Genetic Basis of Hypertrophic Cardiomyopathy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Role of Z-Disc Proteins in Myopathy and Cardiomyopathy
International Journal of Molecular Sciences Review The Role of Z-disc Proteins in Myopathy and Cardiomyopathy Kirsty Wadmore 1,†, Amar J. Azad 1,† and Katja Gehmlich 1,2,* 1 Institute of Cardiovascular Sciences, College of Medical and Dental Sciences, University of Birmingham, Birmingham B15 2TT, UK; [email protected] (K.W.); [email protected] (A.J.A.) 2 Division of Cardiovascular Medicine, Radcliffe Department of Medicine and British Heart Foundation Centre of Research Excellence Oxford, University of Oxford, Oxford OX3 9DU, UK * Correspondence: [email protected]; Tel.: +44-121-414-8259 † These authors contributed equally. Abstract: The Z-disc acts as a protein-rich structure to tether thin filament in the contractile units, the sarcomeres, of striated muscle cells. Proteins found in the Z-disc are integral for maintaining the architecture of the sarcomere. They also enable it to function as a (bio-mechanical) signalling hub. Numerous proteins interact in the Z-disc to facilitate force transduction and intracellular signalling in both cardiac and skeletal muscle. This review will focus on six key Z-disc proteins: α-actinin 2, filamin C, myopalladin, myotilin, telethonin and Z-disc alternatively spliced PDZ-motif (ZASP), which have all been linked to myopathies and cardiomyopathies. We will summarise pathogenic variants identified in the six genes coding for these proteins and look at their involvement in myopathy and cardiomyopathy. Listing the Minor Allele Frequency (MAF) of these variants in the Genome Aggregation Database (GnomAD) version 3.1 will help to critically re-evaluate pathogenicity based on variant frequency in normal population cohorts. -

Bioinformatic Analysis of Structure and Function of LIM Domains of Human Zyxin Family Proteins
International Journal of Molecular Sciences Article Bioinformatic Analysis of Structure and Function of LIM Domains of Human Zyxin Family Proteins M. Quadir Siddiqui 1,† , Maulik D. Badmalia 1,† and Trushar R. Patel 1,2,3,* 1 Alberta RNA Research and Training Institute, Department of Chemistry and Biochemistry, University of Lethbridge, 4401 University Drive, Lethbridge, AB T1K 3M4, Canada; [email protected] (M.Q.S.); [email protected] (M.D.B.) 2 Department of Microbiology, Immunology and Infectious Disease, Cumming School of Medicine, University of Calgary, 3330 Hospital Drive, Calgary, AB T2N 4N1, Canada 3 Li Ka Shing Institute of Virology, University of Alberta, Edmonton, AB T6G 2E1, Canada * Correspondence: [email protected] † These authors contributed equally to the work. Abstract: Members of the human Zyxin family are LIM domain-containing proteins that perform critical cellular functions and are indispensable for cellular integrity. Despite their importance, not much is known about their structure, functions, interactions and dynamics. To provide insights into these, we used a set of in-silico tools and databases and analyzed their amino acid sequence, phylogeny, post-translational modifications, structure-dynamics, molecular interactions, and func- tions. Our analysis revealed that zyxin members are ohnologs. Presence of a conserved nuclear export signal composed of LxxLxL/LxxxLxL consensus sequence, as well as a possible nuclear localization signal, suggesting that Zyxin family members may have nuclear and cytoplasmic roles. The molecular modeling and structural analysis indicated that Zyxin family LIM domains share Citation: Siddiqui, M.Q.; Badmalia, similarities with transcriptional regulators and have positively charged electrostatic patches, which M.D.; Patel, T.R. -

Spatiotemporal Single-Cell Analysis Reveals Critical Roles of Mechano-Sensing Genes at the Border Zone in Remodeling After Myocardial Infarction
Spatiotemporal single-cell analysis reveals critical roles of mechano-sensing genes at the border zone in remodeling after myocardial infarction Shintaro Yamada Tokyo University https://orcid.org/0000-0002-3240-358X Toshiyuki Ko The University of Tokyo Satoshi Hatsuse The University of Tokyo Seitaro Nomura The University of Tokyo Bo Zhang The University of Tokyo Zhehao Dai The University of Tokyo https://orcid.org/0000-0002-0363-7563 Shunsuke Inoue The University of Tokyo Masayuki Kubota The University of Tokyo Kosuke Sawami The University of Tokyo Takanobu Yamada The University of Tokyo Tatsuro Sassa The University of Tokyo Mikako Katagiri The University of Tokyo Kanna Fujita The University of Tokyo Manami Katoh The University of Tokyo Masamichi Ito The University of Tokyo Mutsuo Harada Page 1/21 The University of Tokyo Haruhiro Toko The University of Tokyo Norifumi Takeda The University of Tokyo https://orcid.org/0000-0003-4818-3347 Hiroyuki Morita The University of Tokyo Hiroyuki Aburatani The University of Tokyo Issei Komuro ( [email protected] ) The University of Tokyo Graduate School of Medicine Article Keywords: spatiotemporal single-cell analysis, myocardial infarction, left ventricular remodeling. Posted Date: June 22nd, 2021 DOI: https://doi.org/10.21203/rs.3.rs-620498/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Page 2/21 Abstract The left ventricular remodeling after myocardial infarction (MI) causes heart failure, but its underlying mechanisms remain largely unknown. Here, we performed an integrative analysis of spatial transcriptomics and single cell RNA-seq in murine MI model and found that mechanical stress-response genes are expressed at the border zone and play a critical role in left ventricular remodeling after MI. -
Identification of a Variant Hotspot in MYBPC3 and of a Novel CSRP3
ORIGINAL ARTICLE Identification of a variant hotspot inMYBPC3 and of a novel CSRP3 autosomal recessive alteration in a cohort of Polish patients with hypertrophic cardiomyopathy Martina Lipari1, Ewa Wypasek2,3, Marek Karpiński2, Lidia Tomkiewicz ‑Pająk2,4, Luigi Laino1, Francesco Binni1, Diana Giannarelli5, Paweł Rubiś2,4, Paweł Petkow ‑Dimitrow6,7, Anetta Undas2,7, Paola Grammatico1, Irene Bottillo1 1 Division of Medical Genetics, Department of Molecular Medicine, Sapienza University, San Camillo ‑Forlanini Hospital, Rome, Italy 2 John Paul II Hospital, Kraków, Poland 3 Faculty of Medicine and Health Sciences, Andrzej Frycz Modrzewski Krakow University, Kraków, Poland 4 Department of Cardiac Vascular Diseases, Institute of Cardiology, Jagiellonian University Medical College, Kraków, Poland 5 Biostatistical Unit, Regina Elena National Cancer Institute, Istituti di Ricovero e Cura a Carattere Scientifico (IRCCS), Rome, Italy 6 2nd Department of Cardiology, Institute of Cardiology, Jagiellonian University Medical College, Kraków, Poland 7 Institute of Cardiology, Jagiellonian University Medical College, Kraków, Poland KEY WORDS ABSTRACT CSRP3 human KO, INTRODUCTION Hypertrophic cardiomyopathy (HCM) is a heart disorder caused by autosomal dominant hypertrophic alterations affecting both sarcomeric genes and other nonsarcomeric loci in a minority of cases. However, cardiomyopathy, in some patients, the occurrence of the causal pathogenic variant or variants in homozygosity, compound MYBPC3 founder heterozygosity, or double heterozygosity has also been described. Most of the HCM pathogenic variants mutation, Polish are missense and unique, but truncating mutations of the MYBPC3 gene have been reported as founder population pathogenic variants in populations from Finland, France, Japan, Iceland, Italy, and the Netherlands. OBJECTIVES This study aimed to assess the genetic background of HCM in a cohort of Polish patients. -

CSRP3 Antibody Order 021-34695924 [email protected] Support 400-6123-828 50Ul [email protected] 100 Ul √ √ Web
TD12922 CSRP3 Antibody Order 021-34695924 [email protected] Support 400-6123-828 50ul [email protected] 100 uL √ √ Web www.ab-mart.com.cn Description: Positive regulator of myogenesis. Acts as cofactor for myogenic bHLH transcription factors such as MYOD1, and probably MYOG and MYF6. Enhances the DNA-binding activity of the MYOD1:TCF3 isoform E47 complex and may promote formation of a functional MYOD1:TCF3 isoform E47:MEF2A complex involved in myogenesis (By similarity). Plays a crucial and specific role in the organization of cytosolic structures in cardiomyocytes. Could play a role in mechanical stretch sensing. May be a scaffold protein that promotes the assembly of interacting proteins at Z-line structures. It is essential for calcineurin anchorage to the Z line. Required for stress-induced calcineurin-NFAT activation (By similarity). The role in regulation of cytoskeleton dynamics by association with CFL2 is reported conflictingly: Shown to enhance CFL2-mediated F-actin depolymerization dependent on the CSRP3:CFL2 molecular ratio, and also shown to reduce the ability of CLF1 and CFL2 to enhance actin depolymerization. Proposed to contribute to the maintenance of muscle cell integerity through an actin-based mechanism. Can directly bind to actin filaments, cross-link actin filaments into bundles without polarity selectivity and protect them from dilution- and cofilin-mediated depolymerization; the function seems to involve its self-association. In vitro can inhibit PKC/PRKCA activity. Proposed to be involved in cardiac stress signaling by down-regulating excessive PKC/PRKCA signaling (By similarity).May play a role in early sarcomere organization. Overexpression in myotubes negatively regulates myotube differentiation. -
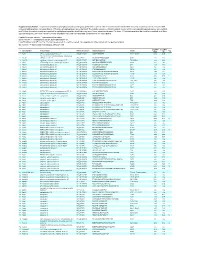
Supplementary Table 1
Supplementary Table 1. Large-scale quantitative phosphoproteomic profiling was performed on paired vehicle- and hormone-treated mTAL-enriched suspensions (n=3). A total of 654 unique phosphopeptides corresponding to 374 unique phosphoproteins were identified. The peptide sequence, phosphorylation site(s), and the corresponding protein name, gene symbol, and RefSeq Accession number are reported for each phosphopeptide identified in any one of three experimental pairs. For those 414 phosphopeptides that could be quantified in all three experimental pairs, the mean Hormone:Vehicle abundance ratio and corresponding standard error are also reported. Peptide Sequence column: * = phosphorylated residue Site(s) column: ^ = ambiguously assigned phosphorylation site Log2(H/V) Mean and SE columns: H = hormone-treated, V = vehicle-treated, n/a = peptide not observable in all 3 experimental pairs Sig. column: * = significantly changed Log 2(H/V), p<0.05 Log (H/V) Log (H/V) # Gene Symbol Protein Name Refseq Accession Peptide Sequence Site(s) 2 2 Sig. Mean SE 1 Aak1 AP2-associated protein kinase 1 NP_001166921 VGSLT*PPSS*PK T622^, S626^ 0.24 0.95 PREDICTED: ATP-binding cassette, sub-family A 2 Abca12 (ABC1), member 12 XP_237242 GLVQVLS*FFSQVQQQR S251^ 1.24 2.13 3 Abcc10 multidrug resistance-associated protein 7 NP_001101671 LMT*ELLS*GIRVLK T464, S468 -2.68 2.48 4 Abcf1 ATP-binding cassette sub-family F member 1 NP_001103353 QLSVPAS*DEEDEVPVPVPR S109 n/a n/a 5 Ablim1 actin-binding LIM protein 1 NP_001037859 PGSSIPGS*PGHTIYAK S51 -3.55 1.81 6 Ablim1 actin-binding -

Human Induced Pluripotent Stem Cell–Derived Podocytes Mature Into Vascularized Glomeruli Upon Experimental Transplantation
BASIC RESEARCH www.jasn.org Human Induced Pluripotent Stem Cell–Derived Podocytes Mature into Vascularized Glomeruli upon Experimental Transplantation † Sazia Sharmin,* Atsuhiro Taguchi,* Yusuke Kaku,* Yasuhiro Yoshimura,* Tomoko Ohmori,* ‡ † ‡ Tetsushi Sakuma, Masashi Mukoyama, Takashi Yamamoto, Hidetake Kurihara,§ and | Ryuichi Nishinakamura* *Department of Kidney Development, Institute of Molecular Embryology and Genetics, and †Department of Nephrology, Faculty of Life Sciences, Kumamoto University, Kumamoto, Japan; ‡Department of Mathematical and Life Sciences, Graduate School of Science, Hiroshima University, Hiroshima, Japan; §Division of Anatomy, Juntendo University School of Medicine, Tokyo, Japan; and |Japan Science and Technology Agency, CREST, Kumamoto, Japan ABSTRACT Glomerular podocytes express proteins, such as nephrin, that constitute the slit diaphragm, thereby contributing to the filtration process in the kidney. Glomerular development has been analyzed mainly in mice, whereas analysis of human kidney development has been minimal because of limited access to embryonic kidneys. We previously reported the induction of three-dimensional primordial glomeruli from human induced pluripotent stem (iPS) cells. Here, using transcription activator–like effector nuclease-mediated homologous recombination, we generated human iPS cell lines that express green fluorescent protein (GFP) in the NPHS1 locus, which encodes nephrin, and we show that GFP expression facilitated accurate visualization of nephrin-positive podocyte formation in -

Spatial and Temporal Aspects of Signalling 6 1
r r r Cell Signalling Biology Michael J. Berridge Module 6 Spatial and Temporal Aspects of Signalling 6 1 Module 6 Spatial and Temporal Aspects of Signalling Synopsis The function and efficiency of cell signalling pathways are very dependent on their organization both in space and time. With regard to spatial organization, signalling components are highly organized with respect to their cellular location and how they transmit information from one region of the cell to another. This spatial organization of signalling pathways depends on the molecular interactions that occur between signalling components that use signal transduction domains to construct signalling pathways. Very often, the components responsible for information transfer mechanisms are held in place by being attached to scaffolding proteins to form macromolecular signalling complexes. Sometimes these macromolecular complexes can be organized further by being localized to specific regions of the cell, as found in lipid rafts and caveolae or in the T-tubule regions of skeletal and cardiac cells. Another feature of the spatial aspects concerns the local Another important temporal aspect is timing and signal and global aspects of signalling. The spatial organization of integration, which relates to the way in which functional signalling molecules mentioned above can lead to highly interactions between signalling pathways are determined localized signalling events, but when the signalling mo- by both the order and the timing of their presentations. lecules are more evenly distributed, signals can spread The organization of signalling systems in both time and more globally throughout the cell. In addition, signals space greatly enhances both their efficiency and versatility. -

Effects of Delayed NSAID Administration After Experimental Eccentric Contraction Injury – a Cellular and Proteomics Study Laura Bond Boise State University
Boise State University ScholarWorks Biology Faculty Publications and Presentations Department of Biological Sciences 2-28-2017 Effects of Delayed NSAID Administration After Experimental Eccentric Contraction Injury – A Cellular and Proteomics Study Laura Bond Boise State University This document was originally published by Public Library of Science (PLOS) in PLOS ONE. This work is provided under a Creative Commons Public Domain 1.0 license. Details regarding the use of this work can be found at: http://creativecommons.org/publicdomain/zero/1.0/. doi: http://dx.doi.org/10.1371/journal.pone.0172486 RESEARCH ARTICLE Effects of delayed NSAID administration after experimental eccentric contraction injury ± A cellular and proteomics study Amy E. Bryant1,2*, Michael J. Aldape1,3, Clifford R. Bayer1, Eva J. Katahira1, Laura Bond4, Carrie D. Nicora5, Thomas L. Fillmore5, Therese R. W. Clauss5, Thomas O. Metz5, Bobbie- Jo Webb-Robertson5, Dennis L. Stevens1,2 1 U.S. Department of Veterans Affairs, Office of Research and Development, Boise, ID, United States of America, 2 University of Washington School of Medicine, Seattle, WA, United States of America, a1111111111 3 Northwest Nazarene University, Nampa, ID, United States of America, 4 Boise State University, Boise, ID, a1111111111 United States of America, 5 Pacific Northwest National Laboratory, Richland, WA, United States of America a1111111111 a1111111111 * [email protected], [email protected] a1111111111 Abstract OPEN ACCESS Background Citation: Bryant AE, Aldape MJ, Bayer CR, Katahira EJ, Bond L, Nicora CD, et al. (2017) Effects of Acute muscle injuries are exceedingly common and non-steroidal anti-inflammatory drugs delayed NSAID administration after experimental (NSAIDs) are widely consumed to reduce the associated inflammation, swelling and pain eccentric contraction injury ± A cellular and that peak 1±2 days post-injury. -

Actin Bundling Via LIM Domains
[Plant Signaling & Behavior 3:5, 320-321; May 2008]; ©2008 Landes Bioscience Article Addendum Actin bundling via LIM domains Clément Thomas,* Monika Dieterle, Sabrina Gatti, Céline Hoffmann, Flora Moreau, Jessica Papuga and André Steinmetz Centre de Recherche Public-Santé; Val Fleuri 84; L-1526; Luxembourg Key words: Actin-binding proteins, actin-bundling, cysteine-rich proteins, cytoskeleton, LIM domain. The LIM domain is defined as a protein-protein interaction module involved in the regulation of diverse cellular processes including gene expression and cytoskeleton organization. We distribute. have recently shown that the tobacco WLIM1, a two LIM domain-containing protein, is able to bind to, stabilize and bundle actin filaments, suggesting that it participates to the regulation of actin cytoskeleton structure and dynamics. In the December issue of the Journal of Biological Chemistry we report a domain analysis not that specifically ascribes the actin-related activities of WLIM1 to its two LIM domains. Results suggest that LIM domains func- Figure 1. Domain maps for wild-type WLIM1 (A) and GFP-fused chimeric tion synergistically in the full-length protein to achieve optimal 3xWLIM1 (B). A. WLIM1 basically comprises a short N-terminal domain (Nt), two LIM domains (LIM1Do and LIM2), an interLIM spacer (IL) and a C-terminal activities. Here we briefly summarize relevant data regarding the domain (Ct). B. 3xWLIM1 consists of three tandem WLIM1 copies. This chi- actin-related properties/functions of two LIM domain-containing meric protein has been fused in C-terminus to GFP and transiently expressed proteins in plants and animals. In addition, we provide further in tobacco BY2 cells. -

Early Evolution of the LIM Homeobox Gene Family
Srivastava et al. BMC Biology 2010, 8:4 http://www.biomedcentral.com/1741-7007/8/4 RESEARCH ARTICLE Open Access Early evolution of the LIM homeobox gene family Mansi Srivastava1*, Claire Larroux2, Daniel R Lu1, Kareshma Mohanty1, Jarrod Chapman3, Bernard M Degnan2, Daniel S Rokhsar1,3 Abstract Background: LIM homeobox (Lhx) transcription factors are unique to the animal lineage and have patterning roles during embryonic development in flies, nematodes and vertebrates, with a conserved role in specifying neuronal identity. Though genes of this family have been reported in a sponge and a cnidarian, the expression patterns and functions of the Lhx family during development in non-bilaterian phyla are not known. Results: We identified Lhx genes in two cnidarians and a placozoan and report the expression of Lhx genes during embryonic development in Nematostella and the demosponge Amphimedon. Members of the six major LIM homeobox subfamilies are represented in the genomes of the starlet sea anemone, Nematostella vectensis, and the placozoan Trichoplax adhaerens. The hydrozoan cnidarian, Hydra magnipapillata, has retained four of the six Lhx subfamilies, but apparently lost two others. Only three subfamilies are represented in the haplosclerid demosponge Amphimedon queenslandica. A tandem cluster of three Lhx genes of different subfamilies and a gene containing two LIM domains in the genome of T. adhaerens (an animal without any neurons) indicates that Lhx subfamilies were generated by tandem duplication. This tandem cluster in Trichoplax is likely a remnant of the original chromosomal context in which Lhx subfamilies first appeared. Three of the six Trichoplax Lhx genes are expressed in animals in laboratory culture, as are all Lhx genes in Hydra. -

Cardiomyopathies: When the Goliaths of Heart Muscle Hurt
Chapter 4 Cardiomyopathies: When the Goliaths of Heart Muscle Hurt Maegen A. Ackermann and Aikaterini Kontrogianni-Konstantopoulos Additional information is available at the end of the chapter http://dx.doi.org/10.5772/55609 1. Introduction Cardiomyopathy, a primary cause of human death, is defined as a disease of the myocardium, which results in insufficient pumping of the heart. It is classified into four major forms; hypertrophic cardiomyopathy (HCM), dilated cardiomyopathy (DCM), restrictive cardiomyopathy (RMC), and arrhythmogenic right ventricular cardiomyop‐ athy (ARVC) [1]. These are characterized by extensive remodeling of the myocardium initially manifested as hypertrophy, evidenced by an increase in the thickness of the left ventricular wall and interventricular septum due to interstitial fibrosis and enlarged myocyte size. Following hypertrophy the heart muscle reverts to a dilated state, characterized by a profound expansion of the intraventricular volume and a modest increase in ventricular wall thickness [2]. These changes, initially compensatory, eventu‐ ally become maladaptive. During the past ~20 years, several mutations in genes encoding sarcomeric proteins have been causally linked to cardiomyopathies [1]. Among the long list of affected proteins are three members of the family of giant sarcomeric proteins of striated muscles: titin, nebulette, a member of the nebulin subfamily, and obscurin, each encoded by single genes namely TTN, NEBL, and OBSCN, respectively [3]-[10]. This chapter will briefly describe the molecular structure of these genes, assisting the reader to excellent de‐ tailed reviews when appropriate, and further provide a comprehensive and up-to-date listing of the mutations that have been identified and directly linked to the develop‐ ment of cardiomyopathy.