No. 747 for Calcium Lactate in Potato and Vegetable Snacks and Sweetened Crackers
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

How to Fortify Beverages with Calcium by Dr
Ingredients How to Fortify Beverages With Calcium by Dr. Gerhard Gerstner Along with current developments of the overall functional foods market, the use of minerals and especially calcium salts is expected to exhibit strong growth rates. In contrary to other functional ingredients, calcium is widely known as being beneficial for human health and there is no need to explain its nutritional ad- vantages to the customer. According to Leatherhead International, future trends include growing consumer concern regarding osteoporosis and bone health, leading to increased sales of calcium salts. The con- observation is seen as being one of tinuous market growth drives mineral the main factors causing osteo- Common calium sources salt suppliers to offer not only one porosis 2 .As a consequence, national for beverage fortification product but rather a range of different authorities all over the world have calcium salts and granulations to be recently reconsidered recommend- Table 1 shows a typical range of able to tune them to industrial cus- ations in order to take remedial calcium fortified beverages which tomers’ applications. This article measures against calcium deficiency have been seen in European and US discusses important nutritional, and accordingly, to reduce the risk of supermarkets recently. Practically technological as well as economical osteoporosis. In this respect, the US every type of beverage such as aspects of calcium in beverages with National Institute of Health (NIH) has mineral water, soy milk, energy drink, a focus on our company’s products increased the amounts of optimal nectar or juice does have a fortified Tricalcium Citrate, Calcium Gluconate daily calcium intake and defined product line already. -

Factors Affecting Precipitation of Calcium Lactate from Fermentation Broths and from Aqueous Solution
https://doi.org/10.3311/PPch.14043 Creative Commons Attribution b |533 Periodica Polytechnica Chemical Engineering, 63(4), pp. 533–540, 2019 Factors Affecting Precipitation of Calcium Lactate from Fermentation Broths and from Aqueous Solution Aladár Vidra1, Áron Németh1*, András Salgó1 1 Department of Applied Biotechnology and Food Science, Faculty of Chemical Technology and Biotechnology, Budapest University of Technology and Economics, H-1111 Budapest, Budafoki út 6-8, Hungary * Corresponding author, e-mail: [email protected] Received: 19 March 2019, Accepted: 22 May 2019, Published online: 28 June 2019 Abstract Lactic acid is one of the most important organic acids which is being extensively used around the globe in a range of industrial and biotechnological applications. Lactic acid can be produced either by fermentation or by chemical synthesis but the biotechnological fermentation process has several advantages compared to the other one. However fermentation broth contains a number of impurities which must be removed from the broth in order to achieve more pure lactic acid. Efficiency of recovery is crucial to the economy of the whole process as well since the costs of separation and recovery are responsible for more than half of the entire cost of production. In the traditional procedure, the heated and filtered fermentation broth is concentrated to allow crystallization or precipitation of calcium lactate, followed by addition of sulphuric acid to remove the calcium in form of calcium sulphate. The disadvantage of this procedure is the relatively high solubility of calcium lactate which causes product loss in the crystallization step. Therefore we investigated the effects of four operating parameters of the crystallization/precipitation process from two different fermentation broths and from an aqueous solution. -

GHS Calcium Lactate Gluconate MSDS.Pdf
Safety Data Sheet (Calcium Lactate Gluconate) DATE PREPARED: 7/9/2015 Section 1. Product and Company Identification Product Name Calcium Lactate Gluconate CAS Number 11116-97-5 Parchem - fine & specialty chemicals EMERGENCY RESPONSE NUMBER 415 Huguenot Street CHEMTEL New Rochelle, NY 10801 Toll Free US & Canada: 1 (800) 255-3924 (914) 654-6800 (914) 654-6899 All other Origins: 1 (813) 248-0585 parchem.com [email protected] Collect Calls Accepted Section 2. Hazards Identification Classification of the substance or mixture Classification according to Directive 67/548/EEC or 1999/45/EC as amended: This preparation does not meet the criteria for classification according to Directive 1999/45/EC as amended. Classification according to Regulation (EC) No 1272/2008 as amended: This mixture does not meet the criteria for classification according to Regulation (EC) 1272/2008 as amended. Hazard and precautionary statements Hazard statements: The substance does not meet the criteria for classification. Precautionary statements: Not available. Appearance & Odor: White powder with no odor. Fire & Explosion Hazards Potential for dust explosion may exist. This product is not defined as flammable or combustible. However, the product may decompose under fire conditions to produce toxic oxides of carbon. Depending upon conditions, dusts may be sensitive to static discharge. Avoid possibility of dry powder and friction causing static electricity in presence of flammables (See NFPA-77, Chpt. 6) Primary Route of Exposure: Skin and eye contact are the primary routes of exposure to this product. Inhalation Acute Exposure: Inhalation of dust may cause mild irritation. Skin Contact - Acute: Skin contact is not expected to cause irritation. -

Fine Biocompatible Powders Synthesized from Calcium Lactate and Ammonium Sulfate
ceramics Article Fine Biocompatible Powders Synthesized from Calcium Lactate and Ammonium Sulfate Maksim Kaimonov 1,* , Tatiana Shatalova 1,2 , Yaroslav Filippov 1,3 and Tatiana Safronova 1,2 1 Department of Materials Science, Lomonosov Moscow State University, Building, 73, Leninskie Gory, 1, 119991 Moscow, Russia; [email protected] (T.S.); fi[email protected] (Y.F.); [email protected] (T.S.) 2 Department of Chemistry, Lomonosov Moscow State University, Building, 3, Leninskie Gory, 1, 119991 Moscow, Russia 3 Research Institute of Mechanics, Lomonosov Moscow State University, Michurinsky pr., 1, 119192 Moscow, Russia * Correspondence: [email protected]; Tel.: +7-952-889-11-43 Abstract: Fine biocompatible powders with different phase compositions were obtained from a 0.5 M solution of ammonium sulfate (NH4)2SO4 and calcium lactate Ca(C3H5O3)2. The powder ◦ after synthesis and drying at 40 C included calcium sulfate dehydrate CaSO4·2H2O and calcite ◦ CaCO3. The powder after heat treatment at 350 C included β-hemihydrate calcium sulfate β- CaSO4·0.5H2O, γ-anhydrite calcium sulfate γ-CaSO4 and calcite CaCO3. The phase composition of ◦ powder heat-treated at 600 C was presented as β-anhydrate calcium sulfate β-CaSO4 and calcite ◦ CaCO3. Increasing the temperature up to 800 C leads to the sintering of a calcium sulfate powder β β consisting of -anhydrite calcium sulfate -CaSO4 main phase and a tiny amount of calcium oxide CaO. The obtained fine biocompatible powders of calcium sulfate both after synthesis and after heat Citation: Kaimonov, M.; Shatalova, treatment at temperature not above 600 ◦C can be recommended as a filler for producing unique T.; Filippov, Y.; Safronova, T. -

Milk Allergy
Allergic reactions Allergic reactions are severe adverse reactions that occur when the body’s immune system overreacts to a particular allergen.These reactions may be caused by food, insect stings, latex, medications and other substances. In Canada, the nine priority food allergens Milk are peanuts, tree nuts, sesame seeds, milk, eggs, seafood (fish, crustaceans and shellfish), soy, wheat One of the nine most and sulphites (a food additive). common food allergens What are the symptoms of an allergic reaction? When someone comes in contact with an allergen, the symptoms of a reaction may develop quickly and rapidly progress from mild to severe. The most severe form of an allergic reaction is called anaphylaxis. Symptoms can include breathing difficulties, a drop in blood pressure or shock, which may result in loss of consciousness and even death. A person experiencing an allergic reaction may have any of the following symptoms: • Flushed face, hives or a rash, red and itchy skin • Swelling of the eyes, face, lips, throat and tongue • Trouble breathing, speaking or swallowing • Anxiety, distress, faintness, paleness, sense of doom, weakness • Cramps, diarrhea, vomiting • A drop in blood pressure, rapid heart beat, loss of consciousness How are food allergies and severe allergic reactions treated? Currently there is no cure for food allergies. The only option is complete avoidance of the specific allergen. Appropriate emergency treatment for anaphylaxis (a severe food allergy reaction) includes an injection of adrenaline, which is available in an auto-injector device. Adrenaline must be administered as soon as symptoms of a severe allergic reaction appear.The injection must be followed by further treatment and observation in a hospital emergency room. -

Sodium Reduction Made Easy with Sub4salt® Cure and Potassium
facts Sodium reduction made easy with sub4salt ® cure and potassium lactates Introduction There are two important considerations in the preparation of processed meat products. Firstly, a product that remains safe and stable for its entire shelf life is a must. Secondly, there is an increasing demand for healthier meat products. One of the major health trends in the processed meat market is sodium reduction, since these products usually contain high levels of salt. A high sodium intake is associated with negative effects on the human body such as hypertension, strokes and kidney disease. Potassium lactate and blends with acetates or diacetates accommodate both of these considerations. Jungbunzlauer provides solutions for the meat industry that ensure there is no microbiological growth in products over a long period of time, even at low use levels. Furthermore, choosing the right potassium-based ingredient can result in a sodium reduction of over 25% and, in combination with Jungbunzlauer’s sub4salt ® cure, a 1:1 curing salt substitute, a sodium reduction of over 50% is possible. 2 Why reduce sodium? Changing lifestyles and rapid urbanization have caused a shift in dietary patterns to consuming more highly processed food and further from a diet focusing on fresh fruits and vegetables. Processed food is not only usually more calorie-dense and high in saturated fats, trans fats, sugars and salt, but also lower in potassium as this highly soluble mineral is washed out during processing. [20] Due to the reasons above, arteriosclerosis and hypertension are common in the modern Western world leading to cardio - vascular diseases (CVD). -

An Overview of Functional Non-Meat Ingredients in Meat Processing: the Current Toolbox
PROCESSOR’S CHALLENGES IN ADDRESSING NEW MARKET/CONSUMER DEMANDS An Overview of Functional Non-Meat Ingredients in Meat Processing: The Current Toolbox Joseph G. Sebranek INTRODUCTION ing the use of these “toolbox” ingredients is not only the critical nature of the roles they play but also because these My “assignment” as part of this discussion of the chal- are all multifunctional ingredients. Because they impact lenges facing meat processors trying to meet consumer several important properties of processed meats, attempt- demands for clean labels is to review the critical func- ing to reduce or eliminate these ingredients has implica- tional roles of the fundamental non-meat ingredients that tions for multiple changes in the product. are essential for processed meats. The market pressure for shorter, simpler, easier-to-understand ingredient state- WATER ments is providing considerable motivation for processors to reduce or even eliminate some of the traditional, well- One of the functional non-meat ingredients in the current established non-meat ingredients. However, the practical toolbox that is often overlooked is water. While water applications of many of the traditional non-meat ingredi- is a major component of lean meat, it is also commonly ents have been developed and refined as a result of years, added to many processed meat products, and, as such, decades or even centuries of use, and have clearly evolved becomes a non-meat ingredient. Water plays an impor- to play very critical roles in processed meats. These ingre- tant functional role in processed meats which is likely to dients comprise the “current toolbox” that provides the be modified if other ingredients are changed. -

Solubilities of Calcium and Zinc Lactate in Water and Water-Ethanol Mixture
Korean J. Chem. Eng., 18(1), 133-135 (2001) SHORT COMMUNICATION Solubilities of Calcium and Zinc Lactate in Water and Water-Ethanol Mixture Xuejun Cao*, Ho-Joon Lee, Hyun Shik Yun and Yoon-Mo Koo† *State Key Laboratory of Bioreactor Engineering, Department of Biochemical Engineering, East China University of Science and Technology, Shanghai, 200237, China Department of Biological Engineering, Inha University, 253 Yonghyundong, Namku, Inchon, 402-751, Korea (Received 21 August 2000 • accepted 26 December 2000) Abstract−The solubility of lactate salts, L(+) and DL(±) forms of calcium and zinc lactate in water at temperature between 5 and 80 oC, was measured and empirical equations were obtained by regression of solubility-temperature data. The equations can be used to calculate the solubility of calcium and zinc lactate at a given temperature. The change in solubility of L(+) and DL(±) calcium and zinc lactate in water-ethanol mixture at 20 oC was also in- vestigated. The solubilities of calcium and zinc lactate were lowered by the addition of ethanol to the solution. Key words: Solubility, Calcium Lactate, Zinc Lactate INTRODUCTION reached an equilibrium at a given temperature. The attainment of equilibrium was checked by measuring the concentration of sam- Calcium and zinc lactates are important chemicals in the lactic ples every 30 min. Salts were added until they formed precipitates. acid industry, and calcium lactate crystallization is a popular com- Tested temperature range was between 5 and 80 oC with 5 oC in- mercial separation method of lactic acid. Calcium and zinc salts of tervals. If necessary, a short temperature interval was applied. -
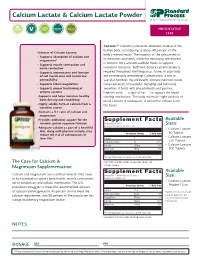
Calcium Lactate Fact Sheet
Calcium Lactate & Calcium Lactate Powder PREVENTATIVE CARE Calcium:2,3 Calcium is the most abundant mineral in the human body, contributing to about 40 percent of the Features of Calcium Lactate: body’s mineral mass. The majority of the calcium exists • Supports absorption of calcium and in the bones and teeth, while the remaining one percent magnesium* is found in intra and extracellular fluids to support • Supports muscle contraction and nerve conduction metabolic functions. Sufficient dietary calcium intake is • Supports maintenance and function required throughout the lifespan as bones in your body of cell membranes and membrane are continuously remodeling. Calcium plays a role in permeability vascular function, muscle health, immune function, nerve • Supports blood coagulation communication, intracellular signaling and hormonal • Supports proper functioning of secretion. It binds with phospholipids and gamma- enzyme systems linolenic acids — a type of fat — to support the blood •Supports and helps maintain healthy clotting mechanism. The body maintains tight controls of bone density and remodeling blood calcium; if inadequate, it will utilize calcium from •Highly soluble form of calcium from a the bones. nondairy source •Contains a 5:1 ratio of calcium and magnesium •Provides additional support for the Supplement Facts Available immune system response function Serving Size: 6 Tablets Sizes: Servings per Container: 15, 55, or 133 •Adequate calcium as part of a healthful . • Calcium Lactate diet, along with physical activity, may 90 Tablets reduce the risk of osteoporosis in Amount per Serving % Daily Value • Calcium Lactate later life.* Calories 5 Total Carbohydrate 1g <1%* 330 Tablets Calcium 250mg 19% • Calcium Lactate Magnesium 50mg 12% 800 Tablets . -

CALCIUM-SANDOZ® Novartis Consumer Health Calcium Preparations Calcium Therapy Indications and Clinical Uses: As a Dietary Suppl
CALCIUM-SANDOZ® Novartis Consumer Health Calcium Preparations Calcium Therapy Indications And Clinical Uses: As a dietary supplement where calcium intake may be inadequate: childhood and adolescence, pregnancy and lactation, postmenopausal females and in the aged. In the treatment of calcium deficiency states which may occur in diseases such as: tetany of the newborn (as a supplement to parenterally administered calcium), hypoparathyroidism (acute and chronic), pseudo-hypoparathyroidism, postmenopausal and senile osteoporosis, rickets and osteomalacia. Contra-Indications: Hypercalcemia and hypercalciuria (e.g. hyperparathyroidism, vitamin D overdosage, decalcifying tumors such as plasmocytoma, bone metastases); severe renal disease; and in calcium loss due to immobilization. Hypersensitivity to any of the components of Calcium-Sandoz. Although no concrete evidence is available about the metabolic process leading from calcium glucono-galacto-gluconate to galactose, it is advisable not to administer to galactosemic patients. Precautions: For diabetic patients, consideration should be given to the sucrose content of 719 mg/tablet of Calcium-Sandoz Forte. Gramcal and Calcium-Sandoz Syrup are suitable for sodium and potassium restricted diets. Calcium-Sandoz Forte is suitable for potassium restricted diets. Because of the presence of sodium (12 mmol), Calcium-Sandoz Forte is not suitable for sodium restricted diets. In mild hypercalciuria (exceeding 300 mg/24 hours) as well as in chronic renal failure, or where there is evidence of stone formation in the urinary tract, adequate checks must be kept on urinary calcium excretion. If necessary the dosage should be reduced or calcium therapy discontinued. In patients prone to formation of calculi in the urinary tract an increased fluid intake is recommended. -

24 May 2016 Agen
EUROPEAN COMMISSION HEALTH AND FOOD SAFETY DIRECTORATE-GENERAL Ares (2016) 2537654 Standing Committee on Plants, Animals, Food and Feed Section Animal Nutrition 23 MAY 2016 - 24 MAY 2016 CIRCABC Link: https://circabc.europa.eu/w/browse/e360a1b3-c86e-4696-8122-f8c95d0412c5 AGENDA Section A Information and/or discussion A.01 Feed Additives - Applications under Regulation (EC) No 1831/2003 Art. 4 or 13. (MP) New applications (copies). A.02 Feed Additives - Applications under Regulation (EC) No 1831/2003 Art. 9. (MP + AR + WT) Discussion on EFSA Scientific Opinions on the safety and efficacy of : A.02.1. a natural mixture of dolomite plus magnesite and magnesium- phyllosilicates (Fluidol) as feed additive for all animal species - Annex A.02.2. Friedland clay (montmorillonite–illite mixed layer clay) when used as a technological additive for all animal species - Annex A.02.3. malic acid, sodium malate and calcium malate for all animal species - Annex A.02.4. propionic acid, sodium propionate, calcium propionate and ammonium propionate for all animal species - Annex A.02.5. formic acid, ammonium formate and calcium formate for all animal species - Annex A.02.6. lactic acid and calcium lactate for all animal species - Annex A.02.7. sodium benzoate as silage additive - Annex Created: 04-05-2016 14:58:28 Page 1 A.02.8. acetic acid, sodium diacetate and calcium acetate for all animal species - Annex A.02.9. sorbic acid and potassium sorbate for all animal species - Annex A.02.10. citric acid for all animal species - Annex A.02.11. concentrated liquid L-lysine (base), L-lysine monohydrochloride and L- lysine sulphate produced using different strains of Corynebacterium glutamicum for all animal species based on a dossier submitted by AMAC/EEIG A.02.12. -

Quintessenz Journals
pyri Co gh Not for Publicationt b y Q u i N n o t t r f e o Remineralisation of Enamel Subsurface Lesions by Xylitol Chewingssence Gum Containing Calcium Hydrogen Phosphate and Funoran Xiao Ling WANG1, Ye Hua GAN2, Yao GE1, Chuo Yue CHENG1, Xiao Chi CHEN1, Wen Hui WANG1, Bo Xue ZHANG1 Objective: To investigate the effects of xylitol chewing gum containing calcium hydrogen phos- phate and funoran (a polysaccharide extracted from seaweed) on initial enamel lesions. Methods: The clinical trial of the study was double blind. Human enamel blocks with artifi- cial subsurface lesions were mounted in oral devices in 15 subjects. The subjects served as their own controls and were instructed to chew the three different gums, containing: (1) 79% su- crose (S), (2) 40% xylitol (X) and (3) 40% xylitol plus calcium hydrogen phosphate and funo- ran (X+2), 7 times daily, for a period of 1 week each respectively. Mineral content within the lesions after chewing each gum was analysed by quantitative microradiography. All data were analysed statistically using a one-way ANOVA test. Results: After chewing the gums, the amount of mineral at all depths of subsurface lesion was highest in the X+2 group, followed by the X group and then the S group. The difference be- tween the groups was statistically significant (p < 0.01), especially in the lesion body. Conclusion: Xylitol chewing gum containing calcium hydrogen phosphate and funoran sig- nificantly enhanced the remineralisation of initial human enamel lesions in situ. Key words: calcium hydrogen phosphate, enamel subsurface lesion, funoran, remineralisa- tion, xylitol chewing gum ylitol is generally considered to be non-cariogenic explain the caries-inhibitory effects of xylitol as a total Xas it is not fermented by oral bacteria.