Wakix, INN-Pitolisant
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pharmacy Policy Statement
PHARMACY POLICY STATEMENT Georgia Medicaid DRUG NAME Wakix (pitolisant) BILLING CODE Must use valid NDC BENEFIT TYPE Pharmacy SITE OF SERVICE ALLOWED Home COVERAGE REQUIREMENTS Prior Authorization Required (Non-Preferred Product) QUANTITY LIMIT— 60 tablets per 30 days LIST OF DIAGNOSES CONSIDERED NOT Click Here MEDICALLY NECESSARY Wakix (pitolisant) is a non-preferred product and will only be considered for coverage under the pharmacy benefit when the following criteria are met: Members must be clinically diagnosed with one of the following disease states and meet their individual criteria as stated. NARCOLEPSY WITH EXCESSIVE DAYTIME SLEEPINESS (EDS) For initial authorization: 1. Member is 18 years old or older; AND 2. Medication must be prescribed by or in consultation with a neurologist or sleep specialist; AND 3. Member has a diagnosis of narcolepsy confirmed by sleep studies: polysomnogram and MSLT (multiple sleep latency test); AND 4. Member has symptoms of excessive sleepiness not attributed to other factors such as insufficient sleep, irregular sleep schedule, co-existent sleep disorder, medications or other substances; AND 5. Member’s current score on the Epworth sleepiness scale (ESS) is documented in chart notes; AND 6. Member has tried and failed or did not tolerate the following, at max tolerated dose, for at least 30 days each: modafinil or armodafinil, AND Sunosi; AND 7. Member does not have ANY of the following: a) Severe hepatic impairment; b) End stage renal disease; c) QT interval prolongation or cardiac arrythmia. 8. Dosage allowed: Up to 2 tablets per day; max daily dose of 35.6mg (Two 17.8mg tablets once daily). -

Réglementation De La Pharmacie
R E C U E I L D E T E X T E S S U R L A P H A R M A C I E Mis à jour le 13 février 2017 par l’Inspection de la pharmacie P R É A M B U L E La réglementation relative à la pharmacie en vigueur en Nouvelle-Calédonie résulte de la coexistence des dispositions adoptées par la Nouvelle-Calédonie au titre de ses compétences en matières d’hygiène publique, de santé et de professions de la pharmacie1, et de celles adoptées par l’Etat au titre de ses compétences en matières de garanties des libertés publiques, de droit civil et de droit commercial2. Sur le contenu du recueil En 1954, la Nouvelle-Calédonie s’est vue étendre les articles L. 511 à L. 520 et L. 549 à L. 665 de l’ancien Livre V relatif à la Pharmacie du code de la santé publique métropolitain par la loi n° 54-418 du 15 avril 1954 étendant aux territoires d'outre-mer, au Togo et au Cameroun certaines dispositions du Code de la santé publique relatives à l'exercice de la pharmacie3, dont les modalités d’application ont été fixées par le décret modifié n° 55-1122 du 16 août 1955 fixant les modalités d'application de la loi n° 54-418 du 15 avril 1954 étendant aux territoires d'outre-mer, au Togo et au Cameroun certaines dispositions du code de la santé publique relatives à l'exercice de la pharmacie4. Depuis sont intervenues la loi- cadre Defferre5, la loi référendaire de 19886 et la loi organique n° 99-209 du 19 mars 1999 dont les apports ont eu pour résultat le transfert de ces articles de la compétence de l’Etat à la compétence de la Nouvelle-Calédonie, permettant à celle-ci de s’en approprier et de les modifier à sa guise par des délibérations du congrès de la Nouvelle-Calédonie7. -

Phencyclidine (PCP) Abuse: an Appraisal
PHENCYCLIDINE Latest Revision: May 16, 2005 1. SYNONYMS CFR: Phencyclidine CAS #: Base: 77-10-1 Hydrochloride: 956-90-1 Other Names: 1-(1-Phenylcyclohexyl) piperidine PCP Angel dust CI-395 Sernylan Sernyl 2. CHEMICAL AND PHYSICAL DATA 2.1. CHEMICAL DATA Form Chemical Formula Molecular Weight Melting Point (°C) Base C17H25N 243.4 46-46.5 Hydrochloride C17H26NCl 279.9 233-235 2.2. SOLUBILITY Form A C E H M W Base FS FS FS FS S VSS Hydrochloride SS FS I I FS FS A = acetone, C = chloroform, E = ether, H = hexane, M = methanol and W = water, VS = very soluble, FS = freely soluble, S = soluble, PS = sparingly soluble, SS = slightly soluble, VSS = very slightly soluble and I = insoluble 3. SCREENING TECHNIQUES 3.1. COLOR TESTS REAGENT COLOR PRODUCED p-Dimethylaminobenzaldehyde Red 3.2. CRYSTAL TESTS REAGENT CRYSTALS FORMED Potassium permanganate Bow-tie shaped 3.3. THIN-LAYER CHROMATOGRAPHY Visualization Acidified iodoplatinate spray Dragendorff spray COMPOUND RELATIVE R1 System System System TLC17 TLC11 TLC16 piperidine 0.4 0.2 0.1 PCP 1.0 1.0 1.0 piperidinocyclohexylcarbonitrile (PCC) 4.5 1.7 1.7 Both iodoplatinate and Dragendorff sprays will detect the three components. Iodine vapor produces a white spot outlined in brown for PCC, where as PCP and piperidine both give brown spots. 3.4. GAS CHROMATOGRAPHY Method PCP-GCS1 Instrument: Gas chromatograph operated in split mode with FID Column: 5% phenyl/95% methyl silicone 12 m x 0.2 mm x 0.33 µm film thickness Carrier gas: Helium at 1.0 mL/min Temperatures: Injector: 270°C Detector: 280°C Oven program: 1) 175°C initial temperature for 1.0 min 2) Ramp to 275°C at 15°C/min 3) Hold final temperature for 3.0 min Injection Parameters: Split Ratio = 60:1, 1 µL injected Samples are to be dissolved or diluted in chloroform and filtered. -

CAS Number Index
2334 CAS Number Index CAS # Page Name CAS # Page Name CAS # Page Name 50-00-0 905 Formaldehyde 56-81-5 967 Glycerol 61-90-5 1135 Leucine 50-02-2 596 Dexamethasone 56-85-9 963 Glutamine 62-44-2 1640 Phenacetin 50-06-6 1654 Phenobarbital 57-00-1 514 Creatine 62-46-4 1166 α-Lipoic acid 50-11-3 1288 Metharbital 57-22-7 2229 Vincristine 62-53-3 131 Aniline 50-12-4 1245 Mephenytoin 57-24-9 1950 Strychnine 62-73-7 626 Dichlorvos 50-23-7 1017 Hydrocortisone 57-27-2 1428 Morphine 63-05-8 127 Androstenedione 50-24-8 1739 Prednisolone 57-41-0 1672 Phenytoin 63-25-2 335 Carbaryl 50-29-3 569 DDT 57-42-1 1239 Meperidine 63-75-2 142 Arecoline 50-33-9 1666 Phenylbutazone 57-43-2 108 Amobarbital 64-04-0 1648 Phenethylamine 50-34-0 1770 Propantheline bromide 57-44-3 191 Barbital 64-13-1 1308 p-Methoxyamphetamine 50-35-1 2054 Thalidomide 57-47-6 1683 Physostigmine 64-17-5 784 Ethanol 50-36-2 497 Cocaine 57-53-4 1249 Meprobamate 64-18-6 909 Formic acid 50-37-3 1197 Lysergic acid diethylamide 57-55-6 1782 Propylene glycol 64-77-7 2104 Tolbutamide 50-44-2 1253 6-Mercaptopurine 57-66-9 1751 Probenecid 64-86-8 506 Colchicine 50-47-5 589 Desipramine 57-74-9 398 Chlordane 65-23-6 1802 Pyridoxine 50-48-6 103 Amitriptyline 57-92-1 1947 Streptomycin 65-29-2 931 Gallamine 50-49-7 1053 Imipramine 57-94-3 2179 Tubocurarine chloride 65-45-2 1888 Salicylamide 50-52-2 2071 Thioridazine 57-96-5 1966 Sulfinpyrazone 65-49-6 98 p-Aminosalicylic acid 50-53-3 426 Chlorpromazine 58-00-4 138 Apomorphine 66-76-2 632 Dicumarol 50-55-5 1841 Reserpine 58-05-9 1136 Leucovorin 66-79-5 -

APPENDIX G Acid Dissociation Constants
harxxxxx_App-G.qxd 3/8/10 1:34 PM Page AP11 APPENDIX G Acid Dissociation Constants § ϭ 0.1 M 0 ؍ (Ionic strength ( † ‡ † Name Structure* pKa Ka pKa ϫ Ϫ5 Acetic acid CH3CO2H 4.756 1.75 10 4.56 (ethanoic acid) N ϩ H3 ϫ Ϫ3 Alanine CHCH3 2.344 (CO2H) 4.53 10 2.33 ϫ Ϫ10 9.868 (NH3) 1.36 10 9.71 CO2H ϩ Ϫ5 Aminobenzene NH3 4.601 2.51 ϫ 10 4.64 (aniline) ϪO SNϩ Ϫ4 4-Aminobenzenesulfonic acid 3 H3 3.232 5.86 ϫ 10 3.01 (sulfanilic acid) ϩ NH3 ϫ Ϫ3 2-Aminobenzoic acid 2.08 (CO2H) 8.3 10 2.01 ϫ Ϫ5 (anthranilic acid) 4.96 (NH3) 1.10 10 4.78 CO2H ϩ 2-Aminoethanethiol HSCH2CH2NH3 —— 8.21 (SH) (2-mercaptoethylamine) —— 10.73 (NH3) ϩ ϫ Ϫ10 2-Aminoethanol HOCH2CH2NH3 9.498 3.18 10 9.52 (ethanolamine) O H ϫ Ϫ5 4.70 (NH3) (20°) 2.0 10 4.74 2-Aminophenol Ϫ 9.97 (OH) (20°) 1.05 ϫ 10 10 9.87 ϩ NH3 ϩ ϫ Ϫ10 Ammonia NH4 9.245 5.69 10 9.26 N ϩ H3 N ϩ H2 ϫ Ϫ2 1.823 (CO2H) 1.50 10 2.03 CHCH CH CH NHC ϫ Ϫ9 Arginine 2 2 2 8.991 (NH3) 1.02 10 9.00 NH —— (NH2) —— (12.1) CO2H 2 O Ϫ 2.24 5.8 ϫ 10 3 2.15 Ϫ Arsenic acid HO As OH 6.96 1.10 ϫ 10 7 6.65 Ϫ (hydrogen arsenate) (11.50) 3.2 ϫ 10 12 (11.18) OH ϫ Ϫ10 Arsenious acid As(OH)3 9.29 5.1 10 9.14 (hydrogen arsenite) N ϩ O H3 Asparagine CHCH2CNH2 —— —— 2.16 (CO2H) —— —— 8.73 (NH3) CO2H *Each acid is written in its protonated form. -

Neuroenhancement in Healthy Adults, Part I: Pharmaceutical
l Rese ca arc ni h li & C f B o i o l e Journal of a t h n Fond et al., J Clinic Res Bioeth 2015, 6:2 r i c u s o J DOI: 10.4172/2155-9627.1000213 ISSN: 2155-9627 Clinical Research & Bioethics Review Article Open Access Neuroenhancement in Healthy Adults, Part I: Pharmaceutical Cognitive Enhancement: A Systematic Review Fond G1,2*, Micoulaud-Franchi JA3, Macgregor A2, Richieri R3,4, Miot S5,6, Lopez R2, Abbar M7, Lancon C3 and Repantis D8 1Université Paris Est-Créteil, Psychiatry and Addiction Pole University Hospitals Henri Mondor, Inserm U955, Eq 15 Psychiatric Genetics, DHU Pe-psy, FondaMental Foundation, Scientific Cooperation Foundation Mental Health, National Network of Schizophrenia Expert Centers, F-94000, France 2Inserm 1061, University Psychiatry Service, University of Montpellier 1, CHU Montpellier F-34000, France 3POLE Academic Psychiatry, CHU Sainte-Marguerite, F-13274 Marseille, Cedex 09, France 4 Public Health Laboratory, Faculty of Medicine, EA 3279, F-13385 Marseille, Cedex 05, France 5Inserm U1061, Idiopathic Hypersomnia Narcolepsy National Reference Centre, Unit of sleep disorders, University of Montpellier 1, CHU Montpellier F-34000, Paris, France 6Inserm U952, CNRS UMR 7224, Pierre and Marie Curie University, F-75000, Paris, France 7CHU Carémeau, University of Nîmes, Nîmes, F-31000, France 8Department of Psychiatry, Charité-Universitätsmedizin Berlin, Campus Benjamin Franklin, Eschenallee 3, 14050 Berlin, Germany *Corresponding author: Dr. Guillaume Fond, Pole de Psychiatrie, Hôpital A. Chenevier, 40 rue de Mesly, Créteil F-94010, France, Tel: (33)178682372; Fax: (33)178682381; E-mail: [email protected] Received date: January 06, 2015, Accepted date: February 23, 2015, Published date: February 28, 2015 Copyright: © 2015 Fond G, et al. -
![Ehealth DSI [Ehdsi V2.2.2-OR] Ehealth DSI – Master Value Set](https://docslib.b-cdn.net/cover/8870/ehealth-dsi-ehdsi-v2-2-2-or-ehealth-dsi-master-value-set-1028870.webp)
Ehealth DSI [Ehdsi V2.2.2-OR] Ehealth DSI – Master Value Set
MTC eHealth DSI [eHDSI v2.2.2-OR] eHealth DSI – Master Value Set Catalogue Responsible : eHDSI Solution Provider PublishDate : Wed Nov 08 16:16:10 CET 2017 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 1 of 490 MTC Table of Contents epSOSActiveIngredient 4 epSOSAdministrativeGender 148 epSOSAdverseEventType 149 epSOSAllergenNoDrugs 150 epSOSBloodGroup 155 epSOSBloodPressure 156 epSOSCodeNoMedication 157 epSOSCodeProb 158 epSOSConfidentiality 159 epSOSCountry 160 epSOSDisplayLabel 167 epSOSDocumentCode 170 epSOSDoseForm 171 epSOSHealthcareProfessionalRoles 184 epSOSIllnessesandDisorders 186 epSOSLanguage 448 epSOSMedicalDevices 458 epSOSNullFavor 461 epSOSPackage 462 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 2 of 490 MTC epSOSPersonalRelationship 464 epSOSPregnancyInformation 466 epSOSProcedures 467 epSOSReactionAllergy 470 epSOSResolutionOutcome 472 epSOSRoleClass 473 epSOSRouteofAdministration 474 epSOSSections 477 epSOSSeverity 478 epSOSSocialHistory 479 epSOSStatusCode 480 epSOSSubstitutionCode 481 epSOSTelecomAddress 482 epSOSTimingEvent 483 epSOSUnits 484 epSOSUnknownInformation 487 epSOSVaccine 488 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 3 of 490 MTC epSOSActiveIngredient epSOSActiveIngredient Value Set ID 1.3.6.1.4.1.12559.11.10.1.3.1.42.24 TRANSLATIONS Code System ID Code System Version Concept Code Description (FSN) 2.16.840.1.113883.6.73 2017-01 A ALIMENTARY TRACT AND METABOLISM 2.16.840.1.113883.6.73 2017-01 -

Chemicals Required for the Illicit Manufacture of Drugs Table 1 SUBSTANCES in TABLES I and II of the 1988 CONVENTION
Chemicals Required 1. A variety of chemicals are used in the illicit manufacture of for the Illicit drugs. The United Nations Convention against Illicit Traffic in Manufacture of Drugs Narcotic Drugs and Psychotropic Substances of 1988 (1988 Convention) refers to “substances frequently used in the illicit manufacture of narcotic drugs and psychotropic substances”. Twenty-two such substances are listed in Tables I and II of the 1988 Convention as in force on 1st May, 1998. (See Table1) Table 1 Table I Table II SUBSTANCES IN N-Acetylanthranilic acid. Acetic anhydride TABLES I AND II OF Ephedrine Acetone THE 1988 Ergometrine Anthranilic acid CONVENTION Ergotamine Ethyl ether Isosafrole Hydrochloric acid* Lysergic acid Methyl ethyl ketone 3,4-methylenedioxyphenyl-2-propanone Phenylacetic acid 1-phenyl-2-propanone Piperidine Piperonal Potassium permanganate Pseudoephedrine Sulphuric acid* Safrole Toluene The salts of the substances in this Table The salts of the substances whenever the existence of such salts is in this Table whenever the possible. existence of such salts is possible. * The salts of hydrochloric acid and sulphuric acid are specifically excluded from Table II. U N D C P 11 The term “precursor” is used to indicate any of these substances in the two Tables. Chemicals used in the illicit manufacture of narcotic drugs and psychotropic substances are often described as precursors or essential chemicals, and these include true precursors, solvents, oxidising agents and other Chemicals used in the illicit manufacture of narcotic substances. Although the term is not drugs and psychotropic substances are often technically correct, it has become common described as precursors or essential chemicals, and practice to refer to all such substances as these include true precursors, solvents, oxidising “precursors”. -
For Personal Use Only
Antidep ® Dowden Health Media CopyrightFor personal use only Referring to certain groups of drugs as antidepressants does them a great disservice; their potential uses range far beyond mood disorders For mass reproduction, content licensing and permissions contact Dowden Health Media. ressants molecule is a molecule is a molecule—until it The spectrum becomes identified with a purpose. Consider, for example, (-)-trans-4R-(4’-fluorophenyl)-3S- beyond depression A[(3’,4’-methylenedioxyphenoxy) methyl] piperidine. You probably know this molecule as paroxetine—an an- tidepressant, of course, but it is more than that. If you James W. Jefferson, MD examine paroxetine’s FDA-approved indications, it also Distinguished senior scientist has anti-panic, anti-social anxiety, anti-obsessive-com- Madison Institute of Medicine, Inc. pulsive disorder, anti-posttraumatic stress disorder, and Clinical professor of psychiatry University of Wisconsin School of Medicine anti-premenstrual dysphoric disorder effects. and Public Health “Antidepressants” have achieved fame as antidepres- sants; one could say these molecules’ search for meaning has been fulfilled. Yet even within psychiatry, their many other uses (Table, page 36) can create semantic misunder- standings. Beyond psychiatry, consider the nondepressed patient with neurocardiogenic syncope who wonders why he’s being treated with an antidepressant. Rather than calling antidepressants “panaceas,” the better choice is to educate patients about the drugs’ wide spectrum of activity. Let’s look broadly across the so-called antidepressants and examine their varied uses in psychiatry and other medical specialties. Pain syndromes Peripheral neuropathy. The only antidepressant with an FDA-approved pain indication is duloxetine, Current Psychiatry © 2007 MATT MANLEY Vol. -
Safety Data Sheet: Piperidine
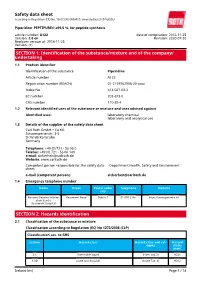
Safety data sheet according to Regulation (EC) No. 1907/2006 (REACH), amended by 2015/830/EU Piperidine PEPTIPURE® ≥99,5 %, for peptide synthesis article number: A122 date of compilation: 2016-11-25 Version: 2.0 en Revision: 2020-07-20 Replaces version of: 2016-11-25 Version: (1) SECTION 1: Identification of the substance/mixture and of the company/ undertaking 1.1 Product identifier Identification of the substance Piperidine Article number A122 Registration number (REACH) 01-2119962908-20-xxxx Index No 613-027-00-3 EC number 203-813-0 CAS number 110-89-4 1.2 Relevant identified uses of the substance or mixture and uses advised against Identified uses: laboratory chemical laboratory and analytical use 1.3 Details of the supplier of the safety data sheet Carl Roth GmbH + Co KG Schoemperlenstr. 3-5 D-76185 Karlsruhe Germany Telephone: +49 (0) 721 - 56 06 0 Telefax: +49 (0) 721 - 56 06 149 e-mail: [email protected] Website: www.carlroth.de Competent person responsible for the safety data : Department Health, Safety and Environment sheet: e-mail (competent person): [email protected] 1.4 Emergency telephone number Name Street Postal code/ Telephone Website city National Poisons Inform- Beaumont Road Dublin 9 01 809 2166 https://www.poisons.ie/ ation Centre Beaumont Hospital SECTION 2: Hazards identification 2.1 Classification of the substance or mixture Classification according to Regulation (EC) No 1272/2008 (CLP) Classification acc. to GHS Section Hazard class Hazard class and cat- Hazard egory state- ment 2.6 flammable liquid (Flam. Liq. 2) H225 3.1O acute toxicity (oral) (Acute Tox. -

Dissociation Constants of Organic Acids and Bases
DISSOCIATION CONSTANTS OF ORGANIC ACIDS AND BASES This table lists the dissociation (ionization) constants of over pKa + pKb = pKwater = 14.00 (at 25°C) 1070 organic acids, bases, and amphoteric compounds. All data apply to dilute aqueous solutions and are presented as values of Compounds are listed by molecular formula in Hill order. pKa, which is defined as the negative of the logarithm of the equi- librium constant K for the reaction a References HA H+ + A- 1. Perrin, D. D., Dissociation Constants of Organic Bases in Aqueous i.e., Solution, Butterworths, London, 1965; Supplement, 1972. 2. Serjeant, E. P., and Dempsey, B., Ionization Constants of Organic Acids + - Ka = [H ][A ]/[HA] in Aqueous Solution, Pergamon, Oxford, 1979. 3. Albert, A., “Ionization Constants of Heterocyclic Substances”, in where [H+], etc. represent the concentrations of the respective Katritzky, A. R., Ed., Physical Methods in Heterocyclic Chemistry, - species in mol/L. It follows that pKa = pH + log[HA] – log[A ], so Academic Press, New York, 1963. 4. Sober, H.A., Ed., CRC Handbook of Biochemistry, CRC Press, Boca that a solution with 50% dissociation has pH equal to the pKa of the acid. Raton, FL, 1968. 5. Perrin, D. D., Dempsey, B., and Serjeant, E. P., pK Prediction for Data for bases are presented as pK values for the conjugate acid, a a Organic Acids and Bases, Chapman and Hall, London, 1981. i.e., for the reaction 6. Albert, A., and Serjeant, E. P., The Determination of Ionization + + Constants, Third Edition, Chapman and Hall, London, 1984. BH H + B 7. Budavari, S., Ed., The Merck Index, Twelth Edition, Merck & Co., Whitehouse Station, NJ, 1996. -

Lääkealan Turvallisuus- Ja Kehittämiskeskuksen Päätös
Lääkealan turvallisuus- ja kehittämiskeskuksen päätös N:o xxxx lääkeluettelosta Annettu Helsingissä xx päivänä maaliskuuta 2016 ————— Lääkealan turvallisuus- ja kehittämiskeskus on 10 päivänä huhtikuuta 1987 annetun lääke- lain (395/1987) 83 §:n nojalla päättänyt vahvistaa seuraavan lääkeluettelon: 1 § Lääkeaineet ovat valmisteessa suolamuodossa Luettelon tarkoitus teknisen käsiteltävyyden vuoksi. Lääkeaine ja sen suolamuoto ovat biologisesti samanarvoisia. Tämä päätös sisältää luettelon Suomessa lääk- Liitteen 1 A aineet ovat lääkeaineanalogeja ja keellisessä käytössä olevista aineista ja rohdoksis- prohormoneja. Kaikki liitteen 1 A aineet rinnaste- ta. Lääkeluettelo laaditaan ottaen huomioon lää- taan aina vaikutuksen perusteella ainoastaan lää- kelain 3 ja 5 §:n säännökset. kemääräyksellä toimitettaviin lääkkeisiin. Lääkkeellä tarkoitetaan valmistetta tai ainetta, jonka tarkoituksena on sisäisesti tai ulkoisesti 2 § käytettynä parantaa, lievittää tai ehkäistä sairautta Lääkkeitä ovat tai sen oireita ihmisessä tai eläimessä. Lääkkeeksi 1) tämän päätöksen liitteessä 1 luetellut aineet, katsotaan myös sisäisesti tai ulkoisesti käytettävä niiden suolat ja esterit; aine tai aineiden yhdistelmä, jota voidaan käyttää 2) rikoslain 44 luvun 16 §:n 1 momentissa tar- ihmisen tai eläimen elintoimintojen palauttami- koitetuista dopingaineista annetussa valtioneuvos- seksi, korjaamiseksi tai muuttamiseksi farmako- ton asetuksessa kulloinkin luetellut dopingaineet; logisen, immunologisen tai metabolisen vaikutuk- ja sen avulla taikka terveydentilan