LASIK) for Myopia in Same-Eye Virtual Trials
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

History of Refractive Surgery
History of Refractive Surgery Refractive surgery corrects common vision problems by reshaping the cornea, the eye’s outermost layer, to bend light rays to focus on the retina, reducing an individual’s dependence on eye glasses or contact lenses.1 LASIK, or laser-assisted in situ keratomileusis, is the most commonly performed refractive surgery to treat myopia, hyperopia and astigmatism.1 The first refractive surgeries were said to be the removal of cataracts – the clouding of the lens in the eye – in ancient Greece.2 1850s The first lensectomy is performed to remove the lens 1996 Clinical trials for LASIK begin and are approved by the of the eye to correct myopia.2 Food & Drug Administration (FDA).3 Late 19th 2 Abott Medical Optics receives FDA approval for the first Century The first surgery to correct astigmatism takes place. 2001 femtosecond laser, the IntraLase® FS Laser.3 The laser is used to create a circular, hinged flap in the cornea, which allows the surgeon access to the tissue affecting the eye’s 1978 Radial Keratotomy is introduced by Svyatoslov Fyodorov shape.1 in the U.S. The procedure involves making a number of incisions in the cornea to change its shape and 2002 The STAR S4 IR® Laser is introduced. The X generation is correct refractive errors, such as myopia, hyperopia used in LASIK procedures today.4 and astigmatism.2,3 1970s Samuel Blum, Rangaswamy Srinivasan and James J. Wynne 2003 The FDA approves the use of wavefront technology,3 invent the excimer laser at the IBM Thomas J. Watson which creates a 3-D map of the eye to measure 1980s Research Center in Yorktown, New York. -

Ocular Surface Changes Associated with Ophthalmic Surgery
Journal of Clinical Medicine Review Ocular Surface Changes Associated with Ophthalmic Surgery Lina Mikalauskiene 1, Andrzej Grzybowski 2,3 and Reda Zemaitiene 1,* 1 Department of Ophthalmology, Medical Academy, Lithuanian University of Health Sciences, 44037 Kaunas, Lithuania; [email protected] 2 Department of Ophthalmology, University of Warmia and Mazury, 10719 Olsztyn, Poland; [email protected] 3 Institute for Research in Ophthalmology, Foundation for Ophthalmology Development, 61553 Poznan, Poland * Correspondence: [email protected] Abstract: Dry eye disease causes ocular discomfort and visual disturbances. Older adults are at a higher risk of developing dry eye disease as well as needing for ophthalmic surgery. Anterior segment surgery may induce or worsen existing dry eye symptoms usually for a short-term period. Despite good visual outcomes, ocular surface dysfunction can significantly affect quality of life and, therefore, lower a patient’s satisfaction with ophthalmic surgery. Preoperative dry eye disease, factors during surgery and postoperative treatment may all contribute to ocular surface dysfunction and its severity. We reviewed relevant articles from 2010 through to 2021 using keywords “cataract surgery”, ”phacoemulsification”, ”refractive surgery”, ”trabeculectomy”, ”vitrectomy” in combina- tion with ”ocular surface dysfunction”, “dry eye disease”, and analyzed studies on dry eye disease pathophysiology and the impact of anterior segment surgery on the ocular surface. Keywords: dry eye disease; ocular surface dysfunction; cataract surgery; phacoemulsification; refractive surgery; trabeculectomy; vitrectomy Citation: Mikalauskiene, L.; Grzybowski, A.; Zemaitiene, R. Ocular Surface Changes Associated with Ophthalmic Surgery. J. Clin. 1. Introduction Med. 2021, 10, 1642. https://doi.org/ 10.3390/jcm10081642 Dry eye disease (DED) is a common condition, which usually causes discomfort, but it can also be an origin of ocular pain and visual disturbances. -

Refractive Surgery Faqs. Refractive Surgery the OD's Role in Refractive
9/18/2013 Refractive Surgery Refractive Surgery FAQs. Help your doctor with refractive surgery patient education Corneal Intraocular Bill Tullo, OD, FAAO, LASIK Phakic IOL Verisys Diplomate Surface Ablation Vice-President of Visian PRK Clinical Services LASEK CLE – Clear Lens Extraction TLC Laser Eye Centers Epi-LASIK Cataract Surgery AK - Femto Toric IOL Multifocal IOL ICRS - Intacs Accommodative IOL Femtosecond Assisted Inlays Kamra The OD’s role in Refractive Surgery Refractive Error Determine the patient’s interest Myopia Make the patient aware of your ability to co-manage surgery Astigmatism Discuss advancements in the field Hyperopia Outline expectations Presbyopia/monovision Presbyopia Enhancements Risks Make a recommendation Manage post-op care and expectations Myopia Myopic Astigmatism FDA Approval Common Use FDA Approval Common Use LASIK: 1D – 14D LASIK: 1D – 8D LASIK: -0.25D – -6D LASIK: -0.25D – -3.50D PRK: 1D – 13D PRK: 1D – 6D PRK: -0.25D – -6D PRK: -0.25D – -3.50D Intacs: 1D- 3D Intacs: 1D- 3D Intacs NONE Intacs: NONE P-IOL: 3D- 20D P-IOL: 8D- 20D P-IOL: NONE P-IOL: NONE CLE/CAT: any CLE/CAT: any CLE/CAT: -0.75D - -3D CLE/CAT: -0.75D - -3D 1 9/18/2013 Hyperopia Hyperopic Astigmatism FDA Approval Common Use FDA Approval Common Use LASIK: 0.25D – 6D LASIK: 0.25D – 4D LASIK: 0.25D – 6D LASIK: 0.25D – 4D PRK: 0.25D – 6D PRK: 0.25D – 4D PRK: 0.25D – 6D PRK: 0.25D – 4D Intacs: NONE Intacs: NONE Intacs: NONE Intacs: NONE P-IOL: NONE P-IOL: NONE P-IOL: NONE P-IOL: -
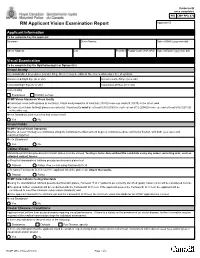
RCMP GRC 2180E (2017-10) Page 1 of 2 Protected B RM Applicant Vision Examination Report Once Completed Applicant ID
Protected B once completed PIB CMP PPU 070 RM Applicant Vision Examination Report Applicant ID Applicant Information To be completed by the applicant Surname Given Names Date of Birth (yyyy-mm-dd) Street Address City Province Postal Code (A9A 9A9) Date of Exam (yyyy-mm-dd) Visual Examination To be completed by the Ophthalmologist or Optometrist Visual Acuity Any standardized procedures (Landoit Ring, Snellen) may be utilized. No error is allowed per line of symbols. Uncorrected Right Eye (6/ or 20/) Uncorrected Left Eye (6/ or 20/) Corrected Right Eye (6/ or 20/) Corrected Left Eye (6/ or 20/) Corrected by Eyeglasses Contact Lenses RCMP Vision Standards Visual Acuity Corrected vision (with glasses or contacts): Visual acuity must be at least 6/6 (20/20) in one eye and 6/9 (20/30) in the other; and Uncorrected vision (without glasses or contacts): Visual acuity must be at least 6/18 (20/60) in each eye or 6/12 (20/40) in one eye and at least 6/30 (20/100) in the other eye. Meets Standards, both corrected and uncorrected? Yes No Visual Fields RCMP Field of Vision Standards Must be at least 150 degrees continuous along the horizontal meridian and 20 degrees continuous above and below fixation, with both eyes open and examined together. Meets Standards? Yes No Colour-Vision Standardized Ishihara pseudo-isochromatic plates must be utilized. Testing is to be done without the candidate using any colour correcting aids, such as coloured contact lenses. a) Result of standardized Ishihara pseudo-isochromatic plates test Passed Failed. If so, re-test using Farnsworth D-15. -

Modern Laser in Situ Keratomileusis Outcomes
REVIEW/UPDATE Modern laser in situ keratomileusis outcomes Helga P. Sandoval, MD, MSCR, Eric D. Donnenfeld, MD, Thomas Kohnen, MD, PhD, FEBO, Richard L. Lindstrom, MD, Richard Potvin, OD, David M. Tremblay, MD, Kerry D. Solomon, MD Laser in situ keratomileusis (LASIK) articles published between 2008 and 2015 that contain clin- ical outcomes data were reviewed and graded for quality, impression, and potential bias. All 97 relevant articles (representing 67 893 eyes) provided a positive or neutral impression of LASIK. Industry bias was not evident. The aggregate loss of 2 or more lines of corrected distance visual acuity was 0.61% (359/58 653). The overall percentage of eyes with uncorrected distance visual acuity better than 20/40 was 99.5% (59 503/59 825). The spherical equivalent refraction was within G1.0 diopter (D) of the target refraction in 98.6% (59 476/60 329) of eyes, with 90.9% (59 954/65 974) within G0.5 D. In studies reporting patient satisfaction, 1.2% (129/9726) of pa- tients were dissatisfied with LASIK. Aggregate outcomes appear better than those reported in summaries of the safety and effectiveness of earlier laser refractive surgery systems approved by the U.S. Food and Drug Administration. Modern results support the safety, efficacy, and patient satisfaction of the procedure. Financial Disclosure: Proprietary or commercial disclosures are listed after the references. J Cataract Refract Surg 2016; 42:1224–1234 Q 2016 ASCRS and ESCRS Laser in situ keratomileusis (LASIK) is one of the most have been performed globally.1 Laser in situ keratomil- commonly performed elective procedures in the United eusis was introduced by Pallikaris et al.2 in 1990. -

Laser Vision Correction Surgery
Patient Information Laser Vision Correction 1 Contents What is Laser Vision Correction? 3 What are the benefits? 3 Who is suitable for laser vision correction? 4 What are the alternatives? 5 Vision correction surgery alternatives 5 Alternative laser procedures 5 Continuing in glasses or contact lenses 5 How is Laser Vision Correction performed? 6 LASIK 6 Surface laser treatments 6 SMILE 6 What are the risks? 7 Loss of vision 7 Additional surgery 7 Risks of contact lens wear 7 What are the side effects? 8 Vision 8 Eye comfort 8 Eye Appearance 8 Will laser vision correction affect my future eye health care? 8 How can I reduce the risk of problems? 9 How much does laser vision correction cost? 9 2 What is Laser Vision Correction? Modern surgical lasers are able to alter the curvature and focusing power of the front surface of the eye (the cornea) very accurately to correct short sight (myopia), long sight (hyperopia), and astigmatism. Three types of procedure are commonly used in If you are suitable for laser vision correction, your the UK: LASIK, surface laser treatments (PRK, surgeon will discuss which type of procedure is the LASEK, TransPRK) and SMILE. Risks and benefits are best option for you. similar, and all these procedures normally produce very good results in the right patients. Differences between these laser vision correction procedures are explained below. What are the benefits? For most patients, vision after laser correction is similar to vision in contact lenses before surgery, without the potential discomfort and limitations on activity. Glasses may still be required for some activities after Short sight and astigmatism normally stabilize in treatment, particularly for reading in older patients. -

Early Postoperative Rotational Stability and Its Related Factors of a Single-Piece Acrylic Toric Intraocular Lens
Eye (2020) 34:474–479 https://doi.org/10.1038/s41433-019-0521-0 ARTICLE Early Postoperative Rotational stability and its related factors of a single-piece acrylic toric intraocular lens 1,2 3 4 5 1 1 1 Shuyi Li ● Xi Li ● Suhong He ● Qianyin Zheng ● Xiang Chen ● Xingdi Wu ● Wen Xu Received: 30 November 2018 / Accepted: 18 June 2019 / Published online: 12 July 2019 © The Author(s) 2019. This article is published with open access Abstract Purpose In the present study, we aimed to evaluate the early postoperative rotational stability of TECNIS toric intraocular lens (IOL) and analyse its correlation with preoperative and intraoperative parameters. Methods A total of 102 eyes from 87 cataract patients who underwent implantation of TECNIS toric IOL during July 2016 to November 2017 were enrolled in this retrospective study. Preoperative parameters including corneal astigmatism, axial length (AL), lens thickness (LT), anterior chamber depth (ACD) and sulcus-to-sulcus (STS), were determined. The area of capsulorhexis was measured with Rhinoceros 5.0 software. The follow-up examinations including the residual astigmatism (RAS) and postoperative toric IOL axis, were performed at 1 month and 3 months after surgery. − − 1234567890();,: 1234567890();,: Results RAS was 0.84 ± 0.88 D at 1 month and 0.81 ± 0.89 D at 3 months after surgery. The rotation of toric IOL at 3 months was 4.83 ± 3.65°. The Pearson’s r of ACD, horizontal and vertical STS, and toric IOL target axis was 0.011, 0.039, 0.045 and 0.082. The toric IOL rotation was positively correlated with the area of capsulorhexis (r = 0.522, P = 0.0003), LT (r = 0.288, P = 0.003) and AL (r = 0.259, P = 0.009). -

Ophthalmology Abbreviations Alphabetical
COMMON OPHTHALMOLOGY ABBREVIATIONS Listed as one of America’s Illinois Eye and Ear Infi rmary Best Hospitals for Ophthalmology UIC Department of Ophthalmology & Visual Sciences by U.S.News & World Report Commonly Used Ophthalmology Abbreviations Alphabetical A POCKET GUIDE FOR RESIDENTS Compiled by: Bryan Kim, MD COMMON OPHTHALMOLOGY ABBREVIATIONS A/C or AC anterior chamber Anterior chamber Dilators (red top); A1% atropine 1% education The Department of Ophthalmology accepts six residents Drops/Meds to its program each year, making it one of nation’s largest programs. We are anterior cortical changes/ ACC Lens: Diagnoses/findings also one of the most competitive with well over 600 applicants annually, of cataract whom 84 are granted interviews. Our selection standards are among the Glaucoma: Diagnoses/ highest. Our incoming residents graduated from prestigious medical schools ACG angle closure glaucoma including Brown, Northwestern, MIT, Cornell, University of Michigan, and findings University of Southern California. GPA’s are typically 4.0 and board scores anterior chamber intraocular ACIOL Lens are rarely lower than the 95th percentile. Most applicants have research lens experience. In recent years our residents have gone on to prestigious fellowships at UC Davis, University of Chicago, Northwestern, University amount of plus reading of Iowa, Oregon Health Sciences University, Bascom Palmer, Duke, UCSF, Add power (for bifocal/progres- Refraction Emory, Wilmer Eye Institute, and UCLA. Our tradition of excellence in sives) ophthalmologic education is reflected in the leadership positions held by anterior ischemic optic Nerve/Neuro: Diagno- AION our alumni, who serve as chairs of ophthalmology departments, the dean neuropathy ses/findings of a leading medical school, and the director of the National Eye Institute. -

Presbyopia Treatment by Monocular Peripheral Presbylasik
Presbyopia Treatment by Monocular Peripheral PresbyLASIK Robert Leonard Epstein, MD, MSEE; Mark Andrew Gurgos, COA ABSTRACT spheric corneal LASIK laser ablation to produce a relatively more highly curved central cornea and PURPOSE: To investigate monocular peripheral presby- a relatively fl at midperipheral cornea has been A 1 LASIK on the non-dominant eye with distance-directed termed “central presbyLASIK” by Alió et al, who reported monofocal refractive surgery on the dominant eye in their surgical results using a proprietary ablation profi le with treating presbyopia. 6-month follow-up. Another proprietary central presbyLASIK technique was described and patented by Ruiz2 and indepen- METHODS: One hundred three patients underwent dently tested by Jackson3 in Canada. treatment with a VISX S4 system and follow-up from 1.1 to 3.9 years (mean 27.4 months). Average patient Peripheral presbyLASIK with a relatively fl atter central age was 53.3 years. Preoperative refraction ranged cornea and more highly curved corneal midperiphery was from Ϫ9.75 to ϩ2.75 diopters (D). Non-dominant eyes described by Avalos4 (PARM technique), and a proprietary underwent peripheral presbyLASIK—an aspheric, pupil– peripheral presbyLASIK algorithm was described and patent- size dependent LASIK to induce central corneal relative ed by Tamayo.5 Telandro6 reported 3-month follow-up results fl attening and peripheral corneal relative steepening. Dominant eyes underwent monofocal refraction-based on a different peripheral presbyLASIK algorithm. 7 LASIK (75.8%), wavefront-guided LASIK, limbal relaxing McDonnell et al fi rst described improved visual acuity from incisions, or no treatment to optimize distance vision. a multifocal effect after radial keratotomy. -

Medical Treatment of Operative Corneal Perforation Caused By
CASE REPORTS AND SMALL CASE SERIES and clinical course of a patient with the stromal bed was thin; in the left Medical Treatment a LASIK-induced corneal perfora- eye, the corneal flap was very edema- of Operative Corneal tion that affected the final visual acu- tous and a space was visible between Perforation Caused ity. We believe that this report on the the corneal flap and the stromal bed treatment and recovery of the cor- (Figure 1, left). The anterior cham- by Laser In Situ neal perforation will be valuable in- ber was very shallow, and aqueous Keratomileusis formation for refractive surgeons. humor was observed to leak onto the ocular surface with blinking (Figure Laser in situ keratomileusis (LASIK) Report of a Case. A 33-year-old man 1, right). A round, 0.25-mm diam- is an effective procedure to treat a was referred to us with a complaint eter perforation site was observed in wide range of myopia.1 The advan- of decreased visual acuity in the left the center of the stromal bed by slit- tages of LASIK over photorefrac- eye after bilateral simultaneous lamp examination. tive keratectomy (PRK) are rapid vi- LASIK performed 3 days previ- We treated the corneal perfo- sual recovery, lower risk of corneal ously at a different facility. A cor- ration by applying a therapeutic soft haze, greater regression of myopia, neal perforation was noticed in the contact lens with topical antibiot- and less postoperative pain.1-3 How- left eye during LASIK laser abla- ics, oral carbonic anhydrase inhibi- ever, LASIK requires more skillful tion in this eye. -

Refractive Errors a Closer Look
2011-2012 refractive errors a closer look WHAT ARE REFRACTIVE ERRORS? WHAT ARE THE DIFFERENT TYPES OF REFRACTIVE ERRORS? In order for our eyes to be able to see, light rays must be bent or refracted by the cornea and the lens MYOPIA (NEARSIGHTEDNESS) so they can focus on the retina, the layer of light- sensitive cells lining the back of the eye. A myopic eye is longer than normal or has a cornea that is too steep. As a result, light rays focus in front of The retina receives the picture formed by these light the retina instead of on it. Close objects look clear but rays and sends the image to the brain through the distant objects appear blurred. optic nerve. Myopia is inherited and is often discovered in children A refractive error means that due to its shape, your when they are between ages eight and 12 years old. eye doesn’t refract the light properly, so the image you During the teenage years, when the body grows see is blurred. Although refractive errors are called rapidly, myopia may become worse. Between the eye disorders, they are not diseases. ages of 20 and 40, there is usually little change. If the myopia is mild, it is called low myopia. Severe myopia is known as high myopia. Lens Retina Cornea Lens Retina Cornea Light rays Light is focused onto the retina Light rays Light is focused In a normal eye, the cornea and lens focus light rays on in front of the retina the retina. In myopia, the eye is too long or the cornea is too steep. -

Facts You Need to Know About Laser Assisted in Situ Keratomileusis (LASIK) and Photorefractive Keratectomy (PRK) Surgery
Facts You Need to Know About Laser Assisted In Situ Keratomileusis (LASIK) and Photorefractive Keratectomy (PRK) Surgery Patient Information Booklet LASIK: Nearsighted Patients (0 to -14.0 diopters) with or without -0.5 to -5.0 Diopters of Astigmatism Farsighted Patients (+0.5 to +5.0 diopters) with up to +3.0 Diopters of Refractive Astigmatism Mixed Astigmatism Patients (≤ 6.0 diopters of astigmatism) PRK: Nearsighted Patients (-1.0 to -12.0 diopters) or Nearsighted Patients (0 to -12.0 diopters) with up to -4.0 Diopters of Astigmatism Farsighted Patients (+1.0 to +6.0 diopters) with no more than 1.0 Diopter of Refractive Astigmatism Farsighted Patients (+0.5 to +5.0 diopters) with +0.5 to +4.0 Diopters of Refractive Astigmatism Please read this entire booklet. Discuss its contents with your doctor so that all your questions are answered to your satisfaction. Ask any questions you may have before you agree to the surgery. VISX, Incorporated 3400 Central Expressway Santa Clara, CA 95051-0703 U.S.A. Tel: 408.733.2020 Copyright 2001 by VISX, Incorporated All Rights Reserved VISX® is a registered trademark of VISX, Incorporated. VISX STAR Excimer Laser System™ is a trademark of VISX, Incorporated. Accutane® is a registered trademark of Hoffmann-La Roche Inc. Cordarone® is a registered trademark of Sanofi. Imitrex® is a registered trademark of Glaxo Group Ltd. Table of Contents Introduction . 1 How the Eye Functions . 2 What are PRK and LASIK? . 5 Benefits . 6 Risks . 6 The First Week Following Surgery . 7 The First Two To Six Months Following Surgery .