Venous Cutdown Versus the Seldinger Technique for Placement of Totally Implantable Venous Access Ports (Protocol)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Central Venous Access with Accelerated Seldinger Technique Versus Modified Seldinger Technique
Central Venous Access with Accelerated Seldinger Technique versus Modified Seldinger Technique L A N E THAUT , D O , CAPT , M C , USAF SAN ANTONIO MILITARY MEDICAL CENTER CO- AUTHORS: WELLS WEYMOUTH, MD, DANIEL RESCHKE, MD, BRANDEN HUNSAKER,MD Disclosures Expired POWERWAND™ combination device kits were donated by Access Scientific for the express purpose to be used in this study; however, no other contributions were made. We approached Access Scientific to obtain the devices to conduct this study. No financial relationship with Access Scientific. Background Techniques Research and Outcomes Questions Background Air Force SAMMC San Antonio, TX Level 1 Trauma Center 85,000+ patients annually Central Access Common Procedure Approximately 8% of hospitalized patients Multiple indications Large volume fluid or blood product resuscitation Administration of central acting medications Multiple medications simultaneously Trans venous pacing Difficult peripheral access Quick Story What if there was a simpler/quicker way? Intra-osseous? Complications Slower Flow Rate Labs Traditional Central Line Multiple steps/parts Midlines Usually used for extended dwelling lines. Self contained, all in one device. Equivalent and sometimes superior flow rate. Question Will the use of combination devices (midline/POWERWAND™) and the associated accelerated technique reduce the time of CVC placement? VS What is Accelerated Seldinger Technique? Needle, guidewire, dilator, and sheath into one. The device needle is inserted into the target vein under ultrasound guidance and a flash is observed The internal guidewire is then advanced into the vein and snapped into the needle hub. Dilator collar is turned and the dilator and sheath are advanced The dilator hub is disengaged from the needle hub, and the guidewire, dilator, and needle are all removed as a single unit. -

Practice Parameter for the Use of Ultrasound to Guide Vascular Access Procedures
PRACTICE GUIDELINES AIUM Practice Parameter for the Use of Ultrasound to Guide Vascular Access Procedures I. Introduction he clinical aspects of this parameter were developed collaboratively among the AIUM and other organizations whose members use ultrasound for guidance in vascular T “ ” access procedures (see Acknowledgments ). Recommendations for practitioner requirements, the written request for the examination, procedure documentation, and quality control vary among the organizations and are addressed by each separately. This parameter has been developed by and for clinicians from diverse specialties and practitioner levels who perform vascular access. While vascular access may be performed using external landmarks, point-of-care ultrasound is now increasingly available.1 Appropriately used, ultrasound guidance for vascular access has been shown to improve success rates while reducing iatrogenic injury, the number of needle passes, and infection rates.2 Addition- ally, it may improve patient comfort and satisfaction. This parameter is intended to be evidence based when possi- ble and to include selected references of importance, but it is not meant to be a comprehensive or rigorous literature review, as this has been accomplished elsewhere.3 The intent of this document is to highlight appropriate evidence while also providing a practical, real-world expert consensus from clinicians with diverse back- grounds on the best use and techniques for incorporating ultra- sound into vascular access procedures with the ultimate goal of improving the care of our patients. II. Indications/Contraindications Ultrasound should be used to aid in central venous, peripheral venous, and arterial access procedures.4 When used appropriately by qualified personnel, there are no absolute contraindications to using ultrasound as a procedural adjunct for vascular guidance. -

Massive Transfusion and Control of Hemorrhage in the Trauma Patient
Massive Transfusion and Control of Hemorrhage in the Trauma Patient N A L T R A I O U T M A A N R C E A T R N E I I Based on Special ITACCS Seminar Panels. The International Trauma Anesthesia and Critical Care Society (ITACCS) is accredited by the Accreditation Council for Continuing Medical Education (ACCME) for physicians. This CME activity was planned and produced in accordance with the ACCME Essentials. ITACCS designates this CME activity for 15 credit hours in Category 1 of the Physicians Recognition Award of the American Medical Association. I CME QUESTIONS INCLUDED JANUARY 2003 LEARNING OBJECTIVES OF THE MONOGRAPH Chapter 6 Atraumatic blood salvage and autotransfusion in trauma and surgery .................................. Page 17 Sherwin V. Kevy, MD, and Robert Brustowicz, MD, Trans- After completion of this activity, the participant will be able to: fusion Service, Children’s Hospital Department of Anes- thesia, Harvard Medical School, Boston, Massachusetts 1. Evaluate the etiology and pathophysiology of traumatic shock. 2. Describe the management of massive transfusion in the trauma patient. Section III: Transfusion: Clinical Practice 3. Discuss the clinical indications and problems related to the use of blood, blood components, hemostatic agents, oxygen-carrying vol- Chapter 7 Current practices in blood and blood ume expanders, and venous thromboembolism prophylaxis. component therapy ....................................... Page 18 Charles E. Smith, MD, FRCPC, Department of Anesthesi- EDITORS ology, MetroHealth Medical Center, Case Western Reserve University School of Medicine, Cleveland, Ohio Charles E. Smith, MD, FRCPC, Professor of Anesthesiology, Chapter 8 Immunomodulatory effects of transfusion .. Page 22 MetroHealth Medical Center, Case Western Reserve University School David T. -

Too Many Twos in One Patient: Two Central Venous Catheters, Two
& Experim l e ca n i t in a l l C Journal of Clinical and Experimental C f a o r d l i a o Chalwade, J Clin Exp cardiolog 2018, 9:9 n l o r g u y o Cardiology DOI: 10.4172/2155-9880.1000605 J ISSN: 2155-9880 Case Report Open Access Too Many Twos in One Patient: Two Central Venous Catheters, Two Routes, Two Hospitals, Two Lost Guidewires, Two Vascular Systems, One Patient Rahul Chalwade* Department of Cardiology, Felix Health Care, Noida, Uttar Pradesh, India *Corresponding author: Rahul Chalwade, Department of Cardiology, Felix Health Care, Noida, Uttar Pradesh, India, Phone: +919717053558; E-mail: [email protected] Received date: September 05, 2018; Accepted date: September 10, 2018; Published date: September 17, 2018 Copyright: © 2018 Chalwade R. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Abstract Central venous catheter insertion by Seldinger's technique is a very common procedure nowadays. The technique though considered safe, is associated with potential dreaded complications. One such complication is intravascular loss of guidewire during insertion. We describe one unusual case of two chronically lost guidewires in venous and arterial system with successful retrieval by innovative interventional techniques. Keywords: Lost guidewire; Interventional cardiology; Interventionl AORTA-ARCH OF AORTA-LOOPING IN DESCENDING AORTA- radiology; Central venous catheter complications; Anaesthesiology; OPENING OF LT SCA (straight tip of guidewire). Snare We did routine blood evaluation, all were normal, venous and arterial Doppler and echo was done to rule out thrombus. -

First Simulator for Seldinger Technique and Angiography Training
This is a repository copy of ImaGiNe Seldinger: first simulator for Seldinger Technique and Angiography Training. White Rose Research Online URL for this paper: http://eprints.whiterose.ac.uk/79950/ Version: Accepted Version Article: Luboz, V, Zhang, Y, Johnson, S et al. (20 more authors) (2013) ImaGiNe Seldinger: first simulator for Seldinger Technique and Angiography Training. Computer Methods and Programs in Biomedicine, 111 (2). 419 - 434. ISSN 0169-2607 https://doi.org/10.1016/j.cmpb.2013.05.014 Reuse Unless indicated otherwise, fulltext items are protected by copyright with all rights reserved. The copyright exception in section 29 of the Copyright, Designs and Patents Act 1988 allows the making of a single copy solely for the purpose of non-commercial research or private study within the limits of fair dealing. The publisher or other rights-holder may allow further reproduction and re-use of this version - refer to the White Rose Research Online record for this item. Where records identify the publisher as the copyright holder, users can verify any specific terms of use on the publisher’s website. Takedown If you consider content in White Rose Research Online to be in breach of UK law, please notify us by emailing [email protected] including the URL of the record and the reason for the withdrawal request. [email protected] https://eprints.whiterose.ac.uk/ ImaGiNe Seldinger: first simulator for Seldinger technique and angiography training V. Luboz, Y. Zhang, S. Johnson, Y. Song, C. Kilkenny, C. Hunt, H. Woolnough, S. Guediri, J. Zhai, T. Odetoyinbo, P. Littler, A. -
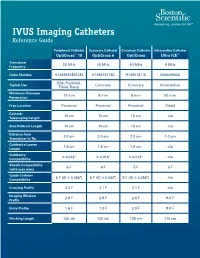
IVUS Imaging Catheters Reference Guide
IVUS Imaging Catheters Reference Guide Peripheral Catheter Coronary Catheter Coronary Catheter Intracardiac Catheter OptiCross™ 18 OptiCross 6 OptiCross Ultra ICE™ Transducer 30 MHz 40 MHz 40 MHz 9 MHz Frequency Order Number H7493932800180 H7495181160 H749518110 M00499000 SFA, Popliteal, Typical Use Coronary Coronary Intracardiac Tibial, Renal Maximum Diameter 12 mm 6 mm 6 mm 50 mm Penetration Prep Location Proximal Proximal Proximal Distal Catheter 15 cm 15 cm 15 cm n/a Telescoping Length Sled Pullback Length 10 cm 10 cm 10 cm n/a Distance from 2.0 cm 2.0 cm 2.0 cm 1.0 cm Transducer to Tip Guidewire Lumen 1.6 cm 1.6 cm 1.6 cm n/a Length Guidewire ≤ 0.018" ≤ 0.014" ≤ 0.014" n/a Compatibility Sheath Compatibility 6 F 6 F 5 F 9 F (with max wire) Guide Catheter 6 F (ID ≥ 0.068") 6 F (ID ≥ 0.064") 5 F (ID ≥ 0.058") n/a Compatibility Crossing Profile 3.5 F 3.1 F 3.1 F n/a Imaging Window 2.9 F 2.9 F 2.6 F 9.0 F Profile Entry Profile 1.6 F 1.3 F 2.0 F 9.0 F Working Length 135 cm 135 cm 135 cm 110 cm OPTICROSS™ 18 CATHETER AND MDU5 PLUS BAG OPTICROSS 6 40 MHZ CORONARY IMAGING CATHETER CAUTION Federal law (USA) restricts this device to sale by or on the order of a physician. Rx only. Prior to use, please see the CAUTION: Federal law (USA) restricts this device to sale by or on the order of a physician. -

Coding Billing
Coding&Billing Quarterly FEBRUARY 2015 EDITOR ALAN L. PLUMMER, MD ATS RUC Advisor Letter from the Editor Welcome to the January 2015 edition of the ATS Coding ADVISORY BOARD MEMBERS: and Billing Quarterly. The New Year will bring a number of KATINA NICOLACAKIS, MD important changes to medicine for practitioners of pulmonary, Chair, ATS Clinical Practice Committee ATS Alternate RUC Advisor critical care and sleep medicine. Below are some issues that ATS STEPHEN P. HOFFMANN, MD members and their staff need to be aware of and prepared for: Member, ATS Clinical Practice Committee ATS CPT Advisor ICD-10 Transition – Barring another last minute intervention MICHAEL NELSON, MD by Congress (which is possible but very unlikely), 2015 will Member, ATS Clinical Practice Committee be the year of the ICD-10 transition. I hope providers and ATS Alternate CPT Advisor practices are well underway preparing for the transition. Over the past year, the STEVE G. PETERS, MD Member, ATS Clinical Practice Committee ATS Coding and Billing Quarterly has featured articles on the transition. The April 2015 edition will cover ICD-10 for pediatric pulmonary services. Lung Cancer Screening Coverage – Earlier this month, the Centers for Medicare In This Issue and Medicaid Services (CMS) released its final coverage policy for lung cancer Low Dose CT Lung Cancer screening. In this issue, Dr. Kovitz describes the final coverage policy, its impact Screening Coverage - Implications on Medicare and private coverage, as well as tips for coding services related to for the Practitioner, page 2 screening. 2015 Brings New Extracorporeal Membrane Oxygenation New ECMO codes – Also covered in this issue is the new and expanded family of (ECMO)/Extracorporeal Life codes for EMCO services. -

General Surgery Residency Curriculum
General Surgery Educational Goals & Objectives General surgeons are specialists in the evaluation and treatment of patients with injuries, deformities, or medical illnesses that require operative intervention. They may diagnose and treat acute and chronic disorders of the breast, endocrine system, gastrointestinal tract, and skin and soft tissue and may go on to further training in a particular area, including such specialties as bariatrics, cardiothoracic surgery, colorectal surgery, oncology, pediatrics, surgical critical care, transplant, trauma, and vascular surgery. Our General Surgery Residency at Community Memorial Hospital will provide the resident with a strong foundation in basic science, including anatomy, biology, immunology, pathology, and physiology, with special expertise in the clinical care of patients in the community. The goal of the residency is to provide exposure to a broad base of surgical interventions and to encourage critical thinking, such that graduates can provide compassionate care at the forefront of knowledge in General Surgery. Residents spend the majority of their initial time in General Surgery, with additional rotations in Anesthesia and Critical Care to develop foundational skills upon which to base further training. Subsequent rotations in General Surgery and its subspecialties hone technical skills and promote dedicated study of General Surgery in both the inpatient and outpatient settings. Focus will be on learning normal and abnormal anatomy, understanding the natural history of surgical disease (untreated, treated medically, and treated surgically), and gaining expertise in multiple procedural skills. Comprehensive experience in pre-and post-operative care as well as exceptional operative training ensures that our residents achieve excellence in the diagnosis and management of surgical disease. -

High Ligation of Sapheno-Femoral Junction and Thermal Ablation For
High ligation of sapheno-femoral junction and thermal ablation for lower limb Ann Ital Chir, 2020 91, 1: 61-64 primary varicosity in day hospital setting pii: S0003469X20030262 Epub Ahead of Print 2 June 2019 free reading: www.annitalchir.com Luciano Izzo*, Federico Pugliese*, Gorizio Pieretti°, Sara Izzo*, Paolo Izzo* With collaboration of : Gaetano Florio***, Mauro Del Papa***, Daniela Messineo** *Department of Surgery “Pietro Valdoni”, Policlinico “Umberto I”, “Sapienza” University, Rome, Italy **Department of Radiological Sciences, Oncology and Pathology, “Sapienza” University, Rome, Italy ***L.P. Delfino Hospital, Department of General Surgery, Colleferro, Rome, Italy °Multidisciplinary Department of Medical-Surgical and Dental Specialties, Plastic Surgery Unit, Università degli Studi della Campania “Luigi Vanvitelli”, Naples, Italy High ligation of sapheno-femoral junction and thermal ablation for lower limb primary varicosity in day hospital setting AIM: The traditional surgical treatment for lower limb primary varicosity has been for a long time high ligation of sapheno-femoral junction and stripping of great saphenous vein. Surgery, however, has been frustrated by postoperative pains and discomfort and recurrences so that it has been challenged by minimally invasive endovenous techniques such as laser treatment and radiofrequency ablation. The aim of the article is to assess the feasibility, in a day hospital set- ting, of a combined approach to greater saphenous vein reflux: high ligation of sapheno-femoral junction and thermal treatment of the great sapenous vein. METHODS: A retrospective analysis on 95 patients treated with high ligation and thermal ablation at our institution from January 2009 to July 2017 was performed, assessing duration of surgery, post-operative pain and analgesics require- ments, early complications and resumption of activities. -

Clinical Review: Vascular Access for Fluid Infusion in Children
Clinical review: Vascular access for fluid infusion in children • Nikolaus A Haas Critical Care20048:478 https://doi.org/10.1186/cc2880 © BioMed Central Ltd 2004 • Published: 3 June 2004 Abstract The current literature on venous access in infants and children for acute intravascular access in the routine situation and in emergency or intensive care settings is reviewed. The various techniques for facilitating venous cannulation, such as application of local warmth, transillumination techniques and epidermal nitroglycerine, are described. Preferred sites for central venous access in infants and children are the external and internal jugular veins, the subclavian and axillary veins, and the femoral vein. The femoral venous cannulation appears to be the most safe and reliable technique in children of all ages, with a high success and low complication rates. Evidence from the reviewed literature strongly supports the use of real- time ultrasound techniques for venous cannulation in infants and children. Additionally, in emergency situations the intraosseous access has almost completly replaced saphenous cutdown procedures in children and has decreased the need for immediate central venous access. Keywords • central venous access • child • epidermal nitroglycerine • intraosseous • transillumination • venous cutdown Introduction Nothing can be more difficult, time consuming and frustrating than obtaining vascular access in the paediatric patient. This was best described by Orlowski in 1984 [1], who stated, 'My kingdom for an intravenous line'. -

I Have Reviewed the DOP/Roster Provided to Me by MSS and Confirm As Indicated Below
ATRIUM HEALTH REAPPOINTMENT DELINEATION OF PRIVILEGES SPECIALTY OF EMERGENCY MEDICINE I have reviewed the DOP/Roster provided to me by MSS and confirm as indicated below: My DOP is accurate and reflects privileges relevant to my current practice I have listed privileges that should be removed: Printed Name: Signature: Date: If your roster indicates that you hold any of the privileges listed below, you must provide the maintenance criteria as described, in order to maintain the privilege. Your maintenance criteria and attestation must be returned together. Maintenance Criteria for Continued Special Privileges (CEMD-1(a-c): • Emergency Ultrasound – Biliary (Cholecystitis and Cholelithiasis) • Emergency Ultrasound – Urinary Tract (Hydronephrosis and bladder size) • Emergency Ultrasound – DVT The Physician must submit a minimum of ten (10) cases over the past two (2) years for each ultrasound privileges held, based on acceptable results of ongoing professional practice evaluation and outcomes, and five (5) ultrasound related Category I or II CME hours over the past two (2) years to reapply for special privileges. This will be reviewed at the time of reappointment. Physicians who would like to continue to hold any special privileges but are unable to document the minimal number will be requested to voluntarily withdraw their request for such privileges and to complete the necessary proctoring forms. Maintenance Criteria for Continued Special Privileges (CEMD-1(d-e): • Emergency Ultrasound – Thoracic • Emergency Ultrasound - Bowel The Physician must submit a minimum of two (2) cases over the past two (2) years for each ultrasound privileges held, based on acceptable results of ongoing professional practice evaluation and outcomes to reapply for special privileges. -

Open Seldinger-Guided Peripheral Femoro-Femoral Cannulation
Chen et al. Journal of Cardiothoracic Surgery (2021) 16:199 https://doi.org/10.1186/s13019-021-01584-x RESEARCH ARTICLE Open Access Open Seldinger-guided peripheral femoro- femoral cannulation technique for totally endoscopic cardiac surgery Yi Chen1,2, Liang-wan Chen1, Xiao-fu Dai1 and Xue-shan Huang1,2* Abstract Background: The cannulation technique used in totally endoscopic cardiac surgery has a significant impact on the overall prognosis of patients. However, there are no large cohort studies to discuss it. Here we report on our research of using open Seldinger-guided technique to establish femoro-femoral cardiopulmonary bypass during totally endoscopic cardiac surgery and evaluate its safety and efficacy. Methods: The institutional database from 2017 to 2020 was retrospectively reviewed to find cases in which totally endoscopic cardiac surgery was performed. We identified 214 consecutive patients who underwent totally endoscopic cardiac surgery with peripheral femoro-femoral cannulation. All patients underwent femoral artery cannulation. Of these, 201 were cannulated in the femoral vein and 13 were cannulated in the femoral vein combined with internal jugular cannulation. The technique involves surgically exposing the femoral vessel, setting up purse-string over the vessels and then inserting a guidewire into the femoral vessel without a vascular incision, followed by exchange of the guidewire with a cannula. Results: Surgery indications included mitral valve disease in 82.71% (177/214), atrial septal defect in 11.68% (25/214) and tricuspid regurgitation in the remaining 5.61% (12/214). Hospital survival was 98.60% (211/214). There were no cases of stroke and postoperative limb ischaemia.