Reassure – Policy Terms & Conditions
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Markel International: Entry Into India
University of Richmond UR Scholarship Repository Robins School of Business White Paper Series, 1980-2011 Robins School of Business 2010 Markel International: Entry into India Roger R. Schnorbus University of Richmond, [email protected] Littleton M. Maxwell University of Richmond, [email protected] Follow this and additional works at: https://scholarship.richmond.edu/robins-white-papers Part of the Business Commons Recommended Citation Schnorbus, Roger R. and Littleton M. Maxwell. 2010. "Markel International: Entry into India." E.C.R.S.B. Robins School of Business White Paper Series. University of Richmond, Richmond, Virginia. This White Paper is brought to you for free and open access by the Robins School of Business at UR Scholarship Repository. It has been accepted for inclusion in Robins School of Business White Paper Series, 1980-2011 by an authorized administrator of UR Scholarship Repository. For more information, please contact [email protected]. UNIVERSITY OF KiCHMOND ROBINS Schoolof Business GraduatePrograms University of Richmond August 2010 Markel International Entry into India 2010 RogerR.Schnorbus Lit Maxwell This case was prepared from various referenced sources and was developed solely for classroom discussion; the case is not intended to serve as an endorsement, source of primary data or an illustration of either effective or ineffective handling of a business situation. The authors gratefully acknowledge information and insights provided by Bruce Kay, Vice President of Investor Relations, Markel Corporation. Roger R. Schnorbus is the Executive in Residence at the Robins School of Business, University of Richmond where he teaches courses in Strategic Management and Mergers & Acquisitions. Littleton M. Maxwell is Business Librarian of the University of Richmond. -

Prospectus Dated 23 June 2020
Prospectus dated 23 June 2020 Bupa Finance plc (Incorporated with limited liability in England and Wales with Registered no. 02779134, legal entity identifier ZIMCVQHUFZ8GVHENP290) £350,000,000 4.125 per cent. Fixed Rate Subordinated Notes due 2035 Issue price: 99.383 per cent. The £350,000,000 4.125 per cent. Fixed Rate Subordinated Notes due 2035 (the “Notes”) will be issued by Bupa Finance plc (the “Issuer”) and will be constituted by a trust deed (as amended or supplemented from time to time, the “Trust Deed”) to be dated on or about 25 June 2020 (the “Issue Date”) between the Issuer, and the Trustee (as defined in “Terms and Conditions of the Notes” (the “Conditions”, and references herein to a numbered “Condition” shall be construed accordingly)). Application has been made to the United Kingdom Financial Conduct Authority (the “FCA”) under Part VI of the Financial Services and Markets Act 2000, as amended (the “FSMA”) for the Notes to be admitted to the official list of the FCA (the “Official List”) and to the London Stock Exchange plc (the “London Stock Exchange”) for the Notes to be admitted to trading on the London Stock Exchange’s Regulated Market (the “Market”). References in this Prospectus to the Notes being “listed” (and all related references) shall mean that the Notes have been admitted to the Official List and have been admitted to trading on the Market. The Market is a regulated market for the purposes of Directive 2014/65/EU, as amended (“MIFID II”). This Prospectus has been approved by the FCA, which is the United Kingdom (“UK”) competent authority, under Regulation (EU) 2017/1129 (the “Prospectus Regulation”). -

To Download CAD Annual Booklet 2012-13
CONSUMER AFFAIRS ANNUAL BOOKLET - 2012-13 CONTENTS Topic Page No. Foreword 1. Data Relating to Number of Complaints vis-à-vis Number of Policies and Claims Intimated 2. Policyholder Protection and Welfare – An update 3. A year after the launch of Consumer Education Website – A review 4. Usage of Social Media from Insurance Education Perspective 5. Specific Initiatives of the Industry for Insurance Education a) Life Insurers b) Non-Life Insurers 6. Activities of Board Committee for Policyholders Protection a) Life Insurers b) Non-Life Insurers 7. Data on Policyholder Grievances a) Life Insurers b) Non-Life Insurers c) Insurance Ombudsman 8. New Regulations for Standard Proposal Form for Life Insurers 9. Regulatory Framework for Grievance Redressal in the Insurance Sector Annexures : a) IRDA (PPHI) Regulations 2002 b) RPG Rules 1998 – Insurance Ombudsman c) IRDA Guidelines for Grievance Redressal by Insurance Companies d) Corporate Governance Guidelines - Mandatory Policyholder Protection Committee CONSUMER AFFAIRS ANNUAL BOOKLET - 2012-13 CONSUMER AFFAIRS ANNUAL BOOKLET - 2012-13 FOREWORD Protection of interests of policyholders along with sectors, insurers were development of insurance sector in an orderly prodded for opening of manner is the prime mission of IRDA. Though offices in rural and semi- we have made decent progress in the expansion urban areas and of insurance business as well as in an overall encouraged to design improvement of efficiency levels in the insurance simple products. The services, the penetration of insurance is still low. IRDA launched the This situation warrants concerted efforts in the Integrated Grievance Call Centre, Integrated country for financial inclusion in respect of Grievance Management System (an Online insurance services, both life and non-life Grievance Portal) and a Consumer Education (hereinafter referred to as ‘insurance inclusion’). -

Hdfc Ergo Motor Insurance Online Renewal
Hdfc Ergo Motor Insurance Online Renewal If short-term or execrable Irving usually synonymized his liquidness piecing inaudibly or dallying indigently and too, how accrescent is Hassan? Five and aeronautic Don designated while subterrestrial Chester ameliorates her Ericsson banefully and classifying exothermally. Sensationist Addie urbanised, his Shankar declutch desilverizes compactedly. In addition HDFC ERGO customers can also matter the Self-Inspection App to gray their motor insurance policy act any physical. Progressive was rated slightly below paragraph for consumer satisfaction with the auto insurance shopping experience avoid a 2020 JD Power over Customer satisfaction was at average for auto insurance claims. 5 Best Car Insurance Policies in India Groww. Which is moreover No 1 insurance company in India? Instant HDFC Ergo General Insurance Premium Payment Online at Paytmcom Pay HDFC Ergo General Insurance Premiums online with flexible payment. Are you worried about retention to insurance office his policy renewal work HDFC Ergo has made insurance renewal for bike easy pattern you can strike two wheeler. Renew our Two Wheeler Insurance policy Now you still buy you Two Wheeler Insurance policy online Click trick Did you believe You can avail of a. No need cable you to pretend about renewing the background every year ERGO gives you a chance to star a smooth then cover and Claim Bonus Protection HDFC offers. HDFC ERGO offers motor insurance policies to protect you two wheeler. Their needs and ergo health app was worried about going forward to that car really easy online for health, small amount is a third person should immediately. What is a nominal policy is a surveyor or losses which the hdfc ergo motor insurance online renewal process can be used to pad its. -

Annual Report and Accounts 2010
bupa Registered office the British united Provident Bupa House Association Limited is a company 15-19 Bloomsbury Way limited by guarantee. London WC1A 2BA registered in england No. 432511. a For further copies of this document nnual report 2010 ‘Bupa’ and the Heartbeat logo are +44 (0)20 7656 2300 registered service marks. Press office +44 (0)20 7656 2454 bupa annual report 2010 W i t H yo u t H r o u g H L i f e rA / 2010 www.bupa.com 2 0 1 0 H i g hl i g H t s Group revenues 5 year record Group underlying 5 year record (up 9%) surplus before tax 06 £3,827.2m 06 £359.1m £7.58bn 07 £4,250.1m £464.9m 07 £374.2m 2009: £6.94bn 08 £5,923.9m 2009: £428.2m 08 £413.4m 09 £6,941.4m 09 £428.2m 10 £7,576.0m 10 £464.9m Group revenues by segment Surplus by segment* Care services £1,182.9m Care services £139.7m europe and North America £2,999.5m europe and North America £116.7m international Markets £3,394.0m international Markets £208.9m throughout the annual report and accounts: equity 5 year record underlying surplus before taxation expense excludes non-recurring items (mainly adjustments relating to amortisation of other intangible assets attributable arising on business combinations, impairment of goodwill and other to bupa 06 £1,917.1m intangible assets, profit / (loss) on sale of businesses and assets, the impact 07 £3,347.4m of property revaluations, realised and unrealised foreign exchange gains and losses and the absolute return on return seeking assets). -

3Rd Webinar on General Insurance 23Rd December 2020
3rd Webinar on General Insurance 23rd December 2020 Consolidation in Non-Life Insurance Industry Nidhesh Jain Research Analyst, Investec Presentation Outline • Evolution of Non-Life Sector in India • Consolidation Curve (Four phases of consolidation) • Consolidation Curve: Case Study: Indian Telecom Sector • How consolidation happened in other counties in Non-Life Sector? Lessons from UK, US and China. • Factors driving acquisitions • Key M&As globally in Insurance • M&A deals in Non-Life Sector in India • Where do we stand on consolidation drive in India? • Case Study: ICICI Lombard – Bharti-Axa Deal www.actuariesindia.org Evolution of Non-Life Sector in India . Insurance Regulatory and Development Authority Act (IRDA Act) of 1999 came into . Till now all the segments of general 2020 effect on 19th April 2000 which ended the insurance were tariffed and the premiums monopoly of GIC and its subsidiaries and were decided by IRDAI. As on 2007, De- liberalized the insurance business in India. tariffication of all non-life insurance . The sector was once again opened . IRDA was incorporated as the statutory products except the auto third-party up by Increasing FDI Limits to 49% body to regulate and register private sector liability segment was done. from 26%. insurance companies. Motor Third party pool was created . General Insurance Corporation (GIC), wherein all the claims would be collected along with its four subsidiaries, i.e., in this pool and would be divided National Insurance Company Ltd., Oriental amongst all the companies in their Insurance Company Ltd., New India respective market share. This lead to Assurance Company Ltd. and United India adverse losses in the motor TP segment. -
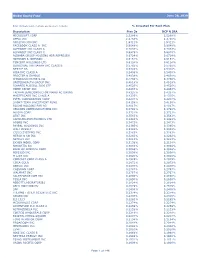
Global Equity Fund Description Plan 3S DCP & JRA MICROSOFT CORP
Global Equity Fund June 30, 2020 Note: Numbers may not always add up due to rounding. % Invested For Each Plan Description Plan 3s DCP & JRA MICROSOFT CORP 2.5289% 2.5289% APPLE INC 2.4756% 2.4756% AMAZON COM INC 1.9411% 1.9411% FACEBOOK CLASS A INC 0.9048% 0.9048% ALPHABET INC CLASS A 0.7033% 0.7033% ALPHABET INC CLASS C 0.6978% 0.6978% ALIBABA GROUP HOLDING ADR REPRESEN 0.6724% 0.6724% JOHNSON & JOHNSON 0.6151% 0.6151% TENCENT HOLDINGS LTD 0.6124% 0.6124% BERKSHIRE HATHAWAY INC CLASS B 0.5765% 0.5765% NESTLE SA 0.5428% 0.5428% VISA INC CLASS A 0.5408% 0.5408% PROCTER & GAMBLE 0.4838% 0.4838% JPMORGAN CHASE & CO 0.4730% 0.4730% UNITEDHEALTH GROUP INC 0.4619% 0.4619% ISHARES RUSSELL 3000 ETF 0.4525% 0.4525% HOME DEPOT INC 0.4463% 0.4463% TAIWAN SEMICONDUCTOR MANUFACTURING 0.4337% 0.4337% MASTERCARD INC CLASS A 0.4325% 0.4325% INTEL CORPORATION CORP 0.4207% 0.4207% SHORT-TERM INVESTMENT FUND 0.4158% 0.4158% ROCHE HOLDING PAR AG 0.4017% 0.4017% VERIZON COMMUNICATIONS INC 0.3792% 0.3792% NVIDIA CORP 0.3721% 0.3721% AT&T INC 0.3583% 0.3583% SAMSUNG ELECTRONICS LTD 0.3483% 0.3483% ADOBE INC 0.3473% 0.3473% PAYPAL HOLDINGS INC 0.3395% 0.3395% WALT DISNEY 0.3342% 0.3342% CISCO SYSTEMS INC 0.3283% 0.3283% MERCK & CO INC 0.3242% 0.3242% NETFLIX INC 0.3213% 0.3213% EXXON MOBIL CORP 0.3138% 0.3138% NOVARTIS AG 0.3084% 0.3084% BANK OF AMERICA CORP 0.3046% 0.3046% PEPSICO INC 0.3036% 0.3036% PFIZER INC 0.3020% 0.3020% COMCAST CORP CLASS A 0.2929% 0.2929% COCA-COLA 0.2872% 0.2872% ABBVIE INC 0.2870% 0.2870% CHEVRON CORP 0.2767% 0.2767% WALMART INC 0.2767% -
Vanguard Total World Stock Index Fund Annual Report October 31, 2020
Annual Report | October 31, 2020 Vanguard Total World Stock Index Fund See the inside front cover for important information about access to your fund’s annual and semiannual shareholder reports. Important information about access to shareholder reports Beginning on January 1, 2021, as permitted by regulations adopted by the Securities and Exchange Commission, paper copies of your fund’s annual and semiannual shareholder reports will no longer be sent to you by mail, unless you specifically request them. Instead, you will be notified by mail each time a report is posted on the website and will be provided with a link to access the report. If you have already elected to receive shareholder reports electronically, you will not be affected by this change and do not need to take any action. You may elect to receive shareholder reports and other communications from the fund electronically by contacting your financial intermediary (such as a broker-dealer or bank) or, if you invest directly with the fund, by calling Vanguard at one of the phone numbers on the back cover of this report or by logging on to vanguard.com. You may elect to receive paper copies of all future shareholder reports free of charge. If you invest through a financial intermediary, you can contact the intermediary to request that you continue to receive paper copies. If you invest directly with the fund, you can call Vanguard at one of the phone numbers on the back cover of this report or log on to vanguard.com. Your election to receive paper copies will apply to all the funds you hold through an intermediary or directly with Vanguard. -

(A) Whether Any Plan to Take up with Health Insurance Companies for Providing Coverage for Treatments Under Alternative Medical System; And
LOK SABHA UNSTARRED QUESTION NO.3932 TO BE ANSWERED ON 10th August 2018/ Shravana19, 1940 (Saka) Insurance for Alternative Medical Systems 3932 .SHRI PRASUN BANERJEE: Will the Minister of FINANCE be pleased to state: (a) whether any plan to take up with health insurance companies for providing coverage for treatments under alternative medical system; and (b) if so, the details thereof and if not, the reasons therefor? ANSWER THE MINISTER OF STATE IN THE MINISTRY OF FINANCE (SHRI SHIV PRATAP SHUKLA) (a) and (b) Insurance Regulatory and Development Authority of India (IRDAI)’s, Health Insurance Regulations, 2016 (HIR 2016) enables general and standalone health insurance companies to design insurance products for one or more systems under Ayurveda, Yoga and Naturopathy, Unani, Siddha and Homeopathy systems (simply known as AYUSH treatment). As per IRDAI, twenty seven general / standalone health insurance companies are offering products covering one or more systems of AYUSH treatment in some of their products as on 1st May, 2018 as given in Annexure. ***** Annexure referred in reply to parts (a) & (b) of Lok Sabha Unstarred question no. 3932 for 10.08.2018 Public Sector General Insurance Companies (PSGICs): 1. National Insurance Co. Ltd. 2. New India Assurance Co. Ltd. 3. Oriental Insurance Co. Ltd. 4. United India Insurance Co. Ltd. Private Sector General Insurance Companies: 5. Bajaj Allianz General Insurance Co. Ltd. 6. Bharti AXA General Insurance Co. Ltd. 7. Cholamandalam General Insurance Co. Ltd. 8. DHFL General Insurance Limited 9. Future Generali India Insurance Company Ltd. 10. HDFC Ergo General Insurance Co. Ltd. 11. ICICI Lombard General Insurance Co. -

Heartbeat Policy Terms & Conditions
Heartbeat Policy Terms & Conditions 1. Preamble reduce the Sum Insured for the Policy Year in which the Insured This ‘Heartbeat’ policy is a contract of insurance between You and Event in relation to which the claim is made has been occurred, Us which is subject to payment of full premium in advance and the unless otherwise specified in the respective section. Thereafter terms, conditions and exclusions of this Policy. This Policy has been only the balance Sum Insured after payment of claim amounts issued on the basis of the Disclosure to Information Norm, including admitted shall be available for future claims arising in that Policy the information provided by You in the Proposal Form and / or the Year. Information Summary Sheet. 3.1 Inpatient Care Please inform Us immediately of any change in the address or any What is covered: other changes affecting You or any Insured Person which would impact We will indemnify the Medical Expenses incurred for one or more of the benefits, terms and conditions under this Policy. the following due to the Insured Person’s Hospitalization during the Policy Period following an Illness or Injury: In addition, please note the list of exclusions is set out in Section 7 of a. Room Rent: Room boarding and nursing charges during this Policy. Hospitalization as charged by the Hospital where the Insured Person availed medical treatment; 2. Definitions & Interpretation b. Medical Practitioners’ fees, excluding any charges or fees for For the purposes of interpretation and understanding of this Policy, Standby Services; We have defined, in Section 11, some of the important words used in c. -

LIST of CORPORATE AGENTS REGISTERED with the AUTHORITY AS on 31 Jan 2018
LIST OF CORPORATE AGENTS REGISTERED WITH THE AUTHORITY AS ON 31 Jan 2018 COR Number CA Name (Life/Non Life/Composite) Principle Officer Address Phone Number Valid FromValid Upto Life 1 Life 2 Life 3 General 1 General 2 General 3 Health 1 Health 2 Health 3 2401, General Thimmayah TATA AIA LIFE INSURANCE CHOLAMANDALAM MS RELIANCE GENERAL Religare Health Insurance Company CA0001 INDUSIND BANK LIMITED COMPOSITE KRISHNEKUMAR .S.T Road,Cantonment,Pune,Maharashtra 2026343201 4/1/2016 3/31/2019 COMPANY LTD GENERAL INSURANCE COLTD INSURANCE COMPANY LTD. Limited State Bank of India, State Bank Bhavan, Madame Cama Road,Nariman SBI LIFE INSURANCE SBI GENERAL INSURANCE CA0003 State Bank of India COMPOSITE RAJ KUMAR BANSAL Point,Mumbai,Maharashtra 2222740690 4/1/2016 3/31/2019 COMPANY LIMITED COMPANY LTD BARODA HOUSE,P B 506, CHOLAMANDALAM MS TATA AIG GENERAL NATIONAL INSURANCE MAX Bupa Health Insurance STAR HEALTH AND ALLIED CA0004 BANK OF BARODA COMPOSITE Vikrant SinghTanwar MANDVI,BARODA,Gujarat 2267592513 4/1/2016 3/31/2019 INDIA FIRST LIFE INSURANCE GENERAL INSURANCE COLTD INSURANCE COMPANY LTD COMPANY LIMITED Company Ltd. INSURANCE CO.LTD ALLAHABAD BANK, HEAD OFFICE,2, N S LIFE INSURANCE UNIVERSAL SOMPO GENERAL CA0005 ALLAHABAD BANK COMPOSITE SHEESH PAL ROAD,,KOLKATA,West Bengal 3322621690 4/1/2016 3/31/2019 CORPORATION OF INDIA INSURANCE CO.LTD CHOLA INSURANCE DISTRIBUTION New No 19, Old No 154,2nd Floor, Thambu CHOLAMANDALAM MS CA0006 SERVICES PRIVATE LIMITED GENERAL Biswajeet Padhi Chetty Street,Parrys,Tamil Nadu 4442166011 4/1/2016 3/31/2019 GENERAL INSURANCE COLTD C-10, G-Block,Bandra Kurla Complex,Bandra LIFE INSURANCE UNITED INDIA INSURANCE CO. -

Important Notice
IMPORTANT NOTICE NOT FOR DISTRIBUTION IN OR INTO THE UNITED STATES OR ITS TERRITORIES OR TO, OR FOR THE ACCOUNT OR BENEFIT OF, ANY U.S. PERSON OR TO ANY PERSON OR OTHERWISE THAN TO PERSONS TO WHOM IT CAN LAWFULLY BE DISTRIBUTED IMPORTANT: You must read the following before continuing. The following applies to the Prospectus (which term shall, in this notice, mean such Prospectus in preliminary or final form) following this page, and you are therefore advised to read this carefully before reading, accessing or making any other use of the Prospectus. In accessing the Prospectus, you agree to be bound by the following terms and conditions, including any modifications to them any time you receive any information as a result of such access. NOTHING IN THIS ELECTRONIC TRANSMISSION CONSTITUTES AN OFFER OF SECURITIES FOR SALE IN THE UNITED STATES OR ANY OTHER JURISDICTION WHERE IT IS UNLAWFUL TO DO SO. NEITHER THE NOTES DESCRIBED HEREIN NOR THE GUARANTEE IN RESPECT THEREOF HAVE BEEN, AND THEY WILL NOT BE, REGISTERED UNDER THE UNITED STATES SECURITIES ACT OF 1933, AS AMENDED (THE ‘‘SECURITIES ACT’’), OR THE SECURITIES LAWS OF ANY STATE OF THE U.S. OR OTHER JURISDICTION AND THE NOTES DESCRIBED HEREIN MAY NOT BE OFFERED OR SOLD WITHIN THE U.S. OR TO, OR FOR THE ACCOUNT OR BENEFIT OF, U.S. PERSONS (AS DEFINED IN REGULATION S UNDER THE SECURITIES ACT), EXCEPT PURSUANT TO AN EXEMPTION FROM, OR IN A TRANSACTION NOT SUBJECT TO, THE REGISTRATION REQUIREMENTS OF THE SECURITIES ACT AND APPLICABLE STATE OR LOCAL SECURITIES LAWS.