Oromocto and Surrounding Area Health and Well-Being Needs Assessment, 2011
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

AT a GLANCE 2017 Oromocto, Gagetown, Fredericton Junction Area This Community Is 1 of 33 in New Brunswick
MY COMMUNITY AT A GLANCE 2017 Oromocto, Gagetown, Fredericton Junction Area This community is 1 of 33 in New Brunswick. Population: 18,427 Land Area (km2): 1,325 It is part of: The goal of My Community at a Glance is to empower Zone 3: Fredericton and River individuals and groups with information about our Valley Area communities and stimulate interest in building healthier communities. It can help us towards becoming increasingly engaged healthier New Brunswickers. The information provided in this profile gives a comprehensive view about the people who live, learn, work, take part in activities and in community life in this area. The information included in this profile comes from a variety of provincial and federal sources, from either surveys or administrative databases. Having the ability to access local information relating to children, youth, adults and seniors for a community is important to support planning and targeted strategies but more importantly it can build on the diversity and uniqueness of each community. The median household income is The main industries include: $65,082 Public administration Retail trade Health care and social assistance Accommodation and food services Construction See their health as being very good or excellent (%) 58 57 35 Youth of grade 6 to 12 Adults (18 to 64 years) Seniors (65 years and over) My Community About the New Brunswick Health Council: New Brunswickers have a right to be aware of the decisions The communities in this profile include: being made, to be part of the decision making process, and to be Blissville aware of the outcomes and cost of the health system. -
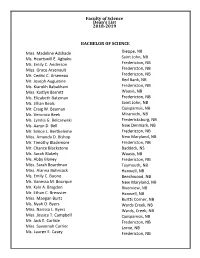
Faculty of Science Dean's List 2018-2019
Faculty of Science Dean's List 2018-2019 BACHELOR OF SCIENCE Miss. Madeline Adshade Dieppe, NB Ms. Heartswill E. Agbaku Saint John, NB Ms. Emily C. Anderson Fredericton, NB Miss. Grace Arsenault Fredericton, NB Mr. Cedric C. Arseneau Fredericton, NB Mr. Joseph Augustine Red Bank, NB Ms. Kiarokh Babakhani Fredericton, NB Miss. Kaitlyn Barrett Waasis, NB Ms. Elizabeth Bateman Fredericton, NB Ms. Jillian Beals Saint John, NB Mr. Craig W. Beaman Quispamsis, NB Ms. Veronica Beek Miramichi, NB Ms. Lyndia G. Belczewski Fredericksburg, NB Ms. Aaryn D. Bell New Denmark, NB Mr. Simon L. Bertheleme Fredericton, NB Miss. Amanda D. Bishop New Maryland, NB Mr. Timothy Blackmore Fredericton, NB Mr. Chance Blackstone Baddeck, NS Ms. Sarah Blakely Waasis, NB Ms. Abby Blaney Fredericton, NB Miss. Sarah Boardman Taymouth, NB Miss. Alanna Bohnsack Hanwell, NB Ms. Emily C. Boone Beechwood, NB Ms. Vanessa M. Bourque New Maryland, NB Mr. Kyle A. Bragdon Riverview, NB Mr. Ethan C. Brewster Hanwell, NB Miss. Maegan Burtt Burtts Corner, NB Ms. Nyah D. Byers Wards Creek, NB Miss. Narissa L. Byers Wards, Creek, NB Miss. Jessica T. Campbell Quispamsis, NB Mr. Jack E. Carlisle Fredericton, NB Miss. Savannah Carrier Lorne, NB Ms. Lauren E. Casey Fredericton, NB Mr. Kevin D. Comeau Mr. Nicholas F. Comeau Miss Emma M. Connell BACHELOR OF SCIENCE Ms. Jennifer Chan Fredericton, NB Mr. Benjamin Chase Fredericton, NB Mr. Matthew L. Clinton Fredericton, NB Miss. Grace M. Coles North Milton, PE Ms. Emma A. Collings Montague, PE Mr. Jordan W. Conrad Dartmouth, NS Mr. Samuel R. Cookson Quispamsis, NB Ms. Kelsey E. -

National Defence Team DEMOGRAPHICS ADVERTISE in 167 CANADIAN FORCES NEWSPAPERS LOCATED ACROSS CANADA Representing the Three CF Elements: Army, Air Force & Navy
MEDIA KIT REACH DND and the National Defence Team DEMOGRAPHICS ADVERTISE IN 167 CANADIAN FORCES NEWSPAPERS LOCATED ACROSS CANADA representing the three CF elements: Army, Air Force & Navy Canadian Forces COMMUNITY PROFILE Members of the CF and the Department of National Defence are powerful consumer groups. The National Defence Team Regular Force 64 000 Primary Reserve 34 500 Supplementary Reserve, Cadet Instructors Cadre and the Canadian Rangers 41 100 DND Public Servants 26 600 Total : 166 200 Regular Force DND 38% Public Servants 16% Supp. Reserve, Primary Cadet Inst. Reserve and Rangers 21% 25% *Data as of 2008 Statistics on the Canadian Forces members (Regular Force) Average age 35 Married or common-law 62% Married or common-law, with children 41% Reach this unique market Number of families 39 300 Average number of children 1.99 with only 1 point of contact! *Average income of officers $81 300 *Average income of non-commissioned members $55 600 * Based on average rank Captain/Corporal Stats are based on information provided by Director General Military Personnel and are current as of July 2008. CANADIAN FORCES NEWSPAPERS www.forcesadvertising.com OUR NEWSPAPERS Adsum The Aurora Borden Citizen Contact VALCARTIER GARRISON 14 WING GREENWOOD CFB BORDEN 8 WING TRENTON Québec, QC Greenwood, NS Borden, ON Trenton, ON The Courier Lookout North Bay Shield Petawawa Post 4 WING COLD LAKE CBF ESQUIMALT 22 WING NORTH BAY CFB PETAWAWA Cold Lake, AB Victoria, BC North Bay, ON Petawawa, ON The Post Gazette Servir The Shilo Stag Totem Times CFB GAGETOWN -

Fredericton Directory for Seniors
1 Personal Record The Fredericton Directory of Services for For additional copies phone 506-460-2020 Seniors is published and distributed by the For the online version, please visit: Fredericton Age-Friendly Community Advisory www.fredericton.ca Committee, and funded through a New Horizons Grant. Personal Record Name: __________________________________________________________________________________ Address: ________________________________________________________________________________ Civic Address: ____________________________________________________________________________ Postal Code: _____________________________________________________________________________ 2 Telephone: ______________________________________________________________________________ Social Insurance Number: __________________________________________________________________ Medicare Number: ________________________________________________________________________ Medical Insurance Provider & Number: _______________________________________________________ My bank or credit union: __________________________________________________________________ My church: ______________________________________________________________________________ My dentist: ______________________________________________________________________________ My electrician: ___________________________________________________________________________ My family physician: ______________________________________________________________________ My gas appliance service provider (furnace, boiler, stove): _______________________________________ -

FEATURES Milner’S BBQ
THE DRAGOON THE NATIONAL VOICE OF THE OLD COMRADES FEATURES Milner’s BBQ .............................................................. 6 Remembering .............................................................. 8 Things Aren’t Always as They Appear to Be............... 12 In Retrospect ............................................................... 14 Into The Trenches ........................................................ 18 DEPARTMENTS Messages The President ........................................................... 2 The Last Trumpet Call ............................................. 4 General Rick Hillier (retired) Mailbag .......................................................................... 5 OC, CMM, ONL, MSC, CD Patron of the RCD Association Chapter Reports Atlantic .................................................................... 20 Quebec ..................................................................... 24 Kingston .................................................................. 26 Ottawa Valley .......................................................... 28 National Capital Region .......................................... 30 BC ............................................................................ 32 Business Guild Donors ........................................................... 34 Secretary/Treasurer .................................................. 36 Association Executive .............................................. 37 Gathering of Dragoons 2016 ......................................... 38 BACKGROUND -

For an Extra $130 Bucks…
For an Extra $130 Bucks…. Update On Canada’s Military Financial Crisis A VIEW FROM THE BOTTOM UP Report of the Standing Senate Committee on National Security and Defence Committee Members Sen. Colin Kenny – Chair Sen. J. Michael Forrestall – Deputy Chair Sen. Norman K. Atkins Sen. Tommy Banks Sen. Jane Cordy Sen. Joseph A. Day Sen. Michael A. Meighen Sen. David P. Smith Sen. John (Jack) Wiebe Second Session Thirty-Seventh Parliament November 2002 (Ce rapport est disponible en français) Information regarding the committee can be obtained through its web site: http://sen-sec.ca Questions can be directed to: Toll free: 1-800-267-7362 Or via e-mail: The Committee Clerk: [email protected] The Committee Chair: [email protected] Media inquiries can be directed to: [email protected] For an Extra 130 Bucks . Update On Canada’s Military Financial Crisis A VIEW FROM THE BOTTOM UP • Senate Standing Committee on National Security and Defence November, 2002 MEMBERSHIP 37th Parliament – 2nd Session STANDING COMMITTEE ON NATIONAL SECURITY AND DEFENCE The Honourable Colin Kenny, Chair The Honourable J. Michael Forrestall, Deputy Chair And The Honourable Senators: Atkins Banks Cordy Day Meighen Smith* (Not a member of the Committee during the period that the evidence was gathered) Wiebe *Carstairs, P.C. (or Robichaud, P.C.) *Lynch-Staunton (or Kinsella) *Ex Officio Members FOR AN EXTRA $130 BUCKS: UPDATE ON CANADA’S MILITARY FINANCIAL CRISIS A VIEW FROM THE BOTTOM UP TABLE OF CONTENTS INTRODUCTION 7 MONEY ISN’T EVERYTHING, BUT . ............................................ 9 WHEN FRUGAL ISN’T SMART .................................................... -

Feed Grain Transportation and Storage Assistance Regulations
CANADA CONSOLIDATION CODIFICATION Feed Grain Transportation and Règlement sur l’aide au Storage Assistance Regulations transport et à l’emmagasinage des céréales C.R.C., c. 1027 C.R.C., ch. 1027 Current to November 21, 2016 À jour au 21 novembre 2016 Published by the Minister of Justice at the following address: Publié par le ministre de la Justice à l’adresse suivante : http://laws-lois.justice.gc.ca http://lois-laws.justice.gc.ca OFFICIAL STATUS CARACTÈRE OFFICIEL OF CONSOLIDATIONS DES CODIFICATIONS Subsections 31(1) and (3) of the Legislation Revision and Les paragraphes 31(1) et (3) de la Loi sur la révision et la Consolidation Act, in force on June 1, 2009, provide as codification des textes législatifs, en vigueur le 1er juin follows: 2009, prévoient ce qui suit : Published consolidation is evidence Codifications comme élément de preuve 31 (1) Every copy of a consolidated statute or consolidated 31 (1) Tout exemplaire d'une loi codifiée ou d'un règlement regulation published by the Minister under this Act in either codifié, publié par le ministre en vertu de la présente loi sur print or electronic form is evidence of that statute or regula- support papier ou sur support électronique, fait foi de cette tion and of its contents and every copy purporting to be pub- loi ou de ce règlement et de son contenu. Tout exemplaire lished by the Minister is deemed to be so published, unless donné comme publié par le ministre est réputé avoir été ainsi the contrary is shown. publié, sauf preuve contraire. -

HOULTON PIONEER TIMES Over a Century
Pre** Run Over A Century 4400 Copies Of Service 2 Section* In Aroostook HOULTON PIONEER TIMES County Tlx Only Newspaper in tbe World Interested in Houlton, Maine Vol. 105, No. 29 Houlton, Maine, Thursday, July 18, 1963 TEN CENTS 11RDC Claims Odor Problem Brochure To Explain Not Exclusive SAD Building Plans McLaughlin Says Facts Should Be Recognized Plans for the proposed million-doilar addition to Houlton High School will be pre In Fight For Controls in the form in detail the Aubrey A. McLaughlin, execu tive director of the Houlton Re gional Development Corporation, completion in stated when questioned this week about the obnoxious odors origin ating from the Aroostook Potato combined junior - senior high Product luc. plant area and the New Teachers Listed Meduxnekeag river area, that na turally none of us in this area, either businesses or individuals, For District Schools can willingly accept such a con dition. Not only is it obnoxious to us but it also could be some- what detrimental to business ac- tivity during the period of ex- treme conditions. However, he continued, a few facts should be the senior high school. The junior recognized as we fight this situa and senior high will be in the tion. same cluster of buildings, and will HOULTON NOT ALONE m adv share some common facilities. First, Houlton does not bold Proposed in the construction for top honors for a condition of this tion of principal of the Junior the junior high will be a separate nature. It is a condition that is High and Central Schools. -

Oromocto and Surrounding Area 2018 Community Health Needs Assessment
Oromocto and Surrounding Area 2018 Community Health Needs Assessment Blissville Hoyt Community Consultation Focus Burton Oromocto Fredericton Junction Oromocto First Nation Coping as a family with young children Rural living Gagetown Tracy Health Promotion services Seniors and seniors supports Living with special needs Social supports in the community Geary Upper Gagetown Military family health and wellbeing Women’s health Gladstone Primary Care access Youth and youth supports Community Advisory Representation Health and Wellness Priorities Improve access to local Better support the 5 CDSG Gagetown; Base, Unit, Supports New Brunswick Association of Community Living primary care providers mental health needs and support services for of children, youth, and Ambulance NB NB Dept. of Environment and Local Government all community members. adults living in OSA. Autumn Years 50+ Club Oromocto Health Centre, Horizon Burton Lions Club Primary Health Care Program, Horizon Enhance public awareness Address the lack of of local programs and Clinic 554 Public Health, Horizon affordable, reliable services that promote transportation Community Residents Royal Canadian Legion Branch 93 Oromocto and support health and services in OSA. wellbeing. Fay Tidd Public Library Sexual Assault Nurse Examiner Program, Horizon Fredericton Junction Health Centre, Horizon Transportation, ASD-W Support rural communities Sustainably strengthen Gagetown & Area Health Services Association Inc. Town of Oromocto and improve access to current efforts addressing health services, programs, community and household Greater Fredericton Social Innovation United Way of Central New Brunswick and supports in rural areas. food security. Healthy Learners Program, ASD-W Village of Fredericton Junction Local Businesses Village of Tracy Better support families Improve communication Midwifery Program, Horizon Wellness Branch, Social Development who are struggling with and collaboration between day-to-day demands and local and regional services expectations. -
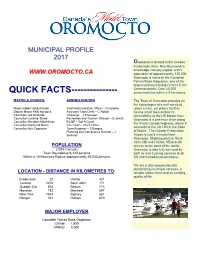
QUICK FACTS------Consumers Live Within a 9 Km Radius
. MUNICIPAL PROFILE 2017 Oromocto is located in the Greater Fredericton Area, New Brunswick’s knowledge industry capital, with a WWW.OROMOCTO.CA population of approximately 125,000. Oromocto is home to the Canadian Forces Base Gagetown, one of the largest military training centres in the Commonwealth. Over 25,000 QUICK FACTS--------------- consumers live within a 9 km radius. MAYOR & COUNCIL ADMINISTRATION The Town of Oromocto provides all the advantages of a well-serviced Mayor Robert (Bob) Powell Chief Administrative Officer – D Isabelle urban centre, yet prides itself on Deputy Mayor Kelly Murdock Assistant Town Clerk – C Abbott having small town ambiance. Councillor Jeff Kirkbride Treasurer – J Thomson Accessibility to the US border from Councillor Lorraine Dawe Recreation and Tourism Director – B Jarratt Oromocto is a one-hour drive along Councillor Sheridan Mawhinney RCMP – Sgt A Duval the Trans Canada Highway, where it Councillor Raymond Henry Fire Chief – Chief J Price Councillor Alex Zaporzan Town Engineer – S Basque connects to the US I-95 in the State Planning and Compliance Director – J of Maine. The Greater Fredericton Jackson Airport is just 5 minutes from Oromocto. Shipping ports in Saint John, NB and Halifax, NS provide POPULATION access to the ports of the world. (2016 Census) Oromocto is also fully serviced by Town Boundaries 9,223 persons both air and trucking services to all Within a 10 Kilometre Radius approximately 25,000 persons US and Canadian destinations. We are a vital community with outstanding municipal services, -

René Morin DND DEPENDANTS' SCHOOLS 1921-1983
René Morin DND DEPENDANTS’ SCHOOLS 1921-1983 Die Dorfschule, by Albert Anker, a Swiss who won interna- tional acclaim for his paintings of rustic scenes. (1896) Kunstmuseum Basel René Morin DND DEPENDANTS’ SCHOOLS 1921-1983 Ottawa Directorate of History National Defence Headquarters 1986 RENÉ MORIN, CD COLONEL (RETIRED) CANADIAN FORCES Note In the writing of this paper the author has been given full access to the relevant files and documents under the di- rection of NDHO/NDRMS and those in the custody of the Direc- tor of History. Old DND files and loose documents now with the Public Archives were also reviewed and pertinent informa- tion extracted for this study. Maps drawn by William R. Constable (iv) TABLE OF CONTENTS List of Annexes......................................... vi List of Tables.......................................... vii List of Abbreviations................................... viii Acknowledgements........................................ x Foreword................................................ xi Preface................................................. xv I Historical Background................................... 1 II The Establishment of DND Dependants' Schools in Canada.. 15 III Federal-Provincial Relations............................ 23 IV DND Dependants' Schools in Europe....................... 35 V The religious issue..................................... 45 VI The language issue...................................... 55 VII Education Allowance (Canada)............................ 73 VIII Language of Instruction: -

1 Atlantic Immigration Pilot Designated Employer List: The
Atlantic Immigration Pilot Designated Employer List: The following is a list of employers designated in New Brunswick through the Atlantic Immigration Pilot. This list does not indicate that these employers are hiring. To find current job vacancies got to www.nbjobs.ca. Liste des employeurs désignés Voici la liste des employeurs désignés sous le Projet pilote en matière d’immigration au Canada atlantique. Cette liste ne signifie pas que ces employeurs recrutent présentement.ss Pour les offres d’emploi, visitez le www.emploisnb.ca. Employer Name 3D Property Management 670807 NB Inc (Dépaneur Needs Caraquet & Shippagan) 693666 NB Inc. A & J Hanna Construction Ltd (Fredericton) A&W Miramichi (630883 NB Inc) A.C. Sharkey's Pub & Grill (Florenceville-Bristol) A.N.D. Communications A.R.Rietzel Landscaping Ltd Acadia Pizza Donair / Korean Restaurant (Dieppe) Acadia Veterinary Hospital Accor Hotels Global Reservation Centre Acorn Restaurant / Mads Truckstop (Lake George) Admiral's Quay B&B (Yang Developments Ltd.) Adorable Chocolat Inc Adrice Cormier Ltd Agence Résidentielle Restigouche Airport General Store (649459 NB Ltd) Airport Inn AirVM Albert's Draperies Alexandru & Camelia Trucking All Needs Special Care Inc. Allen, Paquet & Arseneau Allen's Petro Canada & Grocery (Allen's Enterprise Inc.) AL-Pack Amsterdam Inn & Suites Sussex (deWinter Brothers Ltd.) Andrei Chartovich 1 Employer Name Andrei Master Tailors Ltd Apex Industries Inc Appcast Armour Transport Inc Arom Chinese Cuisine Fredericton (655749 N.B. Ltd.) Asian Garden Indian Restaurant Moncton (Bhatia Brothers Ltd) Aspen University Association Multiculturelle du Restigouche Assurion Canada Inc Asurion Atelier Gérard Beaulieu Atlantic Ballet of Canada Atlantic Controls (Division of Laurentide Controls) Atlantic Home Improvement (656637 NB Inc) Atlantic Lottery Corporation Atlantic Pacific Transport Ltd.