ORIGINAL ARTICLE Soft Tissue Cephalometric Analysis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A New Dimension of Success in Your Practice
3D Imaging Family A new dimension of success in your practice dentsplysirona.com CEREC® Diagnosis Treatment Plan Guided Endodontics Airway Functional Orthodontics Integration Implantology Analysis Occlusal & TMD 2/3 Good reasons for 3D With 3D imaging, you have the ideal basis for a new dimension of success in your practice. Best image quality at a low dose and shorter visits—that is what Dentsply Sirona 3D X-ray units provide for your practice. These BETTER benefits provide greater certainty to help make difcult diagnoses Communicate with easier, while providing the opportunity to explore new options for stunning images implantology, endodontics, orthodontics, and more. to your patients Thanks to the 3D Family, Galileos® Comfort Plus, Orthophos® SL 3D and Orthophos XG 3D patients have a better understanding of the diagnosis and accept treatment more readily. It all adds up to efcient clinical workflow that leads to greater practice success. Enjoy every day. With Dentsply Sirona. SAFER Predictable diagnosis and treatment options FASTER Efcient clinical workflow 4/5 More insight More possibilities Your patients are candidates for 3D more often than you think. How severe is the bone atrophy or the periapical lesion? Is the tooth impacted? In all dental disciplines, there are numerous questions that can be answered far more easily using 3D imaging with CBCT. 3D CBCT from Dentsply Sirona ofers clinicians and specialists numerous When does 3D provide more certainty? options for diagnosis, treatment plans, patient consultation—all with a seamless, efcient workflow. This is one way you can expand your range Areas Cases of services and treat more patients at your practice. -

Class II Article
Journal of the World Federation of Orthodontists 4 (2015) 40e49 Contents lists available at ScienceDirect Journal of the World Federation of Orthodontists journal homepage: www.jwfo.org Case Report A new, no-compliance class II correction strategy using nickel-titanium coil-springs Luca Lombardo a,*, Antonella Carlucci b, Francesca Cervinara c, Giuseppe Siciliani d a Adjunct Professor, Postgraduate School of Orthodontics, University of Ferrara, Ferrara, Italy b Postgraduate Student, Postgraduate School of Orthodontics, University of Ferrara, Ferrara, Italy c Private Practice in Bari, Italy d Chairman of Postgraduate School of Orthodontics, Department of Orthodontics, University of Ferrara, Ferrara, Italy article info abstract Article history: Background: Correcting Class II malocclusion with Class II elastics or functional appliances requires great Received 15 October 2014 patient collaboration. Here we describe two Class II cases successfully treated with an alternative Received in revised form approach using a fixed device designed to obviate compliance. 27 November 2014 Methods: We fitted specific Class II springs to the bilateral hooks on the stainless steel maxillary and Accepted 3 December 2014 mandibular archwires of a full fixed appliance to correct the Class II malocclusion and to promote Available online 14 February 2015 mandibular growth. Results: The new device brought about full Class I canine and molar relationships in both treated cases Keywords: Class II and improved the maxillomandibular relationship without relying on patient collaboration. Compliance-free Conclusion: Class II springs appear to be a simple, fast, and effective alternative approach to Class II Spring correction, facilitating mandibular growth even in noncompliant patients. Ó 2015 World Federation of Orthodontists. -

Cephalometric and Malocclusion Analysis of Kadazan Dusun Ethnic Orthodontic Patients (Analisis Sefalometrik Dan Maloklusi Pesakit Ortodontik Etnik Kadazan Dusun)
Sains Malaysiana 42(1)(2013): 25–32 Cephalometric and Malocclusion Analysis of Kadazan Dusun Ethnic Orthodontic Patients (Analisis Sefalometrik dan Maloklusi Pesakit Ortodontik Etnik Kadazan Dusun) ROHAYA MEGAT ABDUL WAHAB* HARTINI IDRIS, HABIBAH YACOB & SHAHRUL HISHAM ZAINAL ARIFFIN ABSTRACT The aims of this study were to assess the skeletal pattern and the malocclusion of Kadazan Dusun ethnic patients who seek for orthodontic treatment. Cephalometric radiographs (248) and 345 study models were collected from four orthodontic clinics in Sabah. The cephalometric mean values (SNA, SNB, ANB, MMA, SNMxP, UIMxP, LIMnP and ALFH) were measured and the study models were analysed for overjet, overbite, incisor and molar relationships. Some morphological or occlusal features such as shovel shape, Talon cusp, peg shape teeth, midline diastema, canine displacement and supernumerary tooth were also noted. The frequency and correlation of cephalometric mean values and prevalence of malocclusion were analysed using SPSS 18. Class I Skeletal pattern was the most common (48%) followed by Class II (33%) and Class III (18%). There was a strong correlation between SNA and SNB values (>0.70). Class II/1 incisor relationship has the highest frequency (41%) followed by Class III (32%), Class I (21%) and Class II/2 (6%). Class II Molar relationship of both right and left showed highest frequency (38%) followed by Class I (33%) and Class III (30%). Increased of overjet (44%) and reduced overbite (41%) and shovel-shaped incisor were the most common occlusal and dental features. The Kadazan Dusun patients who seek for orthodontic treatment in Sabah were mostly presented with Class I Skeletal pattern with high prevalence in Class II/1 incisor relationship, Class II molar relationship, increased overjet and reduced overbite. -

The Frontal Cephalometric Analysis – the Forgotten Perspective
CONTINUING EDUCATION The frontal cephalometric analysis – the forgotten perspective Dr. Bradford Edgren delves into the benefits of the frontal analysis hen greeting a person for the first Wtime, we are supposed to make Educational aims and objectives This article aims to discuss the frontal cephalometric analysis and its direct eye contact and smile. But how often advantages in diagnosis. when you meet a person for the first time do you greet them towards the side of the Expected outcomes Correctly answering the questions on page xx, worth 2 hours of CE, will face? Nonetheless, this is generally the only demonstrate the reader can: perspective by which orthodontists routinely • Understand the value of the frontal analysis in orthodontic diagnosis. evaluate their patients radiographically • Recognize how the certain skeletal facial relationships can be detrimental to skeletal patterns that can affect orthodontic and cephalometrically. Rarely is a frontal treatment. radiograph and cephalometric analysis • Realize how frontal analysis is helpful for evaluation of skeletal facial made, even though our first impression of asymmetries. • Identify the importance of properly diagnosing transverse that new patient is from the front, when we discrepancies in all patients; especially the growing patient. greet him/her for the first time. • Realize the necessity to take appropriate, updated records on all A patient’s own smile assessment transfer patients. is made in the mirror, from the facial perspective. It is also the same perspective by which he/she will ultimately decide cephalometric analysis. outcomes. Furthermore, skeletal lingual if orthodontic treatment is a success Since all orthodontic patients are three- crossbite patterns are not just limited to or a failure. -

2016-Chapter-143-Oropharyngeal-Growth-And-Malformations-PPSM-6E-1.Pdf
To protect the rights of the author(s) and publisher we inform you that this PDF is an uncorrected proof for internal business use only by the author(s), editor(s), reviewer(s), Elsevier and typesetter Toppan Best-set. It is not allowed to publish this proof online or in print. This proof copy is the copyright property of the publisher and is confidential until formal publication. Chapter c00143 Oropharyngeal Growth and Skeletal Malformations 143 Stacey Dagmar Quo; Benjamin T. Pliska; Nelly Huynh Chapter Highlights p0010 • Sleep-disordered breathing (SDB) is marked by manifestations has not been determined. The varying degrees of collapsibility of the length and volume of the airway increase until pharyngeal airway. The hard tissue boundaries the age of 20 years, at which time there is a of the airway dictate the size and therefore the variable period of stability, followed by a slow responsiveness of the muscles that form this decrease in airway size after the fifth decade of part of the upper airway. Thus, the airway is life. The possibility of addressing the early forms shaped not only by the performance of the of this disease with the notions of intervention pharyngeal muscles to stimulation but also by and prevention can change the landscape the surrounding skeletal framework. of care. u0015 • The upper and lower jaws are key components • Correction of specific skeletal anatomic u0025 of the craniofacial skeleton and the deficiencies can improve or eliminate SDB determinants of the anterior wall of the upper symptoms in both children and adults. It is airway. The morphology of the jaws can be possible that the clinician may adapt or modify negatively altered by dysfunction of the upper the growth expression, although the extent of airway during growth and development. -

Craniofacial Growth Nasal Septum Deviation
International Journal of Pediatric Otorhinolaryngology 74 (2010) 1180–1183 Contents lists available at ScienceDirect International Journal of Pediatric Otorhinolaryngology journal homepage: www.elsevier.com/locate/ijporl Craniofacial growth in children with nasal septum deviation: A cephalometric comparative study Luca D’Ascanio a,b,*, Carla Lancione a, Giorgio Pompa b, Elena Rebuffini c, Nicola Mansi d, Marco Manzini a a Department of Otolaryngology – Head & Neck Surgery, Citta` di Castello Civil Hospital, Citta` di Castello (Perugia), Italy b Department of Dentistry and Maxillo-Facial Surgery, ‘‘La Sapienza’’ University of Rome, Rome, Italy c Department of Maxillo-Facial Surgery, University of Ferrara, Ferrara, Italy d Department of Otolaryngology, ‘‘Santobono–Pausilipon’’ Children’s Hospital, Naples, Italy ARTICLE INFO ABSTRACT Article history: Objective: Nasal-breathing impairment has been described as a possible determinant of maxillofacial Received 2 April 2010 development in children with adenoids/tonsils hypertrophy. However little is known about the possible Received in revised form 13 July 2010 influence of nasal septum deviation on craniofacial growth in childhood. We conducted a multicenter Accepted 15 July 2010 cephalometric study to compare skeletal and dental features in children with chronic nasal-breathing Available online 9 August 2010 obstruction secondary to nasal septum deviation and nose-breathing controls. Methods: Ninety-eight children (59M, 39F; mean age 8.8 years; age range 7–12 years) with obligate Keywords: mouth-breathing secondary to nasal septum deviation (group 1) and 98 age- and sex-matched nasal- Craniofacial growth breathing controls (group 2) were evaluated. Nasal-breathing function was assessed in all patients with Nasal septum Childhood clinical history, ENT instrumental examination and anterior active rhinomanometry. -
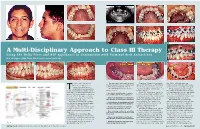
A Multi-Disciplinary Approach to Class III Therapy Using the Delta Force and ALF Appliances in Conjunction with Terminal Arch Extractions
Fig. 3 Fig. 9 Fig. 10 Fig. 11 Fig. 1 Fig. 2 Fig. 4 Fig. 14 Fig. 12 Fig. 13 A Multi-Disciplinary Approach to Class III Therapy Using The Delta Force and ALF Appliances in Conjunction with Terminal Arch Extractions By J. Wellington (Skip) Truitt, DDS & Livier Carreon-Truitt, DDS Fig. 15 Fig. 5 Fig. 6 Fig. 7 Fig. 16 Fig. 17 Fig. 18 he use of the low friction The panoramic radiograph showed Treatment began by placing an the .020 x .020 arch wire was Delta Force appliance in the third molars to be developing very upper ALF appliance on First Molar replaced every sixty days with a new conjunction with the bio- well in all four quadrants. (Fig. 9) Bands with standard pre-adjusted arch wire of the same type and gauge. compatible forces generated The following was the proposed .022 buccal tubes containing 10° of The treatment objective for this byT the ALF appliance creates a new treatment plan: torque. (Fig. 10) first phase of therapy was to develop approach to treating under-developed Composite ledges were placed on the maxillary arch over the mandibular • Develop the maxilla using a combina- arches. It is now possible to develop tion of ALF and Delta Force appliances. both the left and right maxillary 1st arch. Once this first phase of treat- the size of both the upper or lower bicuspids to secure the crescent wires ment was accomplished therapy could arch and level, align and torque the • Remove the mandibular second molars of the ALF appliance. (Fig. 11) All be initiated on the lower arch. -

The Airway, Breathing and Orthodontics
FACHLICH Kieferorthopädie & Atmung The Airway, Breathing and Orthodontics Dr. David C. Page & Dr. Derek Mahony Airway, Breathing and Malocclusion Abstract The airway, mode of breathing, and malocclusion are so inter-related during growth and development that Dentists need to play a bigger role in managing airway form can follow function and function can follow form. development and craniofacial formation even though Since form can follow function and function can follow the relationship between the airway, breathing and mal- form both should be treated preventively, as early as occlusion remains quite controversial. Certainly, the air- possible. way, mode of breathing, and craniofacial formation are so inter-related during growth and development that It is certain that dysfunction of the human airway and form can follow function and function can follow form. breathing can cause malocclusion and skeletal de- So, it is imperative to normalize form and function as formation. Prolonged oral respiration (obligate mouth early as possible, so that function is optimized for life. breathing) often results in dental and skeletal malforma- tion in growing children. Some of these negative chan- Introduction ges included excessive molar eruption, clockwise ro- tation of the mandible, increased anterior vertical face Dentists need to be more involved in managing airway height, retrognathia and open bite. Often related and development and craniofacial formation in growing created low tongue posture can result in reduced late- children. Already, dentists are increasingly involved in ral expansion and anterior development of the maxilla.2 managing the care and airways of patients of all ages with sleep-related breathing disorders, which are com- Conversely, craniofacial malformation and/or malocclu- mon and often associated with vascular complications sion can negatively impact airway and breathing func- such as arterial hypertension, coronary heart disease tion. -

Cephalometric Analysis for Orthognathic Surgery
Review article Annals and Essences of Dentistry 10.5368/aedj.2015.7.3.3.1 CEPHALOMETRIC ANALYSIS FOR ORTHOGNATHIC SURGERY 1 Sowmya B Rao 1 Post graduate 2 Gowri sankar Singaraju 2 Professor 3 Prasad Mandava 3 Professor and Head 4 Vivek Reddy Ganugapanta 4 Reader 1-4 Department of Orthodontics, Narayana Dental College, Nellore, Andhra Pradesh, India. ABSTRACT: The key for successful orthognathic surgery is the precise and careful diagnosis of facial, skeletal and dental problems. The cephalometric analysis for orthognathic surgery shows the orthodontist the horizontal and vertical positions of the facial bones by the use of a steady harmonized system. The sizes of the bones are represented by direct linear measurements whereas the shapes are measured by angular measurements. This analysis has been imperative for diagnosis and treatment planning of orthognathic surgery. The landmarks and measurements selected in the analysis can be altered by numerous surgical procedures. The rectilinear measurements can be transferred readily to a case study for mock surgery to learn further. And finally the comprehensive appraisal encompasses all of the facial bones and a cranial base for reference. To make it clinically practical, the analysis has been reduced to its most relevant and significant measurements. Because the measurements in cephalometric analyses are primarily linear, they may be eagerly applied to prediction overlays and serve as a basis for the assessment of other post treatment stability options. KEYWORDS: Cephalometric analysis, Orthognathic surgery INTRODUCTION: to the natural head position) or differences that concern Cephalometric analysis performed on the lateral the criteria for selecting the ‘normal’ sample, such as cephalometric radiograph provides details about skeletal occlusal features and skeletal background, at any given structure relationships as well as relationships between time. -

Prevalence of Skeletal Components of Malocclusion Using Composite Cephalometric Analysis
Pakistan Oral & Dent. Jr. 23 (2) Dec 2003 PREVALENCE OF SKELETAL COMPONENTS OF MALOCCLUSION USING COMPOSITE CEPHALOMETRIC ANALYSIS *WAHEED-UL-HAMID, BDS, MCPS, MS. (Orthodontics) **SAAD ASAD, FCPS-II (Trainee) ABSTRACT The purpose of this study was to find out the prevalence of skeletal components of malocclusion using composite cephalometric analysis. Cephalograms of a total of 100 patients were assessed. Patients who were selected had the following characteristics. Adult patients, all teeth present except 3'd molars, no supernumerary or retained tooth and no transverse skeletal discrepancy. The mean age of the sample was 18.28 years. 61% females and 39% were male patients. The results were as follows; Skeletal Class II was the most common antero-posterior malocclusion (47%). Among vertical malocclusions the most common was the skeletal open bite (38%) Bimaxillary proclination was the most common dental cephalometric finding (48%) Patients with orthognathic profile & competent lips were most common (34%) Components of various skeletal malocclusions were also assessed. Vertical growth pattern, dental inclinations, lip competency and profile of the patients were assessed in relation with sagital relationship. Identification of prevalence of malocclusion using cephalometrics seems to be an important method as it includes skeletal component of malocclusion. Key words: Prevalence, Components of malocclusion, Cephalometrics INTRODUCTION Purpose of this study was Researchers have employed different methods to • To find out the Prevalence of malocclusion in differentiate between the various components of mal- patients reporting at de`Montmorency College of occlusion. Most of the researchers have used Angle's Dentistry using Composite Cephalometric Classification1while others have used different Analysis indices2,3,4,5 to get information about prevalence6,7,8 and to quantify the severity of various features of • To find out the components of various malocclu- malocclusion. -

Mouth Breathing “A Habit Or Anomaly” – a Review
JIDAM eISSN 2582 - 0559 REVIEW ARTICLE “An Official Journal of IDA - Madras Branch”©2019. Available online MOUTH BREATHING “A HABIT OR ANOMALY” – A REVIEW Dr. B.N. Rangeeth, Dr. Priyaa Rangeeth* Professor, Department of Pedodontics, Thai Moogambigai Dental College,Chennai, Tamilnadu, India *Chief Consultant, Gums to Crowns Laser and Implant Dental Clinic, Chennai, Tamilnadu, India. To access & cite this article ABSTRACT Website: jidam.idamadras.com Mouth breathing has been discussed for quite some time but there is a need to increase the awareness about its effects on the dentofacial structures. The review focuses on the systemic and local effects of Mouth Breathing that includes the effects on psychological development including classification based on systemic influences. Though the dentofacial effects are discussed commonly the article aims to summate the systemic effects such as ADHD and sleep apnea that have an effect on the overall development for children. Management strategies such as nasal patches shows the importance of a parallel ENT therapy to be incorporated for better success. KEYWORDS : Airway Obstruction, Mouth Breathing, Address for correspondence: Hypoxia, Sleep Apnea Syndrome, Respiratory insufficiency. Dr. B.N. Rangeeth., MDS., Professor, Department of Pedodontics, Thai Moogambigai Dental College Chennai, India E-mail: [email protected] Received : 28.11.2019 Accepted : 17.12.2019 Published : 27.12.2019 137 JIDAM/Volume:6/Issue:4/Pages 137 - 143/October - December 2019 Rangeeth et al : Mouth breathing is a habit or anomaly INTRODUCTION: had a greater chance of being mouth breathers. 6 Human infants are sometimes considered to EFFECTS OF MOUTH BREATHING ON be obligate nasal breathers, may also breath through OVERALL HEALTH: mouth or both. -

A Linear Cephalometric Analysis: Its Description and Application in Assessing Changes in the Maxilla After Orthodontic Treatment
Loyola University Chicago Loyola eCommons Master's Theses Theses and Dissertations 1965 A Linear Cephalometric Analysis: Its Description and Application in Assessing Changes in the Maxilla After Orthodontic Treatment Francis Peter Wall Loyola University Chicago Follow this and additional works at: https://ecommons.luc.edu/luc_theses Part of the Medicine and Health Sciences Commons Recommended Citation Wall, Francis Peter, "A Linear Cephalometric Analysis: Its Description and Application in Assessing Changes in the Maxilla After Orthodontic Treatment" (1965). Master's Theses. 2006. https://ecommons.luc.edu/luc_theses/2006 This Thesis is brought to you for free and open access by the Theses and Dissertations at Loyola eCommons. It has been accepted for inclusion in Master's Theses by an authorized administrator of Loyola eCommons. For more information, please contact [email protected]. This work is licensed under a Creative Commons Attribution-Noncommercial-No Derivative Works 3.0 License. Copyright © 1965 Francis Peter Wall A LINEAR CEPHALOMETRIC ANALYSIS: ITS DESCRIPTION AND APPLICATION IN ASSESSING CHANGES IN THE MAXILLA AFTER ORTHODONTIC TREATMENT BY F. PETER WALL A Thesis Submitted to the Faculty of the Graduate School of Loyola University in Partial Fulfillment of the Requirements for the Degree of Master of Science JUNE 1965 LIFE Francis Peter Wall was born in Chicago, Illinois on January 5, 1936. He was graduated from Leo High School in Chicago, Illinois in June, 1953. He entered Loyola University, Chicago, Illinois in September, 1953, as a pre-dental student, and was graduated from Loyola University Dental School in June, 1960, with the degree of Doctor of Dental Surgery.