Haryana Medical Journal March 2017
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Healthcare Sector in India Flanders Investment & Trade Market Survey
HEALTHCARE SECTOR IN INDIA FLANDERS INVESTMENT & TRADE MARKET SURVEY Healthcare Sector in India Flanders Investment & Trade Economic Representation of Flanders c/o Embassy of Belgium 50 - N, Shantipath, Chanakyapuri New Delhi - 110 021 India [email protected] T: +91 11 42 42 81 00 F: +91 11 42 42 81 10 Studie Healthcare Sector in India | juni 2015 1 2 TABLE OF CONTENTS ICT in Healthcare Services in India ................................................................................................. 8 Introduction ......................................................................................................................................... 8 Healthcare Information & Communication Technology (HICT) ...................................................... 9 Patient Monitoring & Tracking ........................................................................................................ 9 Healthcare Information Technology (HIT) ..................................................................................... 10 National Health Policy ................................................................................................................... 10 Health Information Management Systems (HIMS) ....................................................................... 10 Grading of Indian States for the use of ICT in Hospitals ................................................................ 12 Telemedicine .................................................................................................................................... -

Arrear List for :Feb-2018 16-03-2018 02:36:37 Page 1 of 183 Bill Group: PRIVATE (Electricity & Water Bill)
Arrear List for :Feb-2018 16-03-2018 02:36:37 Page 1 of 183 Bill Group: PRIVATE (Electricity & Water Bill) AS ON 28/02/2018 (in `) Sno Name Address E/W Arrear Lpsc Total Arrear KRISHAN DUTT 1 LAT NO 9-10 E BLOCK CON PLACE, NEW DELHI - 110001 W 5124036. 6463333. 11587370.18 23 95 KHALSA TENT HOUSE 2 SHOP NO 27 H C PLACE, NEW DELHI - 110001 E 6443220. 1409128. 7852349.49 73 76 SARDAR EXHIBITORS P LTD 3 74-75 SCINDIA HOUSE, NEW DELHI - 110001 E 96275.66 5867225. 5963501.61 95 SUBHASH KUMAR 4 M 11 MIDDLE CIRCLE CONNAUGHT PLACE, NEW DELHI - 110001 E 4116345. 399542.6 4515888.32 70 2 SECURITY WHITE HOUSE APPTT, OWNER 5 WELFARE ASSO. REGISTRAR, 10 BHAGWAN, DASS ROAD,, NEW DELHI - W 1089859. 1967141. 3057000.96 110001 84 12 SELVEL MEDIA SERVICES LTD, EXTEN, 6 PAK. HOUSE,TILAK MG.SECURITY PERSON OUT, SIDE,, NEW DELHI - W 1061081. 1408632. 2469713.57 110001 14 43 THE GENERAL MANAGER DELHI SIKH GURUDWARA MANAGEMENT 7 GURUDWARA BANGLA SAHIB ASHOKA ROAD, NEW DELHI - 110001 W 2075151. 103757.5 2178909.04 47 7 M/S BLUE RAISIN ENTERTAINMENT 8 L 23/7 MIDDLE CIRCLE CONNAUGHT PLACE, NEW DELHI - 110001 E 1794460. 17961.83 1812422.02 19 INDIAN EXPRESS LTD. 9 S.NO 35094,23 CURZAN ROAD, NEW DELHI - 110001 W 782776.5 1005934. 1788711.42 3 89 YOGESHWAR DAYAL 10 72 JANPATH, NEW DELHI - 110001 W 207063.0 1339970. 1547033.96 6 90 B D KAPOOR 11 3-A AURANJZEB LANE, NEW DELHI - 110011 W 845852.3 594294.5 1440146.90 7 3 PREM LATA BANSAL & ANKUR BANSAL 12 F 60 MALHOTRA BUILDING CONNAUGHT PLACE, NEW DELHI - 110001 E 1070272. -
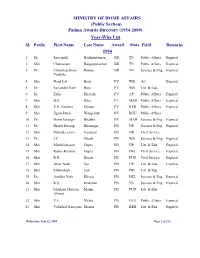
(Public Section) Padma Awards Directory (1954-2009) Year-Wise List Sl
MINISTRY OF HOME AFFAIRS (Public Section) Padma Awards Directory (1954-2009) Year-Wise List Sl. Prefix First Name Last Name Award State Field Remarks 1954 1 Dr. Sarvapalli Radhakrishnan BR TN Public Affairs Expired 2 Shri Chakravarti Rajagopalachari BR TN Public Affairs Expired 3 Dr. Chandrasekhara Raman BR TN Science & Eng. Expired Venkata 4 Shri Nand Lal Bose PV WB Art Expired 5 Dr. Satyendra Nath Bose PV WB Litt. & Edu. 6 Dr. Zakir Hussain PV AP Public Affairs Expired 7 Shri B.G. Kher PV MAH Public Affairs Expired 8 Shri V.K. Krishna Menon PV KER Public Affairs Expired 9 Shri Jigme Dorji Wangchuk PV BHU Public Affairs 10 Dr. Homi Jehangir Bhabha PB MAH Science & Eng. Expired 11 Dr. Shanti Swarup Bhatnagar PB UP Science & Eng. Expired 12 Shri Mahadeva Iyer Ganapati PB OR Civil Service 13 Dr. J.C. Ghosh PB WB Science & Eng. Expired 14 Shri Maithilisharan Gupta PB UP Litt. & Edu. Expired 15 Shri Radha Krishan Gupta PB DEL Civil Service Expired 16 Shri R.R. Handa PB PUN Civil Service Expired 17 Shri Amar Nath Jha PB UP Litt. & Edu. Expired 18 Shri Malihabadi Josh PB DEL Litt. & Edu. 19 Dr. Ajudhia Nath Khosla PB DEL Science & Eng. Expired 20 Shri K.S. Krishnan PB TN Science & Eng. Expired 21 Shri Moulana Hussain Madni PB PUN Litt. & Edu. Ahmed 22 Shri V.L. Mehta PB GUJ Public Affairs Expired 23 Shri Vallathol Narayana Menon PB KER Litt. & Edu. Expired Wednesday, July 22, 2009 Page 1 of 133 Sl. Prefix First Name Last Name Award State Field Remarks 24 Dr. -
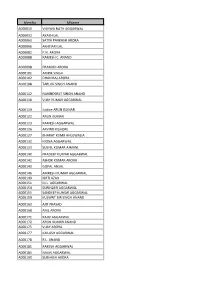
Memno Mname A000010 VISHWA NATH AGGARWAL A000032 AKASH LAL A000063 SATYA PARKASH ARORA A000066 AKHTIARI LAL A000082 P.N
MemNo MName A000010 VISHWA NATH AGGARWAL A000032 AKASH LAL A000063 SATYA PARKASH ARORA A000066 AKHTIARI LAL A000082 P.N. ARORA A000088 RAMESH C. ANAND A000098 PRAMOD ARORA A000101 AMRIK SINGH A000102 DHAN RAJ ARORA A000108 TARLOK SINGH ANAND A000112 NARINDERJIT SINGH ANAND A000118 VIJAY KUMAR AGGARWAL A000119 Justice ARUN KUMAR A000122 ARUN KUMAR A000123 RAMESH AGGARWAL A000126 ARVIND KISHORE A000127 BHARAT KUMR AHLUWALIA A000132 MONA AGGARWAL A000133 SUSHIL KUMAR AJMANI A000140 PRADEEP KUMAR AGGARWAL A000142 ASHOK KUMAR ARORA A000143 GOPAL ANSAL A000146 AMRESH KUMAR AGGARWAL A000149 KIRTI AZAD A000151 M.L. AGGARWAL A000154 SURINDER AGGARWAL A000155 SANDEEP KUMAR AGGARWAL A000159 KULWNT BIR SINGH ANAND A000163 AJIT PRASAD A000168 ANIL ARORA A000171 RAJIV AGGARWAL A000172 ARUN KUMAR ANAND A000175 VIJAY ARORA A000177 KAILASH AGGARWAL A000178 R.L. ANAND A000181 RAKESH AGGARWAL A000185 NALIN AGGARWAL A000190 SUBHASH ARORA A000192 A.K. DEV A000193 LALIT AHLUWALIA A000194 S.K. ARORA A000196 SUDHIR ARORA A000197 ASHOK KUMAR AHLUWALIA A000203 RAKESH ARORA A000204 SANTOSH AULUCK A000205 VINAY KUMAR ARORA A000207 AJIT SINGH A000211 ASHOK KUMAR A000212 L.M. AGGARWAL A000214 MADAN MOHAN AGGARWAL A000218 ASHOK ANAND A000223 JANAK RAJ ARORA A000226 DINESH AGNANI A000227 M.K. ARORA A000230 ASHOK KUMAR A000231 D.K. AGGARWAL A000236 RAM AVTAR AGGARWAL A000244 NAVEEN ANAND A000245 PARVEEN ANAND A000247 MADAN LAL ANAND A000250 JASPAl. S. ARORA A000251 ARVINDER SING ARORA A000253 MANJIT SINGH ARORA A000254 RAJPAL SINGH ARORA A000257 TRILOK NATH ANAND A000258 -

Alphabetical List of Recommendations Received for Padma Awards - 2014
Alphabetical List of recommendations received for Padma Awards - 2014 Sl. No. Name Recommending Authority 1. Shri Manoj Tibrewal Aakash Shri Sriprakash Jaiswal, Minister of Coal, Govt. of India. 2. Dr. (Smt.) Durga Pathak Aarti 1.Dr. Raman Singh, Chief Minister, Govt. of Chhattisgarh. 2.Shri Madhusudan Yadav, MP, Lok Sabha. 3.Shri Motilal Vora, MP, Rajya Sabha. 4.Shri Nand Kumar Saay, MP, Rajya Sabha. 5.Shri Nirmal Kumar Richhariya, Raipur, Chhattisgarh. 6.Shri N.K. Richarya, Chhattisgarh. 3. Dr. Naheed Abidi Dr. Karan Singh, MP, Rajya Sabha & Padma Vibhushan awardee. 4. Dr. Thomas Abraham Shri Inder Singh, Chairman, Global Organization of People Indian Origin, USA. 5. Dr. Yash Pal Abrol Prof. M.S. Swaminathan, Padma Vibhushan awardee. 6. Shri S.K. Acharigi Self 7. Dr. Subrat Kumar Acharya Padma Award Committee. 8. Shri Achintya Kumar Acharya Self 9. Dr. Hariram Acharya Government of Rajasthan. 10. Guru Shashadhar Acharya Ministry of Culture, Govt. of India. 11. Shri Somnath Adhikary Self 12. Dr. Sunkara Venkata Adinarayana Rao Shri Ganta Srinivasa Rao, Minister for Infrastructure & Investments, Ports, Airporst & Natural Gas, Govt. of Andhra Pradesh. 13. Prof. S.H. Advani Dr. S.K. Rana, Consultant Cardiologist & Physician, Kolkata. 14. Shri Vikas Agarwal Self 15. Prof. Amar Agarwal Shri M. Anandan, MP, Lok Sabha. 16. Shri Apoorv Agarwal 1.Shri Praveen Singh Aron, MP, Lok Sabha. 2.Dr. Arun Kumar Saxena, MLA, Uttar Pradesh. 17. Shri Uttam Prakash Agarwal Dr. Deepak K. Tempe, Dean, Maulana Azad Medical College. 18. Dr. Shekhar Agarwal 1.Dr. Ashok Kumar Walia, Minister of Health & Family Welfare, Higher Education & TTE, Skill Mission/Labour, Irrigation & Floods Control, Govt. -

International Coronary Congress 2016
INTERNATIONAL CORONARY Medanta Institute of Education and Research CONGRESS presents 2016 November 11 - 13, 2016 Hotel Taj Palace New Delhi, India State of the Art Course of Coronary Revascularization in association with IACTS & APSIC Indian Association of Asian Pacific Society of Cardiovascular-Thoracic Surgeons Interventional Cardiolog First ever Heart Team Congress on Coronary Revascularization Scientific Programme rge DIC Su on ME AL of s C o A O e f N U g E A e N l d Y l C i R o 11.5 CPD n 20 Credit I A L b C u H l r a Point HOURS g y h o R RCS CPD points are recognised the world over, including in the US and Europe The possibilities are endless when a cardiologist and a cardiac surgeon come together to treat Coronary Artery Disease A world with the purest of meritocracies of Coronary Artery Disease Invitation International Coronary Congress 2016 Dear Friends & Colleagues, It is my privilege to welcome you to the International Coronary Congress 2016, New Delhi, India . AT ICC 2016 we are determined to make the first of its kind comprehensive course on coronary artery disease Dr. Naresh Trehan management where the platform is shared by most eminent cardiac surgeons and cardiologists from the world to give you a complete overview and meet all your unmet needs. The time has come when we have to introspect, leave the controversies and egos behind, and changes our mindset of individualistic approach of coronary artery disease management to more consensus -based approaches. In the light of evidences from recent trials its proved that HEART TEAM is the way forward in the management of cardiovascular diseases be it coronary artery disease or structural heart disease. -

National Affairs
NATIONAL AFFAIRS Prithvi II Missile Successfully Testifi ed India on November 19, 2006 successfully test-fi red the nuclear-capsule airforce version of the surface-to- surface Prithvi II missile from a defence base in Orissa. It is designed for battlefi eld use agaisnt troops or armoured formations. India-China Relations China’s President Hu Jintao arrived in India on November 20, 2006 on a fourday visit that was aimed at consolidating trade and bilateral cooperation as well as ending years of mistrust between the two Asian giants. Hu, the fi rst Chinese head of state to visit India in more than a decade, was received at the airport in New Delhi by India’s Foreign Minister Pranab Mukherjee and Science and Technology Minister Kapil Sibal. The Chinese leader held talks with Indian Prime Minister Manmohan Singh in Delhi on a range of bilateral issues, including commercial and economic cooperation. The two also reviewed progress in resolving the protracted border dispute between the two countries. After the summit, India and China signed various pacts in areas such as trade, economics, health and education and added “more substance” to their strategic partnership in the context of the evolving global order. India and China signed as many as 13 bilateral agreements in the presence of visiting Chinese President Hu Jintao and Prime Minister Manmohan Singh. The fi rst three were signed by External Affairs Minister Pranab Mukherjee and Chinese Foreign Minister Li Zhaoxing. They are: (1) Protocol on the establishment of Consulates-General at Guangzhou and Kolkata. It provides for an Indian Consulate- General in Guangzhou with its consular district covering seven Chinese provinces of Guangdong, Fujian, Hunan, Hainan, Yunnan, Sichuan and Guangxi Zhuang autonomous region. -

A NNUAL R EPORT 2001–2002 Tata Institute of Social Sciences
A NNUAL R EPORT 2001–2002 Tata Institute of Social Sciences Deonar, Mumbai 400 088, India May 3, 2002 Contents Director’s Report 1 SECTION 1 : Main Campus Appendix 1 : Geographical Distribution of Students, 2000–2001 23 Appendix 2 : Field Work Agencies/ Internships and Supervisors 24 Appendix 3 : M.Phil./ Ph.D. Seminars 33 Appendix 4 : Research Projects and Other Projects 34 Appendix 5 : Field Action Projects 44 Appendix 6 : Publications by the Faculty 49 Appendix 7 : Conferences, Seminars, Workshops and Training Programmes 55 Organised by the Faculty Appendix 8 : Faculty Participation in Conferences, Seminars, Workshops and 65 Training Programmes Appendix 9 : Participation of Administrative Staff in Conferences, Seminars, 99 Workshops and Training Programmes Appendix 10 : Talks/ Lectures Delivered by the Faculty 101 Appendix 11 : Executive Committee Memberships and Positions Held by Faculty in 125 Academic, Government and Non-Government Organisations Appendix 12 : Students’ Union 131 Appendix 13 : TISS Committees 132 Appendix 14 : New Appointments 136 Appendix 15 : Special Visitors 137 Appendix 16 : Financial Statement 141 Appendix 17 : Candidates for the Sixty-Second Convocation 142 Appendix 18 : Prizes 144 SECTION 2 : Rural Campus Appendix 1 : Research Projects and Other Projects 146 Appendix 2 : Field Action Projects 147 Appendix 3 : Publications 149 Appendix 4 : Conferences, Seminars, Workshops and Training Programmes 150 Organised Appendix 5 : Participation in Conferences, Seminars, Workshops and Training 152 Programmes Appendix 6 : Talks/ Lectures Delivered 154 Appendix 7 : Executive Committee Memberships and Positions Held by Faculty in 154 Academic, Government and Non-Government Organisations Director’s Report Chairman, Shri B.G. Deshmukh, Honourable Chief Guest, Dr. R.A. -

Enriching Public Health Through Ayurveda’ 7–10 December 2012, Bhopal, Madhya Pradesh, India
2nd announcement Organizers Partner State Govt of Madhya Pradesh Govt of Chhattisgarh Focal theme ‘Enriching Public Health Through Ayurveda’ 7–10 December 2012, Bhopal, Madhya Pradesh, India Partners Prime Sponsor PHARMACEUTICALS EXPORT PROMOTION COUNCIL Ministry of Commerce & Industry AVS, Kottakkal AVP, Coimbatore Government of India CHIEF PATRONS NATIONAL AdvISORY BOARD Secretary, AROGYA Expo– Dr Tanuja Gokhale, Pune Shri Ghulam Nabi Azad Members Co-ordinator – Dr Tushar Mandlik, Bhopal Hon’ble Minister for H & FW, Govt of India Dr T Ramasami, Secretary, Department of Science and Shri Shivraj Singh Chauhan Technology, Government of India International Delegates’ ASSEMBly(IDA) Hon’ble Chief Minister, Govt of Madhya Pradesh Dr S Ayyappan, Secretary, Department of Agriculture Chair – Dr K Anil Kumar, Bengaluru Shri Sudip Bandyopadhyay Education, Government of India and Director General, Co-Chairs – Dr Antonio Morandi, Italy, Hon’ble Minister of State, H & FW, Govt of India Indian Council of Agricultural Research Ms Pratichi Mathur, USA, Dr George Berra, Argentina Shri S Gandhiselvan Shri Rajiv Kher, Additional Secretary, Department of Secretary – Dr Rajesh Kotecha, Jaipur Hon’ble Minister of State, H & FW, Govt of India Commerce, Government of India Convener – Dr Tanuja Gokhale, Pune Shri Raman Singh Prof K I Vasu, Founder-President, Vijnana Bharati Students’ Programme Hon’ble Chief Minister, Govt of Chhattisgarh Dr H R Nagendra, Vice Chancellor, S-VYASA, Bengaluru Chair – Dr B R Ramakrishna, Principal, Sushrutha Ayurveda Dr Naresh Trehan, -

E-Mail : [email protected] Website
022-24132735 022-24132393 Fax No.022-24123322 022-24172288 022-24156392 भारत सरकार E-mail : [email protected] वाणय और उयोग मंालय Website: http://ipindia.nic.in Patents/Designs/Trademark कायालय महानयंक एकव अभकप एव ं यापार चह Geographical Indications बौक संपदा भवन, एस.एम. रोड, एटॉप हल, मुंबई 400037 GOVERNMENT OF INDIA Ministry of Commerce & Industries Office of the Controller General Patents, Designs and Trademarks Boudhik Sampada Bhawan, S. M. Road, Antop Hill, Mumbai 400037 CG/Public Notice/TMR/ Date: 11/07/2016 Public Notice regarding default in filing of reply in respect of office objection raised in Examination report: During the month of March and April 2016, the Trade Mark Registry has dispatched 13062 examination reports containing office objections u/s 9, 11 and other relevant sections of the Trade Marks Act, 1999 to the concerned applicants or their authorised agents on record. Out of the examination reports so dispatched, no reply / communication have been received in 9578 applications even after the expiry of more than 30 days from the date of dispatch. The list of such applications is attached herewith for reference. It is to be noted that examination reports are also made available on official web site of the CGPDTM i.e. www.ipindia.nic.in along with the application status of the relevant application. As per provisions of the Trade Marks Act, 1999 and rules made their under, such applications are likely to be treated as abandoned. Applicants / authorised agents may however send the scanned copy of reply to the examination report on or before 31/07/2016 at [email protected], failing which the applications may be treated as abandoned. -

Pravasi Bharatiya Divas 2003
Pravasi Bharatiya Divas 2003 Sl. No. Session Topic Speakers 1. Plenary India and the Diaspora – Dr. L. M. Singhvi Rajya Sabha MP and Chairman, India Session I Forging a Constructive Organizing Committee of PBD Relationship Mr. Yashwant SInha EAM India Sir Shridath Ramphal Secretariat General UK Prof. Lord Bhikhu Parekh UK H.E. Dato’ Seri S Samy Minister of Works Malaysia Vellu Mr. Mewa Ramgobin MP South Africa Mr. Mahendra P. Former Prime Minister Fiji Chaudhry Mr. Ernest Moutoussamy M.P. Guadeloupe Mr. B.K. Agnihotri Ambassador-at-Large for NRIs & PIOs USA Mr. Ujjal Dosanjh Former Premier of British Columbia Canada Prof. Amartya Sen Mr. Rajat Gupta CEO USA Prof. C.K. Prahalad USA Justice A.M. Ebrahim Retired Supreme Court Judge Zimbabwe Ms. Fatima Meer Director South Africa Prof. Dipak C. Jain Dean USA Prof. Devesh Kapur Associate Professor USA Mr. Bharatkumar J. Shah Chairman Dubai Mr. Dhundev Bauhadoor GOPIO Mauritius Mr. Thomas Abraham 2. Plenary Science and Technology Dr. L.M. Singhvi Rajya Sabha MP and Chairman, India Session II in India – Networking for Organizing Committee of PBD Excellence” Mr. S.K. Tripathi Education Secretary India Dr. Murli Manohar Joshi Minister of Human Resource India Development, Science & Technology and Ocean Development Prof. E.C. George University of Texas USA Sudarshan 1 Dr. R. Chidambaram Principal Scientific Adviser India 3. Plenary The Global Business Mr. Y.K. Modi Senior Vice President FICCI Session III Matrix and the Indian Dr. Manu Chandaria Kenya Diaspora Mr. Jaswant Singh Minister of Finance and Company India Affairs Mr. Rahul Bajaj CMD, Bajaj Auto Ltd. -

The Medicity: a New Concept in Medical and Health Care
TTHHEE MMEEDDIICCIITTYY THE MEDICITY: A NEW CONCEPT IN MEDICAL AND HEALTH CARE Medicity, one of India’s largest projects in multi-specialty tertiary care medical treatment is envisioned as an institute that will redefine standards of excellence in healthcare delivery by bringing together the best of infrastructure, technology, training, education and medical intelligentsia. With an investment of over $350 million, Medicity aims to create a world-class education and training centre backed by remarkable infrastructure, futuristic technology and extraordinary vision of eminent cardiac surgeon, Dr Naresh Trehan – Chairman and Managing Director of Global Health Private Limited. Located across 43 acres in the new international business-destination in the National Capital Region of New Delhi - Gurgaon, Medicity is a 1600 bed medical institute of world standards. The objective of Medicity is to bring in global healthcare delivery standards at affordable prices while firmly placing India on the international roadmap as premier destination for healthcare services, medical research and high-end medical diagnostics. Besides offering the best of preventive and curative medicine, Medicity also offers to explore integrating the knowledge of traditional and alternative medicine with modern medicine, through means of scientific research. SPECIALITIES COVERED Medicity will provide integrated primary, secondary and tertiary care services spanning over 20 super- specialties and high-end services in: • Cardiology and cardiovascular surgery • Oncology (including