University of Florida Thesis Or Dissertation Formatting
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Dissertation Entitled Mechanically-Conditioned Biphasic
A Dissertation entitled Mechanically-Conditioned Biphasic Composite Scaffolds to Augment Healing of Tendon-Bone Interface by Gayathri Subramanian Submitted to the Graduate Faculty as partial fulfillment of the requirements for the Doctor of Philosophy Degree in Biomedical Engineering ________________________________________ Dr. Eda Yildirim-Ayan, Committee Chair ________________________________________ Dr. Beata Lecka-Czernik, Committee Member ________________________________________ Dr. Yakov Lapitsky, Committee Member ________________________________________ Dr. Ronald Fournier, Committee Member ________________________________________ Dr. Arunan Nadarajah, Committee Member ________________________________________ Dr. Amanda Bryant-Friedrich, Dean College of Graduate Studies The University of Toledo August 2017 Copyright 2017, Gayathri Subramanian This document is copyrighted material. Under copyright law, no parts of this document may be reproduced without the expressed permission of the author. An Abstract of Mechanically-Conditioned Biphasic Composite Scaffolds to Augment Healing of Tendon-Bone Interface by Gayathri Subramanian Submitted to the Graduate Faculty as partial fulfillment of the requirements for the Doctor of Philosophy Degree in Biomedical Engineering The University of Toledo August 2017 Rotator cuff injuries are very common among people over the age of 60, with more than 600,000 surgeries performed annually in the United States for rotator cuff repairs. However, in 20-80% of the cases, the repair fails due to re-rupture -

Surnames 198
Surnames 198 P PACQUIN PAGONE PALCISCO PACUCH PAHACH PALEK PAAHANA PACY PAHEL PALENIK PAAR PADASAK PAHUSZKI PALERMO PAASSARELLI PADDOCK PAHUTSKY PALESCH PABALAN PADELL PAINE PALGUTA PABLIK PADGETT PAINTER PALI PABRAZINSKY PADLO PAIRSON PALILLA PABST PADUNCIC PAISELL PALINA PACCONI PAESANI PAJAK PALINO PACE PAESANO PAJEWSKI PALINSKI PACEK PAFFRATH PAKALA PALKO PACELLI PAGANI PAKOS PALL PACEY PAGANO PALACE PALLO PACHARKA PAGDEN PALADINO PALLONE PACIFIC PAGE PALAGGO PALLOSKY PACILLA PAGLARINI PALAIC PALLOTTINI PACINI PAGLIARINI PALANIK PALLOZZI PACK PAGLIARNI PALANKEY PALM PACKARD PAGLIARO PALANKI PALMA PACKER PAGLIARULO PALAZZONE PALMER PACNUCCI PAGLIASOTTI PALCHESKO PALMERO PACOLT PAGO PALCIC PALMERRI Historical & Genealogical Society of Indiana County 1/21/2013 Surnames 199 PALMIERI PANCIERRA PAOLO PARDUS PALMISANO PANCOAST PAONE PARE PALMISCIANO PANCZAK PAPAKIE PARENTE PALMISCNO PANDAL PAPCIAK PARENTI PALMO PANDULLO PAPE PARETTI PALOMBO PANE PAPIK PARETTO PALONE PANGALLO PAPOVICH PARFITT PALSGROVE PANGBURN PAPPAL PARHAM PALUCH PANGONIS PAPSON PARILLO PALUCHAK PANIALE PAPUGA PARIS PALUDA PANKOVICH PAPURELLO PARISE PALUGA PANKRATZ PARADA PARISEY PALUGNACK PANNACHIA PARANA PARISH PALUMBO PANNEBAKER PARANIC PARISI PALUS PANONE PARAPOT PARISO PALUSKA PANOSKY PARATTO PARIZACK PALYA PANTALL PARCELL PARK PAMPE PANTALONE PARCHINSKY PARKE PANAIA PANTANI PARCHUKE PARKER PANASCI PANTANO PARDEE PARKES PANASKI PANTZER PARDINI PARKHILL PANCHICK PANZY PARDO PARKHURST PANCHIK PAOLINELLIE PARDOE PARKIN Historical & Genealogical Society of Indiana County -
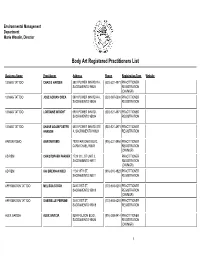
Crystal Reports
Environmental Management Department Marie Woodin, Director Body Art Registered Practitioners List Business Name Practitioner Address Phone Registration Type Website 13 MAG TATTOO CHAD E HAYDEN 5801 POWER INN RD # A, (530) 521-4971 PRACTITIONER No Website SACRAMENTO 95824 REGISTRATION (OW/MGR) 13 MAG TATTOO JOSE ADRIAN OREA 5801 POWER INN RD # A, (530) 987-5394 PRACTITIONER No Website SACRAMENTO 95824 REGISTRATION 13 MAG TATTOO LORRAINE WRIGHT 5801 POWER INN RD, (530) 521-4971 PRACTITIONER No Website SACRAMENTO 95824 REGISTRATION 13 MAG TATTOO SHANE ADAM FOSTER 5801 POWER INN RD STE (530) 521-4971 PRACTITIONER No Website HANSON A, SACRAMENTO 95824 REGISTRATION AARON ROMO AARON ROMO 7820 FAIR OAKS BLVD, (916) 331-5954 PRACTITIONER No Website CARMICHAEL 95608 REGISTRATION (OW/MGR) AD REM CHRISTOPHER PARKER 1729 1/2 L ST UNIT 2, PRACTITIONER No Website SACRAMENTO 95811 REGISTRATION (OW/MGR) AD REM KAI BRENNAN KIDD 1124 18TH ST, (916) 510-4823 PRACTITIONER No Website SACRAMENTO 95811 REGISTRATION AFFIRMATION TATTOO MELISSA STOCK 2400 21ST ST, (773) 603-6281 PRACTITIONER No Website SACRAMENTO 95818 REGISTRATION (OW/MGR) AFFIRMATION TATTOO GABRIELLE PERRINE 2400 21ST ST, (773) 603-6281 PRACTITIONER No Website SACRAMENTO 95818 REGISTRATION ALEX GARCIA ALEX GARCIA 8294 FOLSOM BLVD, (916) 388-2414 PRACTITIONER No Website SACRAMENTO 95826 REGISTRATION (OW/MGR) 1 Business Name Practitioner Address Phone Registration Type Website ALEXANDRIA PEREZ MOORE ALEXANDRIA PEREZ 8270 BELVEDERE AVE STE (925) 344-1889 PRACTITIONER No Website MOORE 100, SACRAMENTO -
Computational Studies of Actinide Complexes with Expanded Porphyrins
Computational Studies of Actinide Complexes with Expanded Porphyrins Poppy Di Pietro UCL PhD in Chemistry 1 I, Poppy Di Pietro, confirm that the work presented in this thesis is my own. Where information has been derived from other sources, I confirm that this has been indicated in the thesis. 2 Abstract Covalency in complexes of the actinides has been identified as the potential driving force behind selective behaviour exhibited by separation ligands of use to the nuclear industry. In this thesis, complexes of actinyls with hexadentate macrocyclic expanded porphyrin ligands are investigated at the density functional level of theory and their electron densities analysed in detail. Initially, strong correlations are established between the vibrational frequencies of the distinctive uranyl stretching modes and covalency in the equatorial bonds of several simple uranyl complexes with monodentate first row ligands, with redshift of the uranyl stretching modes indicating a weakening of the U-Oyl interaction as a result of competing interactions in the equatorial plane. Subsequently, strong similarities are established in the U-N and U-Oyl bonding character of two multidentate uranyl complexes: 2+ UO2-isoamethyrin(1.0.1.0.0.0) and [UO2(bis-triazinyl-pyridine)2] , where isoamethyrin(1.0.1.0.0.0) is a hexadentate macrocyclic expanded porphyrin ligand and bis-trizinyl-pyridine (BTP) is a tridentate ligand which has shown selectivity for An(III) over Ln(III). A series of uranyl hexaphyrin complexes is then investigated, finding moderate correlations between stability, equatorial covalency and the frequencies of the uranyl stretching modes, which crucially only hold when there is a degree of relative planarity in the ligand. -

Surnames Beginning With
Card# Mine Name Operator Year Month Day Surname First and Middle Name Age Fatal/Nonfatal In/Outside Occupation Nationality Citizen/Alien Single/Married #Children Mine Experience Occupation Exp. Accident Cause or Remarks Fault County Page# Mining Dist. Film# Bituminous 2 M Saxman 1902 1 7 Pablisko Stanny 38 nonfatal inside miner Polish alien fall of roof unavoidable 106 2nd 3593 Bituminous 4 Yatesboro 1903 1 15 Pace Modesto 27 fatal inside miner Italian alien single electric shock unavoidable 44 12th 3593 Bituminous 109 Acme 1906 8 10 Pacek Andrew 37 nonfatal inside loader Slavic alien fall of roof victim 202 1st 3593 Bituminous 13 Adrian No.1 1900 3 14 Pachana Raffael 40 fatal inside miner Italian alien married 4 injured by cars victim 42 4th 3593 Bituminous 102 Solon 1906 8 9 Pachanco Paul 30 nonfatal inside miner Hungarian alien burned by blast victim 267 16th 3593 Bituminous 17 Eureka No.36 1905 4 9 Pachina Joe 36 fatal inside miner Hungarian alien married killed by cars victim 154 6th 3593 Bituminous 17 Oak Hill No.5 1903 3 23 Pacifico Carlo 19 fatal inside miner Italian single fall of slate victim 54 14th 3593 Bituminous 71 Bear Run 1900 12 19 Packard Charles 22 nonfatal inside miner Amercian citizen fall of coal victim 44 4th 3593 Bituminous 6 Ponfeigh 1902 1 15 Packer W H 55 fatal inside miner Welsh citizen single fall of roof unavoidable 129 9th 3593 Bituminous 47 Moon Run 1904 5 27 Pacopsky Joseph 40 nonfatal outside blacksmith Austrian alien injured by a drill unavoidable 91 7th 3593 Bituminous 79 Alverton No.1 1904 10 6 Padolick -

Ridgefield Encyclopedia
A compendium of more than 3,300 people, places and things relating to Ridgefield, Connecticut. by Jack Sanders [Note: Abbreviations and sources are explained at the end of the document. This work is being constantly expanded and revised; this version was updated on 4-14-2020.] A A&P: The Great Atlantic and Pacific Tea Company opened a small grocery store at 378 Main Street in 1948 (long after liquor store — q.v.); became a supermarket at 46 Danbury Road in 1962 (now Walgreens site); closed November 1981. [JFS] A&P Liquor Store: Opened at 133½ Main Street Sept. 12, 1935. [P9/12/1935] Aaron’s Court: short, dead-end road serving 9 of 10 lots at 45 acre subdivision on the east side of Ridgebury Road by Lewis and Barry Finch, father-son, who had in 1980 proposed a corporate park here; named for Aaron Turner (q.v.), circus owner, who was born nearby. [RN] A Better Chance (ABC) is Ridgefield chapter of a national organization that sponsors talented, motivated children from inner-cities to attend RHS; students live at 32 Fairview Avenue; program began 1987. A Birdseye View: Column in Ridgefield Press for many years, written by Duncan Smith (q.v.) Abbe family: Lived on West Lane and West Mountain, 1935-36: James E. Abbe, noted photographer of celebrities, his wife, Polly Shorrock Abbe, and their three children Patience, Richard and John; the children became national celebrities when their 1936 book, “Around the World in Eleven Years.” written mostly by Patience, 11, became a bestseller. [WWW] Abbot, Dr. -

Non-Heme Iron Oxygenases: an Investigation of the Protein Ligand Effects on the Chemical Reactivity In
Non-Heme Iron Oxygenases: An Investigation of the Protein Ligand Effects on the Chemical Reactivity in MiaE and Cysteamine Dioxygenase by Philip Palacios Presented to the Faculty of the Graduate School of The University of Texas-Arlington in Partial Fulfillment of the requirements of the Degree of DOCTOR OF PHILOSOPHY THE UNIVERSITY OF TEXAS-ARLINGTON August 2019 Copyright © by Philip Palacios 2019 All Rights Reserved Acknowledgements Firstly, I want to express my sincere gratitude to my P.I. and friend, Dr. Brad Pierce, for his patience and support throughout these five years. It has been greatest honor to have worked under your guidance. I want to also thank my thesis committee members Dr. Rasika Dias, Dr. Robin Macaluso, and Dr. Jongyun Heo for their feedback throughout my graduate career. I want to thank all my coworkers that I’ve had the pleasure of working with throughout my graduate career; Josh, Sinjinee, Nick, Jared, Pender, Bender and the rest of the group. All of you made the experience of going to work enjoyable. We started out as lab mates and ended up as lifelong friends. I cannot think of a more perfect group of delinquents to spend these past five years with. Lastly, I want to thank my family and friends. To my family, you’ve always been a huge support of my dreams and I am not the person I am today without all that you have done and continue to do for me today. To my wonderful girlfriend, Diane, you’ve been the greatest gift in my life. I am not here without all your love and support throughout these years. -

Of Births Code 1 N 1 Surname T. Mother's Maiden Name Race
INDEX OF BIRTHS 1 N MOTHER'S DATE OF BIRTH REGISTERED CODE 1 RACE SEX NUMBER SURNAME T. MAIDEN NAME MO. DAY YR. MOOO MAYO CALVIN MULDROW 2 1 8 21 60 23323 MOOO MAY CHARLES LEE DUSCHL 1 2 11 5 60 32992 MOOO MAYO CICERO o j i GARR I S. ^ J 2 1 1 24 " 60 1865 ^ M h * {9- 0 i'' iTnl pvh-rf 4//1 ^ r- fi / > / nr-r rS -> MOUU A / U m 157%? MOOO MOYE CURTISS LEE" HAMLET 2 1 8 14 60 23375 MOOO MAY DOUGLAS JAME GREENE 1 2 1 28 60 2453 MOOO MAY DUNCAN GOUGH 1 1 10 9 60 29220 MOOO MAYHEW ELMER JOHN WARD 1 2 9 17 60 32448 MOOO MAYO ELNORA MC FAIL 2 2 7 4 60 17886 MOOO MAY FRANKLIN EUG MOBERLY 2 11 27 60 34648 MOOO MAY GARY PATRICK BECKER 2 9 20 60 26870 MOOO MAYO GEORGE EDWAR FULLER 1 7 23 60 20316 MOOO MAY IDWAL JOHN BURKE 1 13 60 22911 MOOO MAYO JESSIE MAE GOODMAN 1 5 60 21678 MOOO MAYO JOHN OAVIS JONES 2 v" 4 60 12964 / MOOO MAY JOSEPH RINGO 1 7 8 60 18795 1 MOOO MAY JOSEPHINE SMITH 1 1 26 60 2233 MOOO MAY KARL EDWIN CAVALLARO 2 4 26 60 11684 MOOO MAYO LAWRENCE JAM HUGGINS 2 12 29 60 37531 MOOO MAYO LEROY MILLER 2 2 1 60 5324 MOOO MAYO LINDSAY MC K MAYO 2 1 21 60 4378^ MOOO MAYO MARY ELI2ABE MACKEY 2 8 2 60 MOOO MAY MICHAEL KENN STOKES 1 9 16 60 MOOO MAY PAUL CLIFFOR KIMBERLY 1 11 29 60 MOOO mayhew PETER HAROLD BOLEY 1 2 1 13 60 MOOO MAYO PHILLIP DAVI BROWN 2 1 11 6 60 MOOO MAYO PHILLIP LEE WIGGINS 2 1 7 13 60 INDEX OF BIRTHS DATE OF BIRTH CODE MOTHER'S REGISTERED MAIDEN NAME MO. -

Hydrogel Scaffolds to Modulate Smooth Muscle Cell Phenotype
ENGINEERING POLY(ETHYLENE GLYCOL) HYDROGEL SCAFFOLDS TO MODULATE SMOOTH MUSCLE CELL PHENOTYPE by JEFFREY ALAN BEAMISH Submitted in partial fulfillment of the requirements For the degree of Doctor of Philosophy Dissertation Advisors: Dr. Roger E. Marchant and Dr. Kandice Kottke-Marchant Department of Biomedical Engineering CASE WESTERN RESERVE UNIVERSITY August, 2009 CASE WESTERN RESERVE UNIVERSITY SCHOOL OF GRADUATE STUDIES We hereby approve the thesis/dissertation of ______________________________________________________ candidate for the ________________________________degree *. (signed)_______________________________________________ (chair of the committee) ________________________________________________ ________________________________________________ ________________________________________________ ________________________________________________ ________________________________________________ (date) _______________________ *We also certify that written approval has been obtained for any proprietary material contained therein. To my loving wife, Susan, and my parents, who have provided unwavering support for all my endeavors Table of Contents Table of Contents ...............................................................................................................i List of Tables ....................................................................................................................iii List of Figures..................................................................................................................