Public Health Reviews HIV/AIDS and Blindness
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Necrotising Retinopathies Simulating Acute Retinal Necrosis Syndrome B Balansard, B Bodaghi, N Cassoux, C Fardeau, S Romand, F Rozenberg, N a Rao, P Lehoang
96 Br J Ophthalmol: first published as 10.1136/bjo.2004.042226 on 21 December 2004. Downloaded from EXTENDED REPORT Necrotising retinopathies simulating acute retinal necrosis syndrome B Balansard, B Bodaghi, N Cassoux, C Fardeau, S Romand, F Rozenberg, N A Rao, P LeHoang ............................................................................................................................... Br J Ophthalmol 2005;89:96–101. doi: 10.1136/bjo.2004.042226 Aim: To determine an aetiological diagnosis in patients presenting with necrotising retinopathies that simulate acute retinal necrosis (ARN). Methods: Retrospective non-comparative case series. The charts of 16 patients presenting with a clinical impression of ARN at Pitie´-Salpeˆtrie`re Hospital, Paris, France, between 1994 and 1999, who required initial antiviral therapy were reviewed. All of the patients had extensive laboratory tests. Anterior chamber paracentesis was performed on 14 patients and evaluated by polymerase chain reaction (PCR) and/or the See end of article for Witmer-Goldmann coefficient to determine the cause of retinitis. Three of the 14 cases also had diagnostic authors’ affiliations vitrectomy. Responses to specific treatment, initiated based on laboratory results, and the final outcome ....................... were evaluated. Correspondence to: Results: Seven of the 16 patients were female and nine were male. The retinitis was bilateral in five patients P LeHoang, and unilateral in 11 patients. The average age of the patients at presentation was 53.6 years. 13 patients MD, PhD, Department of were immune deficient for various reasons. Upon initial presentation, the patients’ visual acuities were less Ophthalmology, Pitie´- than 20/200 in 68% of the affected eyes. The final diagnoses, based on laboratory data and therapeutic Salpeˆtrie`re Hospital, 43 bd de l’Hoˆpital, Paris, France; response were toxoplasmic retinochoroiditis (62.5%), syphilitic retinitis (12.5%), aspergillus endophthal- bahram.bodaghi@ mitis (12.5%), Behc¸et’s disease (6.2%), and intraocular lymphoma (6.2%). -

Cytomegalovirus Retinitis: a Manifestation of the Acquired Immune Deficiency Syndrome (AIDS)*
Br J Ophthalmol: first published as 10.1136/bjo.67.6.372 on 1 June 1983. Downloaded from British Journal ofOphthalmology, 1983, 67, 372-380 Cytomegalovirus retinitis: a manifestation of the acquired immune deficiency syndrome (AIDS)* ALAN H. FRIEDMAN,' JUAN ORELLANA,'2 WILLIAM R. FREEMAN,3 MAURICE H. LUNTZ,2 MICHAEL B. STARR,3 MICHAEL L. TAPPER,4 ILYA SPIGLAND,s HEIDRUN ROTTERDAM,' RICARDO MESA TEJADA,8 SUSAN BRAUNHUT,8 DONNA MILDVAN,6 AND USHA MATHUR6 From the 2Departments ofOphthalmology and 6Medicine (Infectious Disease), Beth Israel Medical Center; 3Ophthalmology, "Medicine (Infectious Disease), and 'Pathology, Lenox Hill Hospital; 'Ophthalmology, Mount Sinai School ofMedicine; 'Division of Virology, Montefiore Hospital and Medical Center; and the 8Institute for Cancer Research, Columbia University College ofPhysicians and Surgeons, New York, USA SUMMARY Two homosexual males with the 'gay bowel syndrome' experienced an acute unilateral loss of vision. Both patients had white intraretinal lesions, which became confluent. One of the cases had a depressed cell-mediated immunity; both patients ultimately died after a prolonged illness. In one patient cytomegalovirus was cultured from a vitreous biopsy. Autopsy revealed disseminated cytomegalovirus in both patients. Widespread retinal necrosis was evident, with typical nuclear and cytoplasmic inclusions of cytomegalovirus. Electron microscopy showed herpes virus, while immunoperoxidase techniques showed cytomegalovirus. The altered cell-mediated response present in homosexual patients may be responsible for the clinical syndromes of Kaposi's sarcoma and opportunistic infection by Pneumocystis carinii, herpes simplex, or cytomegalovirus. http://bjo.bmj.com/ Retinal involvement in adult cytomegalic inclusion manifestations of the syndrome include the 'gay disease (CID) is usually associated with the con- bowel syndrome9 and Kaposi's sarcoma. -

Acute Retinal Necrosis Following Dexamethasone Intravitreal Implant (Ozurdex®) Administration in an Immunocompetent Adult With
Zhang et al. BMC Ophthalmology (2020) 20:247 https://doi.org/10.1186/s12886-020-01514-w CASE REPORT Open Access Acute retinal necrosis following dexamethasone intravitreal implant (Ozurdex®) administration in an immunocompetent adult with a history of HSV encephalitis: a case report Zhi-Yong Zhang1,2* , Xiu-Yun Liu1,2 and Tao Jiang1,2 Abstract Background: Dexamethasone intravitreal implants (0.7 mg) (Ozurdex®, Allergan Inc., Madison, NJ) are FDA approved for managing macular oedema (ME) of retinal vein occlusion (RVO). The major complications associated with intravitreal Ozurdex® implant include increased intraocular pressure and cataract progression. In regard to the occurrence of retinal complications, we report an unusual intravitreal Ozurdex® implantation-related acute retinal necrosis (ARN). Case presentation: A 45-year-old immunocompetent woman with a history of encephalitis presented with photophobia, redness, floaters, and rapidly decreased vision in her left eye. Three and six months ago, she received two doses of intravitreal Ozurdex® implant for ME of RVO. Clinical evaluation, including slit-lamp biomicroscopy, retinal photography, and fluorescein angiography, revealed anterior chamber cells, granulomatous keratic precipitates, cells in the vitreous, optic disc oedema, occlusive retinal vasculitis, scattered retinal haemorrhages, one quadrant of peripheral white areas with retinal necrosis, optic disc and vessels fluorescein staining, and retinal nonperfusion zones. All the above clinical manifestations showed an ARN. Herpes simplex virus was detected in the aqueous and vitreous humour by quantitative polymerase chain reaction testing. Intravenous acyclovir 500 mg tid for 7 days followed by oral valcyclovir was immediately performed for ARN. At 4 months, the patient’s condition improved without retinal detachment, and the best-corrected visual acuity remained stable at 0.3. -

Herpetic Viral Retinitis
American Journal of Virology 2 (1): 25-35, 2013 ISSN: 1949-0097 ©2013 Science Publication doi:10.3844/ajvsp.2013.25.35 Published Online 2 (1) 2013 (http://www.thescipub.com/ajv.toc) Herpetic Viral Retinitis Hidetaka Noma Department of Ophthalmology, Yachiyo Medical Center, Tokyo Women’s Medical University, Chiba, Japan Received 2012-05-30, Revised 2012-07-09; Accepted 2013-07-22 ABSTRACT Human Herpes Virus (HHV) is a DNA virus and is the most important viral pathogen causing intraocular inflammation. HHV is classified into types 1-8. Among these types, HHV-1, HHV-2, HHV-3 Varicella Zoster Virus (VZV) and HHV-5 Cytomegalovirus (CMV) are known to cause herpetic viral retinitis, including acute retinal necrosis and CMV retinitis. Herpes viral retinitis can be diagnosed from characteristic ocular findings and viral identification by PCR of the aqueous humor. Recently, therapy has become more effective than in the past. Herpes viral retinitis gradually progresses if appropriate treatment is not provided with regard to the patient’s immune status. Further advances in diagnostic methods and treatment are required in the future. Keywords: Human Herpes Virus (HHV), Varicella Zoster Virus (VZV), Acute Retinal Necrosis, Polymerase Chain Reaction (PCR), CMV Retinitis, Pathogen Causing Intraocular Inflammation 1. INTRODUCTION by Young and Bird (1978). In the 1980s, the etiology of the disease was shown to be infection by HSV and Human Herpes Virus (HHV) is a DNA virus and VSV. Widespread adoption of the Polymerase Chain the most important viral pathogen causing intraocular Reaction (PCR) method from early the 1990 made it inflammation. It is classified into types 1-8, among possible to easily detect the presence of intraocular which HHV-1, HHV-2, HHV-3 (Varicella Zoster viruses, after which many cases of ARN were Virus: VZV) and HHV-5 Cytomegalovirus (CMV) are diagnosed. -
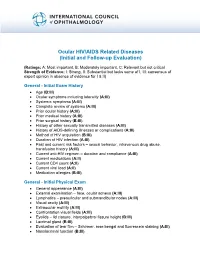
Ocular HIV/AIDS Related Diseases (Initial and Follow-Up Evaluation)
Ocular HIV/AIDS Related Diseases (Initial and Follow-up Evaluation) (Ratings: A: Most important, B: Moderately important, C: Relevant but not critical Strength of Evidence: I: Strong, II: Substantial but lacks some of I, III: consensus of expert opinion in absence of evidence for I & II) General - Initial Exam History Age (B:III) Ocular symptoms including laterality (A:III) Systemic symptoms (A:III) Complete review of systems (A:III) Prior ocular history (A:III) Prior medical history (A:III) Prior surgical history (B:III) History of other sexually transmitted diseases (A:III) History of AIDS-defining illnesses or complications (A:III) Method of HIV acquisition (B:III) Duration of HIV infection (A:III) Past and current risk factors – sexual behavior, intravenous drug abuse, transfusion history (A:III) Current anti-HIV regimen – duration and compliance (A:III) Current medications (A:II) Current CD4 count (A:II) Current viral load (A:II) Medication allergies (B:III) General - Initial Physical Exam General appearance (A:III) External examination – face, ocular adnexa (A:III) Lymphatics – preauricular and submandibular nodes (A:III) Visual acuity (A:III) Extraocular motility (A:III) Confrontation visual fields (A:III) Eyelids – lid closure, interpalpebral fissure height (B:III) Lacrimal gland (B:III) Evaluation of tear film – Schirmer, rose bengal and fluorescein staining (A:III) Nasolacrimal function (B:III) Slit-lamp examination o Eyelid margins (A:III) o Conjunctiva (A:III) o Sclera (A:III) o Cornea (A:III) o -

Advances in the Diagnosis and Management of Acute Retinal Necrosis
8 Review Article Page 1 of 8 Advances in the diagnosis and management of acute retinal necrosis Casey L. Anthony, J. Clay Bavinger, Steven Yeh Department of Ophthalmology, Emory Eye Center, Atlanta, GA, USA Contributions: (I) Conception and design: All authors; (II) Administrative support: S Yeh; (III) Provision of study materials or patients: All authors; (IV) Collection and assembly of data: All authors; (V) Data analysis and interpretation: All authors; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors Correspondence to: Steven Yeh, MD. Department of Ophthalmology, Emory Eye Center, 1365 Clifton Road, Atlanta, GA 30322, USA. Email: [email protected]. Abstract: Acute retinal necrosis (ARN) is a devastating syndrome characterized by panuveitis, retinal necrosis, and a high rate of retinal detachment that may result in poor visual outcomes if not promptly diagnosed and treated. ARN is most commonly caused by viruses within the herpesvirus family. Etiologies include varicella-zoster virus, herpes simplex virus, and cytomegalovirus, and may be promptly diagnosed by polymerase chain reaction testing of aqueous or vitreous fluid. The true incidence of ARN is not known due to its rarity; as a result, clinical treatment is often guided by retrospective case series, case reports, and expert opinion. Standard of care has evolved over time but currently includes a combination of systemic and intravitreal antiviral in conjunction with topical or oral steroids and surgical therapy as needed. Combination therapy may reduce the rate of severe vision loss and increase the rate of visual acuity gain, although further studies are needed in this area. In particular for patients with mild to moderate disease, combination therapy may reduce the rate of retinal detachment. -

Emerging Concepts in the Management of Acute Retinal Necrosis
Downloaded from http://bjo.bmj.com/ on January 3, 2016 - Published by group.bmj.com Review Emerging concepts in the management of acute retinal necrosis Robert William Wong,1,2 J Michael Jumper,2 H Richard McDonald,2 Robert N Johnson,2 Arthur Fu,2 Brandon J Lujan,2,3 Emmett T Cunningham, Jr2,4 ▸ Additional files are ABSTRACT now exists on the characteristics, causes and treat- published online only. To view Acute retinal necrosis (ARN), also known as Kirisawa- ment of this condition. these files please visit the journal online (http://dx.doi. type uveitis, is an uncommon condition caused by org/10.1136/bjophthalmol- infection of the retina by one of the herpes family of CLINICAL SIGNS AND SYMPTOMS 2012-301983). viruses, most typically varicella zoster virus or herpes Acutely, ARN may present with eye redness, periorbi- 1Austin Retina Associates, simplex virus and less commonly cytomegalovirus. tal pain, photophobia and/or vision loss. On anterior Austin, Texas, USA Clinical diagnosis can be challenging and is often aided segment examination, patients may show episcleritis, 2The Department of by PCR-based analysis of ocular fluids. Treatment scleritis, keratitis and/or anterior chamber inflamma- Ophthalmology, California typically involves extended use of one or more antiviral tion, which may be either non-granulomatous or Pacific Medical Center, fi San Francisco, California, USA agents. Long term retinal detachment risk is high. We granulomatous ( gure 2). Examination of the poster- 3Department of Vision Science, review the literature on ARN and present an approach to ior segment may reveal vitreous inflammation, arter- School of Optometry, University the diagnosis and management of this serious condition. -

Treatment of Acute Retinal Necrosis
Treatment of Acute Retinal Necrosis Michael D. Tibbetts, MD,1 Chirag P. Shah, MD, MPH,2 Lucy H. Young, MD, PhD,3 Jay S. Duker, MD,4 Joseph I. Maguire, MD,2 Michael G. Morley, MD5 Objectives: To compare outcomes from patients with acute retinal necrosis (ARN) treated in the acyclovir- only era with those treated in the era of newer antiviral therapies, identify variables affecting outcomes in ARN, and evaluate strategies for fellow eye prophylaxis. Design: Multicenter, nonrandomized, retrospective, interventional series. Participants: A cohort of 58 patients diagnosed with ARN by a retina specialist at 1 of 4 referral centers between 1981 and 2008. The cohort was divided into 2 subgroups: patients treated during the acyclovir-only era (n ϭ 36) and patients treated during the current era of newer antiviral medications (n ϭ 22). Intervention: Intravenous, oral, or intravitreal antiviral medications, including acyclovir, valacyclovir, famci- clovir, valganciclovir, ganciclovir, and foscarnet; prophylactic laser retinopexy; aspirin; oral steroids. Main Outcome Measures: Visual acuity, retinal detachment, and fellow eye involvement. Results: A wide range and combination of antiviral agents are currently used for initial and long-term treatment of ARN. Outcomes from the newer antivirals era were similar to those achieved during the acyclovir- only era. In both groups, the incidence of 20/200 or worse visual acuity was 24% per person-year (P ϭ 0.91). The prevalence of retinal detachment was approximately 50% in each group (P ϭ 0.59). No variables, including prophylactic laser retinopexy, were associated with risk of retinal detachment. Two patients (3.4%) developed ARN in the initially unaffected eye. -

Acute Retinal Necrosis
1452 SCIENTIFIC REPORT Br J Ophthalmol: first published as 10.1136/bjo.2007.114884 on 15 May 2007. Downloaded from Acute retinal necrosis: a national population-based study to assess the incidence, methods of diagnosis, treatment strategies and outcomes in the UK This paper is freely available online under the BMJ Journals unlocked scheme, M N Muthiah, M Michaelides, C S Child, S M Mitchell see http://bjo.bmj.com/info/unlocked.dtl ................................................................................................................................... Br J Ophthalmol 2007;91:1452–1455. doi: 10.1136/bjo.2007.114884 causative viral DNA with laboratory testing of aqueous or Aim: To determine the incidence, methods of diagnosis, vitreous samples.12 Most reported cases have been caused by treatment strategies and outcomes for acute retinal necrosis varicella zoster virus (VZV), accounting for 50% to 80% of cases, (ARN) in the UK. with herpes simplex virus (HSV) responsible for the remaining Methods: A 12-month active case ascertainment study was cases when an organism has been isolated.24–6 carried out between March 2001 and March 2002 to record The incidence of ARN in the UK is unknown. It is possible cases of ARN presenting to ophthalmologists via the British that the incidence of ARN may be rising since both the number Ophthalmological Surveillance Unit (BOSU) reporting system. of immunosuppressed patients and the average age of the Questionnaires were sent to the reporting consultants, request- population in the UK are increasing.7 Prompt diagnosis and ing data on patient characteristics, presentation, clinical treatment is critical in attempting to reduce visual loss in this findings, investigations and treatment. -

November 2000
Vol.XVIII No. 3 NOVEMBER 2000 Scientific Journal of MEDICAL & VISION RESEARCH FOUNDATIONS 18, COLLEGE ROAD, CHENNAI - 600 006, INDIA Presurgical photograph taken at 28 days of life Age 13 months after skin grafting,showing no showing complete left cryptophthalmos. adhesions and good cosmetic outcome. Editorial Perspective — Treatment of Malignant Melanoma of Choroid — Mahesh P Shanmugam Prepucial Skin Graft for Fornicial and Socket Reconstruction in Complete Cryptophthalmos with Congenital Cystic Eye - A Case Report — Nirmala Subramanian, Surbhit Choudhry and Lakshmi Mahesh Detection of Cytomegalovirus (CMV) from Ocular Fluid of Two Patients with Progressive Outer Retinal Necrosis (PORN) — Jyotirmay Biswas, Surbhit Choudhry, K Priya and Lingam Gopal Unilateral Neuroretinitis following Chicken Pox - Report of a Case — Sumeet Chopra, Jyotirmay Biswas, Sudha K Ganesh and Satya Karna Human Genome Project: A Medical Revolution — G Kumaramanickavel Yeast - a Valuable tool for differential diagnosis of glycosuria and galactosuira — S. Ramakrishnan, K.N. Sulochana, R. Punitham and S.B. Vasanthi Last Page — Literature search on the Internet — Rajesh Fogla Editorial The event of this year, some dub it as that of the century _ the unraveling of the Human Genome finds a mention in this issue of Insight also. Dr. Kumaramanickavel has lucidly written about the implications of this discovery to Medicine and in particular Ophthalmology. Scientists especially the Genetic scientists predict the end of the scalpel and the pill. He has also introduced a new term _ Predictive Medicine. The concept is interesting _ predict the onset of the disease and annul it before it occurs. No doubt the darker side of this technology is foreboding to think of,but as Dr. -

Acute Retinal Necrosis After Intravitreal Triamcinolone Acetonide for Aphakic Macular Edema- a Case Report
Asian Pac. J. Health Sci., 2017; 4(1):44-47 e-ISSN: 2349-0659, p-ISSN: 2350-0964 ____________________________________________________________________________________________________________________________________________ Document heading doi: 10.21276/apjhs.2017.4.1.9 Case Report Acute Retinal Necrosis After Intravitreal Triamcinolone Acetonide For Aphakic Macular Edema- A Case Report Aliya Sulatana Assistant Professor, Sarojini Devi Eye Hospital, Hyderabad, Telangana State, India ABSTRACT Triamcinolone acetonide is used in the form of intravitreal injection to treat ocular diseases like uveitis, vasculitis, proliferative vitreoretinopathy, macular degeneration etc. But complications have been reported after injection like elevated intraocular pressure and cataract. Even though rare, acute retinal necrosis is a risky complication after intraocular Triamcinolone acetonide injection, which may cause potential blindness. Here we report a case of acute retinal necrosis following intravitreal injection of Triamcinolone acetonide and review the relevant literature. Keywords: Acute retinal necrosis, Intraocular injection, Triamcinolone acetonide. Introduction Triamcinolone Acetonide (TA), a water-insoluble whole intraocular steroids will cause localised corticosteroid is widely used in the field of immunosuppression. In immunocompromised patients, ophthalmology. It can be injected either under tenon’s necrotizing retinitis may be usually caused by varicella capsule, into the retrobulbar space or directly into the zoster virus (VZV) or herpes -

Cytomegalovirus Retinitis Without Immunocompromise
MEDICAL RETINA s CYTOMEGALOVIRUS RETINITIS WITHOUT IMMUNOCOMPROMISE What could have predisposed this immunocompetent patient to this complication with extensive retinal ischemia? BY MICHAEL C. IZZO, MD; MARIAM MATHAI, MD; AND BRIAN K. DO, MD ytomegalovirus (CMV) retinitis, caused by a CASE PRESENTATION double-stranded DNA virus in the herpesviridae fam- A 71-year-old Black man with a medical history including ily, is the most common opportunistic ocular infec- coronary artery disease, prostate cancer (treated by prosta- tion in patients with advanced AIDS.1 CMV retinitis tectomy without chemotherapy or radiation), and quiescent can occur in the absence of HIV infection, although sarcoidosis (off all treatment for 40 years) presented to a Cthis is uncommon. The retinitis in these cases is typically retina specialist for evaluation of decreased vision in the right associated with relative immunosuppression with systemic eye for 3 weeks. The patient’s ocular history was significant corticosteroids, noncorticosteroid immunosuppressive for cataract surgery with multifocal IOL implantation in both agents, or chemotherapeutics.2 CMV retinitis, in the absence eyes and open-angle glaucoma treated with dorzolamide- of any systemic or local ocular immunosuppression, is timolol (2%/0.5%) and latanoprost (0.005%). He did not have extremely rare.3-5 a history of ocular sarcoid. Here, we present a case of CMV retinitis in a fully immu- BCVA at presentation was counting fingers at 2 feet OD nocompetent patient with significant widespread retinal and 20/25 OS. IOP was 16 mm Hg in each eye, and a mild ischemia in the affected eye. afferent pupillary defect was noted in the right eye.