Curettage Prior to Mohs' Micrographic Surgery for Previously Biopsied
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

CPT® New Codes 2019: Biopsy, Skin
Billing and Coding Update Alexander Miller, M.D. AAD Representative to the AMA CPT Advisory Committee New Skin Biopsy CPT® Codes It’s all about the Technique! SPEAKER: Alexander Miller, M.D. AAD Representative to the AMA -CPT Advisory Committee Chair AAD Health Care Finance Committee Arriving on January 1, 2019 New and Restructured Biopsy Codes Tangential biopsy Punch Biopsy Incisional Biopsy How Did We Get Here? CMS CY 2016 Biopsy codes (11100, 11101 identified as potentially mis-valued; high expenditure RUC Survey sent to AAD Members Specialty survey results are the only tool available to support code values Challenging survey results Survey revealed bimodal data distribution; CPT Codes 11100, 11101 referred to CPT for respondents were valuing different procedures restructuring Rationale for New Codes 11100; 11101 • Previous skin biopsy codes did not distinguish between the different biopsy techniques that were being used CPT Recommended technique specification in new biopsy codes • Will also provide for reimbursement commensurate with the technique used How Did We Get Here? • CPT Editorial Panel deleted 11100; 11101 February 2017 • 6 New codes created based on technique utilized • Each technique: primary code and add-on code March 2017 • RUC survey sent to AAD members April 2017 • Survey results presented to the RUC Biopsy Codes Effective Jan., 1, 2019 • Integumentary biopsy codes 11755 Biopsy of nail unit (plate, bed, matrix, hyponychium, proximal and lateral nail folds 11100, 11101 have been deleted 30100 Biopsy, intranasal • New -
Mohs Surgery Educational Information for Patients
DEPARTMENT OF DERMATOLOGY Mohs Surgery Educational information for patients Thank you for choosing the OHSU Department of Dermatology to provide your dermatologic care. Since the 1920s, the Department of Dermatology has been educati ng doctors, researching skin diseases and providing world-class care to pati ents in Oregon and beyond. We thank you for trusti ng us with your care. The surgeons and staff within the department welcome you. We have prepared this educati onal informati on to answer the most common questi ons presented to us by our pati ents. If you have additi onal questi ons aft er reading this material, please let us know. Some of the questi ons addressed include: • What is skin cancer? • What is Mohs surgery? • How do I prepare for Mohs surgery? • What happens the day of surgery? • What type of wound will I have and how will I care for that wound aft er surgery? • What measures can I take to prevent future skin cancer? What is skin cancer? Cancer is the abnormal growth of cells at an uncontrolled and unpredictable rate. The cancer tissue usually grows at the expense of surrounding normal tissue. The abnormal growth (cancer) originates in the uppermost layer of the skin and may grow downward, forming root and fi nger-like projections under the surface of the skin. Unfortunately, these roots may be subtle and unable to be seen without the aid of a microscope. Therefore, what you see on your skin is sometimes only a small portion of the total cancer. The most common types of skin cancer are basal cell carcinoma and squamous cell carcinoma. -

MOHS SURGERY INFORMATION SHEET Greg S
1 California Skin Institute MOHS SURGERY INFORMATION SHEET Greg S. Morganroth, MD Brian Somoano, MD Joanna Chan, MD www.CAskin.com 525 South Drive, Suite 115 Ph: (650) 969-5600 2420 Samaritan Drive Ph: (408) 369-5600 Mountain View, California 94040 Fax: (650) 969-0360 San Jose, CA 95124 Fax: (408) 558-7949 PLEASE NOTE: THIS INFORMATION SHEET; A REGISTRATION FORM FOR NEW PATIENTS; BEFORE AND AFTER PHOTOS OF ADVANCED FACIAL RECONSTRUCTION; AND ADDITIONAL RESOURCES CAN BE FOUND AT: www.CAskin.com. You are waiting to undergo an advanced skin cancer removal procedure called Mohs Micrographic Surgery. The origin of this technique dates back to the 1930’s when Dr. Frederick Mohs at The University of Wisconsin was researching a way to remove complicated skin cancers unresponsive to traditional therapies such as standard excisional surgery, cryosurgery (freezing), electrodessication and curettage (scraping and burning), and radiation therapy. In the 21st Century, Mohs Micrographic Surgery represents the state-of-the-art treatment for skin cancer by providing the highest cure rate, minimal sacrifice of normal skin, and smallest possible scar. The American College of Mohs Micrographic Surgery and Cutaneous Oncology (www.mohscollege.org) is the official organization responsible for training Mohs surgeons and maintaining the standard-of-care in the specialty of Mohs Surgery. To become a member of this organization and be known as a Mohs surgeon, a special one to two-year fellowship following a dermatology residency is required. Only a limited number of dermatologists are trained each year to be Mohs surgeons to maintain the highest level of competence in the specialty. -
MOHS SURGERY and RECONSTRUCTION a Handbook for Patients
MOHS AND DERMATOLOGIC SURGERY CENTER MOHS SURGERY AND RECONSTRUCTION A Handbook for Patients Focused on cancer. Focused on life. Table of Contents Introduction.....................................................................................................2 Skin Cancer Types............................................................................................3 Causes of Skin Cancer......................................................................................4 Growth of Skin Cancer ....................................................................................4 Skin Cancer Treatment ....................................................................................4 Mohs Surgery ...................................................................................................5 Steps in Mohs Surgery......................................................................................5 Duration of Mohs Surgery ...............................................................................7 Effectiveness of Mohs Surgery ..........................................................................7 Advantages of Mohs Surgery ............................................................................7 Reconstruction of the Surgical Wound.............................................................8 Pre-Operative Instructions................................................................................9 Pre-Operative Medications ...............................................................................9 Healing -

A Practical Guide to Frozen Section Technique Stephen R
A Practical Guide to Frozen Section Technique Stephen R. Peters Editor A Practical Guide to Frozen Section Technique Editor Stephen R. Peters University of Medicine and Dentistry of New Jersey New Jersey Medical School Newark, NJ USA [email protected] ISBN 978-1-4419-1233-6 e-ISBN 978-1-4419-1234-3 DOI 10.1007/978-1-4419-1234-3 Springer New York Dordrecht Heidelberg London Library of Congress Control Number: 2009933112 © Springer Science+Business Media, LLC 2010 All rights reserved. This work may not be translated or copied in whole or in part without the written permission of the publisher (Springer Science+Business Media, LLC, 233 Spring Street, New York, NY 10013, USA), except for brief excerpts in connection with reviews or scholarly analysis. Use in connection with any form of information storage and retrieval, electronic adaptation, computer software, or by similar or dissimilar methodology now known or hereafter developed is forbidden. The use in this publication of trade names, trademarks, service marks, and similar terms, even if they are not identified as such, is not to be taken as an expression of opinion as to whether or not they are subject to proprietary rights. Printed on acid-free paper Springer is part of Springer Science+Business Media (www.springer.com) Preface Frozen section technique is a valuable tool used to rapidly prepare slides from tis- sue for microscopic interpretation. Frozen section technique is used in a myriad of clinical and research settings. In surgical pathology, frozen sections are routinely used for rapid intra-operative diagnosis, providing guidance for our surgical col- leagues. -
Mohs Micrographic Surgery: Current Techniques Ofer Arnon MD1, Ronald P
IMAJ • VOL 12 • JuLy 2010 REVIEWS Mohs Micrographic Surgery: Current Techniques Ofer Arnon MD1, Ronald P. Rapini MD2, Adam J. Mamelak MD3 and Leonard H. Goldberg MD4 1Department of Plastic and Reconstructive Surgery, Soroka University Medical Center and Faculty of Health Sciences, Ben-Gurion University of the Negev, Beer Sheva, Israel 2Departments of Dermatology and Pathology, University of Texas Medical School and MD Anderson Cancer Center, Houston, TX, USA 3Department of Dermatology, The Methodist Hospital, Houston, TX, USA 4DermSurgery Associates, Houston, TX, USA evaluation. The “horizontal” sectioning allowed for complete KEY WORDS: Mohs micrographic surgery, frozen sections, skin tumors, examination of the peripheral tumor margin. Since then, his tissue conservation, histologically clear margins technique has continued to evolve. It has become the gold IMAJ 2010; 12: 431–435 standard and has found a secure niche in the management of cutaneous malignancies. CUTANEOUS MALIGNANCY For Editorial see page 441 Several modalities are used for the treatment of skin cancers, ohs micrographic surgery is considered the most con- including curettage and electrodessication, laser, cryotherapy, M servative yet reliable approach to the management of radiation therapy, topical or intralesional drug therapy, con- cutaneous malignancies. The concept of MMS is simple, ventional excision, and MMS. Laser, cryotherapy and radiol- but its technique, which involves a series of suboperations, ogy are destructive procedures that rely on clinical and often is complex. Although many refinements have been made visual assessment of the tumor’s extent but lack pathologic to the original Mohs technique, the main objectives are the verification of clear margins. ED&C does not permit margin same. -

Mohs Micrographic Surgery FACT SHEET
IMPORTANT REMINDERS FOR YOUR MOHS SURGERY 9/15/11 DO advise us as soon as possible if you must cancel or change your appointment. If you have a bad cold, the flu, or a fever greater than 100˚, the day prior to your surgery, call the office 731-784-4300. It may be necessary to reschedule your appointment. DO get a good night’s sleep prior to surgery. DO take your usual medications on schedule unless instructed otherwise. DO eat a good breakfast, and consider bringing snacks or a light lunch. DO dress comfortably with a button up shirt or blouse if your surgery is on the chest or back. Avoid wearing an undershirt which must be pulled over the head. DO bathe & shampoo your hair the night prior to surgery (the surgery site must be kept absolutely dry for at least 24 hours after surgery). DO bring something to occupy your time for the waiting periods, WIFI is available in the clinic. DO let us know on the medical history form if you are taking aspirin or products containing aspirin under the direction of a physician. DO BRING A DRIVER. DRIVING CAN BE HAZARDOUS AND IS STRONGLY DISCOURAGED IF WE ARE WORKIONG AROUND YOUR EYES. DO have plain Tylenol on hand at home, and bring some with you, to take before your local anesthesia wears off. You should plan to take some 3x a day for the first 3 days. DO have ice packs at home (a freezer bag of frozen peas or corn kernels works well). DO NOT stop your blood thinner such as Plavix, Coumadin, or aspirin if prescribed by a doctor. -

Revised Mohs Surgery Care Guidelines for Squamous Cell Carcinoma In-Situ Are Overdue
Volume 25 Number 3| March 2019| Dermatology Online Journal || Commentary 25(3):2 Revised Mohs surgery care guidelines for squamous cell carcinoma in-situ are overdue Sama K Carley1 MD, Anthony Dixon2 PhD MBBS, Christopher B Zachary1 MBBS FRCP, Howard K Steinman3,4 MD Affiliations: 1University of California Irvine, Department of Dermatology, Irvine, California, USA, 2Australasian College of Cutaneous Oncology, Docklands, Victoria, Australia, 3Campbell University School of Osteopathic Medicine, Lillington, NC, USA, 4US Dermatology Partners, Grapevine, Texas, USA Corresponding Author: Christopher B. Zachary MBBS FRCP, University of California, Irvine, Department of Dermatology, 118 Med Surge I, Irvine, California 92697, Tel: 949-824-4405, Email: [email protected] Surgery Appropriate Use Criteria (MAUC), [1]. We Abstract discuss the rationale for a change in the MAUC for The treatment of cutaneous squamous cell SCCis. carcinoma in situ by Mohs micrographic surgery is currently deemed as appropriate by the Mohs Discussion Appropriate Use Criteria. However, squamous cell carcinoma in situ is a very superficial, indolent, low- Cutaneous SCCis is a common, intra-epidermal, low- risk tumor amenable to destructive and non-surgical risk, indolent malignancy [2, 3]. Many involve the treatments. It is uncommon for squamous cell superficial hair follicle [4]. However, risk of progression carcinoma in situ to have progressed to invasive to invasive SCC is only 3-5%, and SCCis has a negligible malignancy subsequent to definitive management. risk of metastasis [5, 6]. This low risk of progression to The suggestion that squamous cell carcinoma in situ SCC and metastasis exists despite the reported on certain anatomic locations has a poorer prognosis presence of invasive SCC in 9.8% of biopsies diagnosed is widely assumed but lacks an evidence base. -
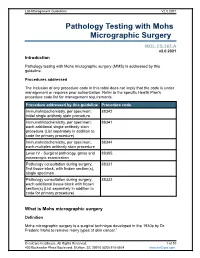
Pathology Testing with Mohs Micrographic Surgery
Lab Management Guidelines V2.0.2021 Pathology Testing with Mohs Micrographic Surgery MOL.CS.363.A v2.0.2021 Introduction Pathology testing with Mohs micrographic surgery (MMS) is addressed by this guideline. Procedures addressed The inclusion of any procedure code in this table does not imply that the code is under management or requires prior authorization. Refer to the specific Health Plan's procedure code list for management requirements. Procedure addressed by this guideline Procedure code Immunohistochemistry, per specimen; 88342 initial single antibody stain procedure Immunohistochemistry, per specimen; 88341 each additional single antibody stain procedure (List separately in addition to code for primary procedure) Immunohistochemistry, per specimen; 88344 each multiplex antibody stain procedure Level IV - Surgical pathology, gross and 88305 microscopic examination Pathology consultation during surgery; 88331 first tissue block, with frozen section(s), single specimen Pathology consultation during surgery; 88332 each additional tissue block with frozen section(s) (List separately in addition to code for primary procedure) What is Mohs micrographic surgery Definition Mohs micrographic surgery is a surgical technique developed in the 1930s by Dr. Frederic Mohs to remove many types of skin cancer.1 © eviCore healthcare. All Rights Reserved. 1 of 10 400 Buckwalter Place Boulevard, Bluffton, SC 29910 (800) 918-8924 www.eviCore.com Lab Management Guidelines V2.0.2021 It is performed by dermatologists, many of whom have completed a one or two year fellowship in Mohs surgery.2 One of the defining, and unique, features of this technique is that the Mohs surgeon also serves the role of the pathologist, examining frozen sections of excised tissue at the time of surgery. -

Tumescent Anesthesia As an Aid for Wide Local Excision in Dermatologic Surgery
140 How do I do? Tumescent anesthesia as an aid for wide local excision in dermatologic surgery Anestesia tumescente: técnica auxiliar para excisões exten- sas em cirurgia dermatológica Authors: Jerry D. Brewer 1 Randall K. Roenigk 2 ABSTRACT Introduction: Local anesthesia is the most common form of anesthesia used in cuta- 1 Department of Dermatology neous surgery. Some patients have comorbidities that put them at risk for general anes- Division of Dermatologic Surgery thesia.Tumescent anesthesia is the technique of injecting a large amount of dilute local Mayo Clinic/Mayo Clinic College of anesthesia into the subcutaneous plane of the skin. Tumescent anesthesia can minimize Medicine Rochester, MN discomfort, aid in hemostasis, and contribute to the ease of closing large surgical defects 2 Department of Dermatology that would otherwise be challenging. Division of Dermatologic Surgery Mayo Clinic/Mayo Clinic College of Objective: To discuss the pros and cons of using tumescent anesthesia in dermatologic Medicine Rochester, MN surgery. Conclusion: Tumescent anesthesia is a viable option that can aid in cutaneous recon- structive surgery, especially when removing tissue in the deeper subcutaneous fat or fas- Correspondência para: cia.Tumescent anesthesia is also associated with good results and few adverse reactions. Jerry D. Brewer Assistant Professor of Dermatology Keywords: anesthesia; skin neoplasms; mohs surgery. Department of Dermatology Division of Dermatologic Surgery Mayo Clinic College of Medicine RESUMO 200 First Street SW Introdução: A anestesia local é a forma mais comum de anestesia utilizada em cirurgias cutâneas. Rochester, Minnesota 55095 +1 (507) 284-3668 Alguns pacientes possuem comorbidades que os colocam no grupo de risco para anestesia geral. -

In Dermatologic Plastic Surgery--- Name Is Game
In Dermatologic Plastic Surgery--- Name is Game Nothing endures but change. -Heracleitus In the last half century dermatology has seen a revolutionary change in the way cosmetic and oncologic surgery is perceived and performed. The increased focus on dermatologic surgery may be surprising to many physicians who trained in the mid twentieth century. However, many founding members of our specialty were originally surgeons who later became interested in skin disease. The first national dermatologic society, the American Dermatologic Association, was established in 1876. Many of its early members were former civil war military surgeons. Because of the high incidence of venereal or urologic disease, the focus of dermatologists of this era was on both dermatology and venerealology. In 1932 the American Board of Dermatology was established, the fourth specialty board of the American Board of Medical Specialties (ABMS). Since that time, more effective medical and surgical advances have been developed which have changed our patients’ lives and the way we practice medicine. Since the mid twentieth century, we have seen a resurgence in the importance of surgery in the practice of dermatology. Growing public interest in aesthetic surgery has led to developments in this field. Many of the pioneers in new or refined techniques have been dermatologists, who have used their knowledge in dermatology to “think outside of the box.” Dermatology residency or surgical fellowship has provided them a foundation upon which to build surgical experience and expertise. For example, this foundation has led to the concepts of laser utility in the treatment of skin disease, donor dominance in hair transplantation, tumescent liposuction with dilute anesthetic solution and micro-cannulas, Mohs micrographic surgery for cutaneous tumors, and laser and radiofrequency endovascular surgery. -

Dr. Hooman Khorasani
EXPERT BEAUTY GUIDE FROM LEADING BOARD-CERTIFIED DERMATOLOGIST DR. HOOMAN KHORASANI HOW TO SCULPT YOUR BEST BODY WITH LIPOSUCTION PG 1 FIGHT FAT PG 2 CORRECT PG 3 GET BIKINI PG 4 SLIM YOUR FOREVER AND TONE READY SHAPE GET RID OF FAT: SCULPT AND RESHAPE YOUR BODY Liposuction, also known as lipoplasty or suction lipectomy, involves the removal of unwanted fat through a vacuum apparatus to reduce fat bulges or pockets. By removing fat with suction through small incisions, your doctor is able to sculpt and shape the curves of your body. Common sites for administering liposuction include the chin, neck, arms, abdomen, thighs, buttocks and even calves and ankles. Types of liposuction include traditional, power-asisted, laser, ultrasound, water-jet and radio frequency. 02 01 03 Traditional Power-Assisted Laser Best for: Entire body (arms, inner Best for: Entire body Best for: Body and face thigh, neck and lower abdomen) This option makes use of special The added bonus for this procedure This option can be used to sculpt equipment to give the cannula the is that the heat emitted by the a more ideal shape, making it more power necessary to dislodge fat. laser can create new collagen to proportional. The traditional tighten minimally loose skin. version is best if you have localized How it works: Power-assisted fat deposits with good skin tone. liposuction uses a cannula that How it works: Laser liposuction moves back and forth to suction delivers laser energy to the tissues How it works: Traditional lipo uses out fat. This technique is also with a fiber to purportedly break hollow metal tubes called cannulas the most similar technique to up fat cells.