience Continuous insights vision roadmap design delivery Research and Direction and Transformation roadmap Solution and Development and opportunities experience concept and future customer prototyping implementation journeys It’s about Customer Intent, not Customer Channel. -

Design Thinking in Higher Education for Promoting Human-Centred Inno- Vation in Business and Society
Design Thinking in Higher Education for Promoting Human-centred Inno- vation in Business and Society Erasmus+ KA2 Project 2017-1-EE01-KA203-034889 O1. Learning needs analysis and development of methodological learning frameworks for design thinking in higher education Circulation: Public Partners: UTH, CERTH-IRETETH, TLU, IPP, METROPOLIA Authors: H. Tsalapatas, O. Heidmann, K. Pata, Merja Bauters, C. Vaz de Carvalho Version: 01 Stage: Final Date: 2/7/2018 Co-funded by the Erasmus+ Program of the European Union. CONTRIBUTORS Despoina Stylla Nadia Vlahoutsou Christina Taka Vlastaridis Panagiotis Velentzas Chronis Eka Jeladze Rita Durão 14/4/2013 Validation Strategy Report 2 Table of Contents CONTRIBUTORS 2 EXECUTIVE SUMMARY 7 1. INTRODUCTION AND DESIGNIT PROJECT RATIONALE 10 2. DESIGNIT HIGH LEVEL OBJECTIVES 14 3. EXPECTED OUTCOMES 16 4. DESIGNIT INNOVATION 22 5. DESIGNIT STAKEHOLDERS 26 6. DESIGN THINKING RETROSPECTIVE, STRATEGIES AND PRACTICES 30 6.1 ENTREPRENEURSHIP AND SOCIAL ENTREPRENEURSHIP 30 6.2 DESIGN THINKING AND ITS TERMINOLOGY 33 6.3 EMPIRICAL STUDY RESULTS ON DESIGN METHODS 34 6.4 DESIGN THINKING AS A PROBLEM SOLVING APPROACH OR PROCESS 35 6.4.1 Design thinking as a solution-based approach 35 6.4.2 Design thinking as a creative approach 36 6.4.3 Design thinking as a user-centred approach brings design into business world 36 6.4.4 Core attributes of design thinking 37 6.4.5 Characteristics of design thinkers 38 6.5 THE DESIGN THINKING PROCESS AND ITS VARIOUS DESCRIPTIONS 39 6.5.1 Design methods versus design process 40 6.5.2 A review of design thinking process stages 40 6.5.3 The non-linear nature of design thinking 42 6.5.4 Design thinking principles 42 6.5.4 Popular design thinking frameworks 43 6.5.5 Examples of design thinking solutions 45 6.6 A CLOSER LOOK AT THE 5 STAGE DESIGN THINKING MODEL 47 O2 3 6.6.1 Stage 1 - Empathise 47 6.6.2 Stage 2 - Define 50 6.6.3 Stage 3 - Ideate 52 6.6.4 Stage 4 - Prototype 53 6.6.5 Stage 5 - Test 54 6.7 HISTORICAL RETROSPECTIVE OF THE DESIGN THINKING PROCESS 55 7. -

Wipro Limited - Update on Material Event
March 15, 2021 Wipro Limited - Update on Material Event Summary of rating(s) outstanding Instrument* Previous Rated Amount Current Rated Amount Rating Outstanding Fund-based (interchangeable) Rs. 696.00 crore Rs. 696.00 crore [ICRA]AAA(Stable)/[ICRA]A1+ facilities Fund-based (interchangeable) USD 965.00 million USD 965.00 million [ICRA]AAA(Stable)/[ICRA]A1+ facilities Non-fund based facilities Rs. 2,799.10 crore Rs. 2,799.10 crore [ICRA]AAA(Stable) Non-fund based facilities USD 70.70 million USD 70.70 million [ICRA]AAA(Stable) Unallocated - Non-fund Rs. 8,666.33 crore Rs. 8,666.33 crore [ICRA]AAA(Stable)/[ICRA]A1+ based/fund-based facilities Total Rs. 20,000.00 crore Rs. 20,000.00 crore *Instrument details are provided in Annexure-1 Rationale Material event On March 4, 2021, Wipro Limited (Wipro) notified the stock exchange that it has signed an agreement to acquire a 100% stake in The Capital Markets Company (Capco) Group (through its holding companies – Cardinal US Holdings, Inc. and Cardinal Foreign Holdings S.à.r.l., and its Indian subsidiary – Capco Technologies Private Limited). The transaction is expected to be completed during the quarter ending June 30, 2021, subject to requisite regulatory approvals and customary closing conditions. The acquisition is for an all-cash deal of USD 1.45 billion and is not a related-party transaction. Established in 1998, Capco is a global technology and management consultancy specialising in driving digital transformation in the financial services industry. It has an experienced executive team and over 5,000 world-class business and technology consultants based across more than 30 global locations. -

Designing Easy Access to Care for First Episode Psychosis in Complex Organizations
Designing easy access to care for first episode psychosis in complex organizations Kristin Lie Romma,b , Erlend Strand Gardsjordb, c, Kristine Gjermundsenb, Manuela Aguirre Ulload,e, Lars-Christian Berentzenb, Ingrid Melle a,b a Institute of Clinical Medicine, KG Jebsen Centre for Psychosis Research and Norwegian Centre for Mental Disorders Research, Faculty of Medicine, University of Oslo, 0318 Oslo, Norway b Division of Mental Health and Addiction, Oslo University Hospital, 0407 Oslo, Norway c Institute of Clinical Medicine, Faculty of Medicine, University of Oslo, 0318 Oslo, Norway d The Oslo School of Architecture and Design, 0175 Oslo, Norway e Designit, 0172 Oslo, Norway *Corresponding author: Kristin Lie Romm, Tel: 0047 97009863, E-mail: [email protected], Postal address: Early Intervention In Psychosis Advisory Unit for South East Norway, Oslo University Hospital, Gaustad sykehus, Sognsvannsveien 21, Oslo, Norway E-mail addresses: [email protected] [email protected] [email protected] [email protected] [email protected] 1 Abstract Aims: Developing early intervention services (EIS) in health care organizations (HCOs) is difficult because it is necessary to integrate service approaches across units. To accommodate the needs of patients and relatives, Oslo University Hospital (OUH) chose to use service design (SD) to redesign their first-episode services with an emphasis on easy access to care. This paper discusses the results and how SD can help to overcome known barriers to change in complex organizations. Method: SD is a method that relies on principles of participation, innovation and visualization to develop coherent services. The method emphasizes the exploration of a problem area from the perspective of multiple stakeholders to create a shared understanding of the complexity. -

Design Thinking for Business Transformation
professional Design Thinking for Business Transformation TECHNICAL FILE Summer Design Thinking for Business Transformation – 5th edition Credits: 5. − The educational planning of all IED Master courses is based on the criteria set by the European Higher Education Area (EHEA). − IED Master employs a system of credits that follows the structure of the European Credit Transfer and Accumulation System (ECTS). − IED Master issues its own exclusively private degrees. Language: English. − A TOEFL 550 or IELTS 6.5 level of language knowledge or equivalent is required for those students whose mother tongue is not English. − Some classes and/or lectures may be given by international guests and in these cases the working language will be English or Spanish. There is also the chance that additional educational material or recommended activities will be provided in English and/or Spanish. Unlocking IED Barcelona, welcome activity for international students: June 28th 2019 (optional attendance). Duration: 1st to 5th July 2019. Timetable: Monday to Friday from 9.30 am to 1.30 pm and from 3 pm to 7 pm. Some sessions may take place outside these hours in the case of making up for missed classes or extra activities. SUMMER Professional / Design Thinking for Business Transformation, a.y. 2019-2020 2 PRESENTATION Design Thinking for Business Transformation are concepts that have tremendous impact in today’s business strategy. They are the ingredients that spur new growth opportunities, optimize business processes and create strong connections with customers. We see these words everywhere we look today. But what do they really define? Are they real? Do they have any real impact on business or are they just a series of trendy words slapped on company slogans, advertisements, and annual reports? Design Thinking is a human-centric group of work processes and frameworks that help identify, develop and deliver on these concepts creatively and efficiently. -

Cslogin 20062019164633 Prju
••••• • • • • •• • • .• .••••••• ... .. wip:ro))!•........••. • • ••••••• • •••••• • • •• • June 20, 2019 The Manager- Listing BSE Limited (BSE: 507685) The Manager- Listing National Stock Exchange of India Limited, (NSE: WIPRO) The Market Operations, NYSE: New York (NYSE: WIT) Dear Sir/Madam, Sub: Press Release We are enclosing a copy of Press Release which is being released today. For WIPRO LIMITED ~~ M.Sanaulla Khan Company Secretary ~hlftgistered"'' Office: Mpro Llrnlttct T : +91(80) 2844 0011 Doddakannelli F : +~1 (80) 2844 0054 8arjapur Road E : [email protected] Bengaluru 560 035 W : wipro.com India C : L32102t<A1945PLC020800 ••••• • • • •••••••••••• • wip"r§.~>)i 4 ••••••• •••••••••• • Wipro Launches Pivotal Software Center of Excellence in Dallas, Texas Company expands digital capabilities and opens a Designit studio Dallas, Texas, USA and Bangalore, India - June 20, 2019: Wipro Limited (NYSE: WIT, BSE: 507685, NSE: WIPRO), a leading global information technology, consulting and business process services company, and Pivotal Software, Inc. (NYSE: PVTL), a leading cloud-native platform provider, announced today the official opening of the Pivotal Center of Excellence at Wipro's Dallas office, to accelerate the innovation and digital transformation capabilities offered to joint customers. Wipro will expand its Dallas footprint and hire locally to help deliver these capabilities and other innovations. In addition, Wipro will expand the design services it offers clients by opening a new Designit studio in Dallas. Designit, which is part of Wipro, provides strategic design, service design and design thinking services from Its other US locations in New York City and San Francisco and 16 studios around the world. A Strategic Partnership for Digital Transformation The Pivotal Center of Excellence in Dallas will serve as a co-creation lab for both Wipro and Pivotal to build new solutions with their joint customers as well as demonstrate examples of digital transformation outcomes they have achieved with clients. -
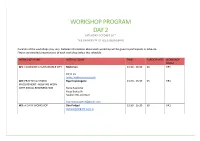
Workshop Program Day 2 Saturday October 26Th the University of Oslo (Blindern)
WORKSHOP PROGRAM DAY 2 SATURDAY OCTOBER 26TH THE UNIVERSITY OF OSLO (BLINDERN) Duration of thE workshops may vary. DEtailEd information about Each workshop will bE givEn to participants in advancE. PlEasE sEE dEtailEd prEsEntations of Each workshop bElow this schedule. WORKSHOP NAME INSTRUCTED BY TIME PARTICIPANTS WORKSHOP ROOM W1: CO-DESIGN A SUSTAINABLE CITY Mobimeo 13:30 - 16:30 20 GR4 Anne Liu [email protected] W2: PRACTICAL CITIZEN Byantropologene 13:30 - 16:30 25 GR1 INVOLVEMENT - HOW WE WORK WITH SOCIAL REGENERATION RunE KvErnmo Katja BratsEth MaikEn Riis EilErtsEn [email protected] W3: A DIRTY WORKSHOP Dan Podjed 13:30 - 16:30 30 UR1 [email protected] W4: THE ESSENTIAL ROLE OF FOOD IN RMIT Europe and RMIT University, Australia 13:30 - 16:30 30 UR2 SUSTAINING CITIES Dr. FErnE Edwards and Dr. Roos GErritsEn [email protected] W5: THE PEOPLE PROJECT The People Project 13:30 - 16:30 25 UR3 Sara Arko [email protected] MarrijE Prins W6: GAMING FUTURES Designit 13:30 - 16:30 12 GR2 ChristophEr RobErt FiEldhousE PEarsEll-Ross [email protected] W7: DESIGNING POLICIES FOR With Company 13:30 - 16:30 24 GR7 SUSTAINABLE TERRITORIES MiguEl Coutinho [email protected] W8: ANTHROPOLOGY AND CREATIVE Halo Ethnographic Bureau 13:30 - 16:30 12 GR3 ENTREPRISE LouisE Pasteur dE Faria [email protected] Livia StroschoEn [email protected] W9: CO-DESIGN OF FUTURE CITY Halmstad University 13:30 - 16:30 30 StorE MOBILITY SOLUTIOS - FROM A MULTI- møterom STAKEHOLDER PERSPECTIVE VaikE Vors [email protected]