Embolization of Bronchial Arteries for the Treatment Of
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Ipsilateral Subclavian Steal in Association with Aberrant Origin of the Left Vertebral Artery from the Aortic Arch
411 Ipsilateral Subclavian Steal in Association with Aberrant Origin of the Left Vertebral Artery from the Aortic Arch John Holder1 Five cases are reported of left subclavian steal syndrome associated with anomalous Eugene F. Binet2 origin of the left vertebral artery from the aortic arch. In all five instances blood flow at Bernard Thompson3 the origin of the left vertebral artery was in an antegrade direction contrary to that usually reported in this condition. The distal subclavian artery was supplied via an extensive collateral network of vessels connecting the vertebral artery to the thyro cervical trunk. If a significant stenosis or occlusion is present within the left subc lavi an artery proximal to the origin of the left vertebral artery, the direction of the bl ood fl ow within the vertebral artery will reverse toward the parent vessel (retrograde flow). This phenomenon occurs when a negative pressure gradient of 20-40 torr exists between the vertebral-basilar artery junction and th e vertebral-subc lavian artery junction [1-3]. We describe five cases of subclavian steal confirmed by angiography where a significant stenosis or occlusion of the left subclavian artery was demonstrated in association with anomalous origin of th e left vertebral artery directly from the aortic arch. In all five cases blood flow at the origin of the left vertebral artery was in an antegrade direction contrary to that more commonly reported in the subclavian steal syndrome. Materials and Methods The five patients were all 44- 58-year-old men. Three sought medical attention for symptoms specificall y related to th e left arm . -
Central Venous Access with Accelerated Seldinger Technique Versus Modified Seldinger Technique
Central Venous Access with Accelerated Seldinger Technique versus Modified Seldinger Technique L A N E THAUT , D O , CAPT , M C , USAF SAN ANTONIO MILITARY MEDICAL CENTER CO- AUTHORS: WELLS WEYMOUTH, MD, DANIEL RESCHKE, MD, BRANDEN HUNSAKER,MD Disclosures Expired POWERWAND™ combination device kits were donated by Access Scientific for the express purpose to be used in this study; however, no other contributions were made. We approached Access Scientific to obtain the devices to conduct this study. No financial relationship with Access Scientific. Background Techniques Research and Outcomes Questions Background Air Force SAMMC San Antonio, TX Level 1 Trauma Center 85,000+ patients annually Central Access Common Procedure Approximately 8% of hospitalized patients Multiple indications Large volume fluid or blood product resuscitation Administration of central acting medications Multiple medications simultaneously Trans venous pacing Difficult peripheral access Quick Story What if there was a simpler/quicker way? Intra-osseous? Complications Slower Flow Rate Labs Traditional Central Line Multiple steps/parts Midlines Usually used for extended dwelling lines. Self contained, all in one device. Equivalent and sometimes superior flow rate. Question Will the use of combination devices (midline/POWERWAND™) and the associated accelerated technique reduce the time of CVC placement? VS What is Accelerated Seldinger Technique? Needle, guidewire, dilator, and sheath into one. The device needle is inserted into the target vein under ultrasound guidance and a flash is observed The internal guidewire is then advanced into the vein and snapped into the needle hub. Dilator collar is turned and the dilator and sheath are advanced The dilator hub is disengaged from the needle hub, and the guidewire, dilator, and needle are all removed as a single unit. -

Practice Parameter for the Use of Ultrasound to Guide Vascular Access Procedures
PRACTICE GUIDELINES AIUM Practice Parameter for the Use of Ultrasound to Guide Vascular Access Procedures I. Introduction he clinical aspects of this parameter were developed collaboratively among the AIUM and other organizations whose members use ultrasound for guidance in vascular T “ ” access procedures (see Acknowledgments ). Recommendations for practitioner requirements, the written request for the examination, procedure documentation, and quality control vary among the organizations and are addressed by each separately. This parameter has been developed by and for clinicians from diverse specialties and practitioner levels who perform vascular access. While vascular access may be performed using external landmarks, point-of-care ultrasound is now increasingly available.1 Appropriately used, ultrasound guidance for vascular access has been shown to improve success rates while reducing iatrogenic injury, the number of needle passes, and infection rates.2 Addition- ally, it may improve patient comfort and satisfaction. This parameter is intended to be evidence based when possi- ble and to include selected references of importance, but it is not meant to be a comprehensive or rigorous literature review, as this has been accomplished elsewhere.3 The intent of this document is to highlight appropriate evidence while also providing a practical, real-world expert consensus from clinicians with diverse back- grounds on the best use and techniques for incorporating ultra- sound into vascular access procedures with the ultimate goal of improving the care of our patients. II. Indications/Contraindications Ultrasound should be used to aid in central venous, peripheral venous, and arterial access procedures.4 When used appropriately by qualified personnel, there are no absolute contraindications to using ultrasound as a procedural adjunct for vascular guidance. -

Too Many Twos in One Patient: Two Central Venous Catheters, Two
& Experim l e ca n i t in a l l C Journal of Clinical and Experimental C f a o r d l i a o Chalwade, J Clin Exp cardiolog 2018, 9:9 n l o r g u y o Cardiology DOI: 10.4172/2155-9880.1000605 J ISSN: 2155-9880 Case Report Open Access Too Many Twos in One Patient: Two Central Venous Catheters, Two Routes, Two Hospitals, Two Lost Guidewires, Two Vascular Systems, One Patient Rahul Chalwade* Department of Cardiology, Felix Health Care, Noida, Uttar Pradesh, India *Corresponding author: Rahul Chalwade, Department of Cardiology, Felix Health Care, Noida, Uttar Pradesh, India, Phone: +919717053558; E-mail: [email protected] Received date: September 05, 2018; Accepted date: September 10, 2018; Published date: September 17, 2018 Copyright: © 2018 Chalwade R. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Abstract Central venous catheter insertion by Seldinger's technique is a very common procedure nowadays. The technique though considered safe, is associated with potential dreaded complications. One such complication is intravascular loss of guidewire during insertion. We describe one unusual case of two chronically lost guidewires in venous and arterial system with successful retrieval by innovative interventional techniques. Keywords: Lost guidewire; Interventional cardiology; Interventionl AORTA-ARCH OF AORTA-LOOPING IN DESCENDING AORTA- radiology; Central venous catheter complications; Anaesthesiology; OPENING OF LT SCA (straight tip of guidewire). Snare We did routine blood evaluation, all were normal, venous and arterial Doppler and echo was done to rule out thrombus. -

The Variations of the Subclavian Artery and Its Branches Ahmet H
Okajimas Folia Anat. Jpn., 76(5): 255-262, December, 1999 The Variations of the Subclavian Artery and Its Branches By Ahmet H. YUCEL, Emine KIZILKANAT and CengizO. OZDEMIR Department of Anatomy, Faculty of Medicine, Cukurova University, 01330 Balcali, Adana Turkey -Received for Publication, June 19,1999- Key Words: Subclavian artery, Vertebral artery, Arterial variation Summary: This study reports important variations in branches of the subclavian artery in a singular cadaver. The origin of the left vertebral artery was from the aortic arch. On the right side, no thyrocervical trunk was found. The two branches which normally originate from the thyrocervical trunk had a different origin. The transverse cervical artery arose directly from the subclavian artery and suprascapular artery originated from the internal thoracic artery. This variation provides a short route for posterior scapular anastomoses. An awareness of this rare variation is important because this area is used for diagnostic and surgical procedures. The subclavian artery, the main artery of the The variations of the subclavian artery and its upper extremity, also gives off the branches which branches have a great importance both in blood supply the neck region. The right subclavian arises vessels surgery and in angiographic investigations. from the brachiocephalic trunk, the left from the aortic arch. Because of this, the first part of the right and left subclavian arteries differs both in the Subjects origin and length. The branches of the subclavian artery are vertebral artery, internal thoracic artery, This work is based on a dissection carried out in thyrocervical trunk, costocervical trunk and dorsal the Department of Anatomy in the Faculty of scapular artery. -

First Simulator for Seldinger Technique and Angiography Training
This is a repository copy of ImaGiNe Seldinger: first simulator for Seldinger Technique and Angiography Training. White Rose Research Online URL for this paper: http://eprints.whiterose.ac.uk/79950/ Version: Accepted Version Article: Luboz, V, Zhang, Y, Johnson, S et al. (20 more authors) (2013) ImaGiNe Seldinger: first simulator for Seldinger Technique and Angiography Training. Computer Methods and Programs in Biomedicine, 111 (2). 419 - 434. ISSN 0169-2607 https://doi.org/10.1016/j.cmpb.2013.05.014 Reuse Unless indicated otherwise, fulltext items are protected by copyright with all rights reserved. The copyright exception in section 29 of the Copyright, Designs and Patents Act 1988 allows the making of a single copy solely for the purpose of non-commercial research or private study within the limits of fair dealing. The publisher or other rights-holder may allow further reproduction and re-use of this version - refer to the White Rose Research Online record for this item. Where records identify the publisher as the copyright holder, users can verify any specific terms of use on the publisher’s website. Takedown If you consider content in White Rose Research Online to be in breach of UK law, please notify us by emailing [email protected] including the URL of the record and the reason for the withdrawal request. [email protected] https://eprints.whiterose.ac.uk/ ImaGiNe Seldinger: first simulator for Seldinger technique and angiography training V. Luboz, Y. Zhang, S. Johnson, Y. Song, C. Kilkenny, C. Hunt, H. Woolnough, S. Guediri, J. Zhai, T. Odetoyinbo, P. Littler, A. -
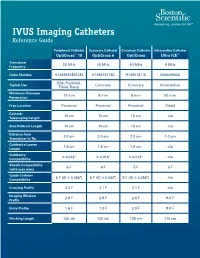
IVUS Imaging Catheters Reference Guide
IVUS Imaging Catheters Reference Guide Peripheral Catheter Coronary Catheter Coronary Catheter Intracardiac Catheter OptiCross™ 18 OptiCross 6 OptiCross Ultra ICE™ Transducer 30 MHz 40 MHz 40 MHz 9 MHz Frequency Order Number H7493932800180 H7495181160 H749518110 M00499000 SFA, Popliteal, Typical Use Coronary Coronary Intracardiac Tibial, Renal Maximum Diameter 12 mm 6 mm 6 mm 50 mm Penetration Prep Location Proximal Proximal Proximal Distal Catheter 15 cm 15 cm 15 cm n/a Telescoping Length Sled Pullback Length 10 cm 10 cm 10 cm n/a Distance from 2.0 cm 2.0 cm 2.0 cm 1.0 cm Transducer to Tip Guidewire Lumen 1.6 cm 1.6 cm 1.6 cm n/a Length Guidewire ≤ 0.018" ≤ 0.014" ≤ 0.014" n/a Compatibility Sheath Compatibility 6 F 6 F 5 F 9 F (with max wire) Guide Catheter 6 F (ID ≥ 0.068") 6 F (ID ≥ 0.064") 5 F (ID ≥ 0.058") n/a Compatibility Crossing Profile 3.5 F 3.1 F 3.1 F n/a Imaging Window 2.9 F 2.9 F 2.6 F 9.0 F Profile Entry Profile 1.6 F 1.3 F 2.0 F 9.0 F Working Length 135 cm 135 cm 135 cm 110 cm OPTICROSS™ 18 CATHETER AND MDU5 PLUS BAG OPTICROSS 6 40 MHZ CORONARY IMAGING CATHETER CAUTION Federal law (USA) restricts this device to sale by or on the order of a physician. Rx only. Prior to use, please see the CAUTION: Federal law (USA) restricts this device to sale by or on the order of a physician. -

Coding Billing
Coding&Billing Quarterly FEBRUARY 2015 EDITOR ALAN L. PLUMMER, MD ATS RUC Advisor Letter from the Editor Welcome to the January 2015 edition of the ATS Coding ADVISORY BOARD MEMBERS: and Billing Quarterly. The New Year will bring a number of KATINA NICOLACAKIS, MD important changes to medicine for practitioners of pulmonary, Chair, ATS Clinical Practice Committee ATS Alternate RUC Advisor critical care and sleep medicine. Below are some issues that ATS STEPHEN P. HOFFMANN, MD members and their staff need to be aware of and prepared for: Member, ATS Clinical Practice Committee ATS CPT Advisor ICD-10 Transition – Barring another last minute intervention MICHAEL NELSON, MD by Congress (which is possible but very unlikely), 2015 will Member, ATS Clinical Practice Committee be the year of the ICD-10 transition. I hope providers and ATS Alternate CPT Advisor practices are well underway preparing for the transition. Over the past year, the STEVE G. PETERS, MD Member, ATS Clinical Practice Committee ATS Coding and Billing Quarterly has featured articles on the transition. The April 2015 edition will cover ICD-10 for pediatric pulmonary services. Lung Cancer Screening Coverage – Earlier this month, the Centers for Medicare In This Issue and Medicaid Services (CMS) released its final coverage policy for lung cancer Low Dose CT Lung Cancer screening. In this issue, Dr. Kovitz describes the final coverage policy, its impact Screening Coverage - Implications on Medicare and private coverage, as well as tips for coding services related to for the Practitioner, page 2 screening. 2015 Brings New Extracorporeal Membrane Oxygenation New ECMO codes – Also covered in this issue is the new and expanded family of (ECMO)/Extracorporeal Life codes for EMCO services. -

Spontaneous Arteriovenous Malformations in the Cervical Area
J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.33.3.303 on 1 June 1970. Downloaded from J. Neurol. Neurosurg. Psychiat., 1970, 33, 303-309 Spontaneous arteriovenous malformations in the cervical area J. GREENBERG, M.D. From the Department of Neurology, Episcopal Hospital, Philadelphia, Pennsylvania 19125, U.S.A. SUMMARY Four patients with spontaneous arteriovenous malformations of cervical vessels have been presented. The embryology of these vessels has been discussed in order to suggest an ex- planation for the apparent difference in the incidence of arteriovenous malformations involving the internal carotid artery and those involving either the vertebral or the external carotid arteries. A fifth case (S.T.) is presented as a probable iatrogenic arteriovenous fistula and is to be added to the steadily growing reports of this phenomenon. Trauma is the most common cause of arteriovenous had sustained a minor injury to the posterior aspect communications between the blood vessels in of the right ear. Routine skull films at the time did not the cervical area (Aronson, 1961). Iatrogenic reveal a fracture, and there was no evidence of local Protected by copyright. deep tissue injury noted. fistulae occurring after carotid or vertebral angio- On the present admission, a slight prominence of the graphy are being reported with regularity in the right retroauricular region was noted and a thrill and recent literature (Sutton, 1962). Spontaneous mal- bruit were present. The bruit could be obliterated by formations in this area also occur. Thus far, eight local pressure. cases have been reported involving the vertebral The neurological examination was within normal vessels (Norman, Schmidt, and Grow, 1950; limits. -

Ascending and Descending Thoracic Vertebral Arteries
CLINICAL REPORT EXTRACRANIAL VASCULAR Ascending and Descending Thoracic Vertebral Arteries X P. Gailloud, X L. Gregg, X M.S. Pearl, and X D. San Millan ABSTRACT SUMMARY: Thoracic vertebral arteries are anastomotic chains similar to cervical vertebral arteries but found at the thoracic level. Descending thoracic vertebral arteries originate from the pretransverse segment of the cervical vertebral artery and curve caudally to pass into the last transverse foramen or the first costotransverse space. Ascending thoracic vertebral arteries originate from the aorta, pass through at least 1 costotransverse space, and continue cranially as the cervical vertebral artery. This report describes the angiographic anatomy and clinical significance of 9 cases of descending and 2 cases of ascending thoracic vertebral arteries. Being located within the upper costotransverse spaces, ascending and descending thoracic vertebral arteries can have important implications during spine inter- ventional or surgical procedures. Because they frequently provide radiculomedullary or bronchial branches, they can also be involved in spinal cord ischemia, supply vascular malformations, or be an elusive source of hemoptysis. ABBREVIATIONS: ISA ϭ intersegmental artery; SIA ϭ supreme intercostal artery; VA ϭ vertebral artery he cervical portion of the vertebral artery (VA) is formed by a bral arteria lusoria8-13 or persistent left seventh cervical ISA of Tseries of anastomoses established between the first 6 cervical aortic origin.14 intersegmental arteries (ISAs) and one of the carotid-vertebral This report discusses 9 angiographic observations of descend- anastomoses, the proatlantal artery.1-3 The VA is labeled a “post- ing thoracic VAs and 2 cases of ascending thoracic VAs. costal” anastomotic chain (ie, located behind the costal process of cervical vertebrae or dorsal to the rib itself at the thoracic level) to CASE SERIES emphasize its location within the transverse foramina. -

The Rare Origin of the Suprascapular Artery Arising Off The
eISSN 1308-4038 International Journal of Anatomical Variations (2011) 4: 182–184 Case Report The rare origin of the suprascapular artery arising off the internal thoracic artery in the presence of the thyrocervical trunk: clinical and surgical implications Published online December 2nd, 2011 © http://www.ijav.org Stavros ATSAS ABSTRACT Jacob N. FOX During routine dissection of the subclavian artery and its branches, the suprascapular artery was found arising from H. Wayne LAMBERT the proximal end of the internal thoracic artery in only the left side of a 68-year-old Caucasian male, despite the presence of the thyrocervical trunk on the ipsilateral side. The suprascapular artery ran deep to the proximal one- third of the clavicle then continued its usual course, running parallel to the suprascapular nerve and passing over the superior transverse scapular ligament distally. Knowledge of this variant origin of the suprascapular artery is clinically Department of Neurobiology and Anatomy, West Virginia University School of Medicine, important because the internal thoracic artery is utilized for a majority of the 800,000 coronary artery bypass surgeries Robert C. Byrd Health Sciences Center, Morgantown, West Virginia, USA. performed worldwide each year. Its course deep to the clavicle is also significant due to clavicular fractures accounting for approximately 5-15% of adult bone fractures. © IJAV. 2011; 4: 182–184. Dr. H. Wayne Lambert, PhD Associate Professor West Virginia University School of Medicine Robert C. Byrd Health Sciences Center Department of Neurobiology and Anatomy HSN 4052; P.O. Box 9128 Morgantown, WV, 26506-9128, USA. +1 304 293-0610 [email protected] Key words [anatomical variant] [suprascapular artery] [internal thoracic artery] [branches of subclavian artery] [thyrocervical trunk] [coronary bypass Received June 21st, 2011; accepted October 12th, 2011 surgery] [radical and modified neck dissections] Introduction In 2005, Weiglein et al. -

An Unusual Origin and Course of the Thyroidea Ima Artery, with Absence of Inferior Thyroid Artery Bilaterally
Surgical and Radiologic Anatomy (2019) 41:235–237 https://doi.org/10.1007/s00276-018-2122-1 ANATOMIC VARIATIONS An unusual origin and course of the thyroidea ima artery, with absence of inferior thyroid artery bilaterally Doris George Yohannan1 · Rajeev Rajan1 · Akhil Bhuvanendran Chandran1 · Renuka Krishnapillai1 Received: 31 May 2018 / Accepted: 21 October 2018 / Published online: 25 October 2018 © Springer-Verlag France SAS, part of Springer Nature 2018 Abstract We report an unusual origin and course of the thyroidea ima artery in a male cadaver. The ima artery originated from the right subclavian artery very close to origin of the right vertebral artery. The artery coursed anteriorly between the common carotid artery medially and internal jugular vein laterally. It then coursed obliquely, from below upwards, from lateral to medial superficial to common carotid artery, to reach the inferior pole of the right lobe of thyroid and branched repeatedly to supply the anteroinferior and posteroinferior aspects of both the thyroid lobes and isthmus. The superior thyroid arteries were normal. Both the inferior thyroid arteries were absent. The unusual feature of this thyroidea ima artery is its origin from the subclavian artery close to vertebral artery origin, the location being remarkably far-off from the usual near midline position, and the oblique and relatively superficial course. This report is a caveat to neck surgeons to consider such a superficially running vessel to be a thyroidea ima artery. Keywords Thyroid vascular anatomy · Thyroidea ima artery · Artery of Neubauer · Blood supply of thyroid · Variations Introduction (1.1%), transverse scapular (1.1%), or pericardiophrenic or thyrocervical trunk [8, 10].