Regulating Mitochondrial Donation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Feeling Controlled in Marriage: a Phenomenon Specific to Physically Aggressive Couples? Miriam K
Journal of Family Psychology Copyright 1999 by the American Psychological Association, Inc. 1999, Vol. 13, No. 1,20-32 0893-320O/99/$3.0O Feeling Controlled in Marriage: A Phenomenon Specific to Physically Aggressive Couples? Miriam K. Ehrensaft, Jennifer Langhinrichsen-Rohling, Richard E. Heyman, K. Daniel O'Leary, and Erika Lawrence State University of New York at Stony Brook Spouses in maritally happy nonaggressive (H; n = 21), distressed nonaggressive (DNA; n = 16), and distressed aggressive (DA; n = 20) marriages were inter- viewed about their perceptions of their spouse as controlling. Four areas of spousal control were assesed: involvement in decision making, relationships with family and friends, freedom to plan activities independently, and sense of competence and self-respect. Overall, as expected, spouses in happy marriages reported feeling less controlled than spouses in the 2 distressed groups. Few gender differences were obtained, with the exception that wives in aggressive marriages were more likely to report that their husbands controlled their sense of competence and self-respect. Differences between the DA and DNA groups depended on the specific area of control. Wives in the aggressive couples were significantly more likely than their husbands to state that their spouse's aggression was an attempt to control them. Scholars and practitioners from a variety of between marital aggression and control, defini- theoretical perspectives have asserted that there tions of control produced by each theory, and is a relationship between coercive control and empirical research that has been associated with the occurrence of physical aggression in mar- these definitions. Then a definition of control is riage (Black, 1983; Finkelhor, 1983; Gondolf, offered, drawing from each of these three 1985; Stets, 1988). -
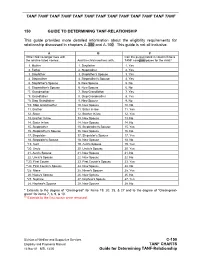
Cussed in Chapters A-300 and A-100
TANF TANF TANF TANF TANF TANF TANF TANF TANF TANF TANF TANF TANF 150 GUIDE TO DETERMINING TANF-RELATIONSHIP This guide provides more detailed information about the eligibility requirements for relationship discussed in chapters A-300 and A-100. This guide is not all inclusive. A B C If the child no longer lives with Can the person listed in column B be a the relative listed +below... And the child now lives with... TANF caregiver/payee for the child? 1. Mother 1. Stepfather 1. Yes 2. Father 2. Stepmother 2. Yes 3. Stepfather 3. Stepfather's Spouse 3. Yes 4. Stepmother 4. Stepmother's Spouse 4. Yes 5. Stepfather's Spouse 5. New Spouse 5. No 6. Stepmother's Spouse 6. New Spouse 6. No *7. Grandmother 7. Step Grandfather 7. Yes *8. Grandfather 8. Step Grandmother 8. Yes *9. Step Grandfather 9. New Spouse 9. No *10. Step Grandmother 10. New Spouse 10. No 11. Brother 11. Sister In-law 11. Yes 12. Sister 12. Brother In-law 12. Yes 13. Brother In-law 13. New Spouse 13. No 14. Sister In-law 14. New Spouse 14. No 15. Stepbrother 15. Stepbrother's Spouse 15. Yes 16. Stepbrother's Spouse 16. New Spouse 16. No 17. Stepsister 17. Stepsister's Spouse 17. Yes 18. Stepsister's Spouse 18. New Spouse 18. No *19. Aunt 19. Aunt's Spouse 19. Yes *20. Uncle 20. Uncle's Spouse 20. Yes 21. Aunt's Spouse 21. New Spouse 21. No 22. Uncle's Spouse 22. New Spouse 22. No **23. First Cousin 23. -

Proof of Marriage for the Purpose of Obtaining Retirement Benefits We Are Asking for Proof of Your Marriage; the Items Listed Below Tell You What You Should Send Us
United States Office of Personnel Management Retirement Operations Washington, D.C. 20415-0001 Proof of Marriage for the Purpose of Obtaining Retirement Benefits We are asking for proof of your marriage; the items listed below tell you what you should send us. Ceremonial Marriage C. The address or addresses at which you resided while To prove a ceremonial marriage we require: you lived together; 1. A copy of the original certificate of marriage, if available; D. Whether there was any public announcement in or connection with your common law marriage; 2. A copy of a public or religious institutions’s record of E. Whether you and your spouse were regarded among marriage, or a statement as to the contents of such a record, your neighbors, friends, and relatives as being husband certified by the authorized custodian of the record; or and wife during the time you lived together; and 3. If neither of the above proofs of marriage is available, you F. How the person swearing the affidavit is in a position to must send us a statement explaining why such proofs know the facts being presented in the affidavit. cannot be obtained. Along with this explanation, send us any or all proofs listed below: 2. Your own affidavit is also required. In your affidavit you should state: - An affidavit of the clergyman or other authorized A. The date on which and the State in which you and your official who performed the marriage. spouse mutually agreed to become husband and wife; - Affidavits of two witnesses to the marriage ceremony. -

An Essential Dichotomy in Australian Kinship Tony Jefferies
11 Close–Distant: An Essential Dichotomy in Australian Kinship Tony Jefferies Abstract This chapter looks at the evidence for the close–distant dichotomy in the kinship systems of Australian Aboriginal societies. The close– distant dichotomy operates on two levels. It is the distinction familiar to Westerners from their own culture between close and distant relatives: those we have frequent contact with as opposed to those we know about but rarely, or never, see. In Aboriginal societies, there is a further distinction: those with whom we share our quotidian existence, and those who live at some physical distance, with whom we feel a social and cultural commonality, but also a decided sense of difference. This chapter gathers a substantial body of evidence to indicate that distance, both physical and genealogical, is a conception intrinsic to the Indigenous understanding of the function and purpose of kinship systems. Having done so, it explores the implications of the close–distant dichotomy for the understanding of pre-European Aboriginal societies in general—in other words: if the dichotomy is a key factor in how Indigenes structure their society, what does it say about the limits and integrity of the societies that employ that kinship system? 363 SKIN, KIN AND CLAN Introduction Kinship is synonymous with anthropology. Morgan’s (1871) Systems of Consanguinity and Affinity of the Human Family is one of the founding documents of the discipline. It also has an immediate connection to Australia: one of the first fieldworkers to assist Morgan in gathering his data was Lorimer Fison, who, later joined by A. -

BMT CTN PROTOCOL 0201 Version 8.0 Study Chairperson
A Phase III Randomized, Multicenter Trial Comparing G-CSF Mobilized Peripheral Blood Stem Cell with Marrow Transplantation from HLA Compatible Unrelated Donors BMT CTN PROTOCOL 0201 Version 8.0 Study Chairperson Claudio Anasetti, M.D. 1 Protocol Team Colleen Allen 2 Stephanie J. Lee, M.D. 8 Paolo Anderlini, M.D. 3 Susan Leitman, M.D. 9 William Bensinger, M.D. 1 Brent Logan, Ph.D. 6 Michael R. Bishop, M.D. 4 Phyllis Mitchell, M.S. 10 Shelly Carter, Sc.D. 2 Scott D. Rowley, M.D. 11 Dennis L. Confer, M.D. 5 Edmund K. Waller, M.D., Ph.D. 12 Mary Horowitz, M.D., M.S. 6 Daniel Weisdorf, M.D. 13 Chatchada Karanes, M.D. 7 John R. Wingard, M.D. 14 Roberta J. King, M.P.H. 5 Sponsored by the National Institutes of Health National Heart, Lung, and Blood Institute National Cancer Institute and the National Marrow Donor Program 1 Fred Hutchinson Cancer Research Center 7 City of Hope 2 The EMMES Corporation 8 Dana Farber Cancer Institute 3 M.D. Anderson Cancer Center 9 NIH Department of Transfusion Medicine 4 National Cancer Institute 10 National Heart, Lung, and Blood Institute 5 National Marrow Donor Program 11 Hackensack University Medical Center 6 Center for International Blood and Marrow 12 Emory University Hospital Transplant Research, Medical College of 13 University of Minnesota Wisconsin 14 University of Florida, Shands Hospital BMT CLINICAL TRIALS NETWORK Core Study Participants: Non-Core Study Participants: City of Hope National Medical Center Baylor College of Medicine City of Hope Samaritan Baylor University Medical Center Dana Farber/Partners Cancer Center CancerCare Manitoba Duke University Medical Center Centre Hospitalier L’hotel Dieu de Quebec Fred Hutchinson Cancer Research Center CHA Hôpital L’Enfant – Jésus Hackensack University Medical Center (PBMTC) Emory University Hospital Karmanos Cancer Institute (PBMTC) Hackensack Univ Medical Center (Adults) Oregon Health Sciences University (CWRU/PBMTC) Hamilton Health Sciences Schneider Children's Hospital (PBMTC) Hôpital Maisonneuve – Rosemont St. -

Mitochondrial Donation
Mitochondrial Donation Standard Note: SN/SC/6833 Last updated: 29 January 2015 Author: Dr Sarah Barber - Science and Environment Section Dr Peter Border – Parliamentary Office of Science and Technology (POST) New mitochondrial donation techniques could provide an option for women with mitochondrial DNA mutations to enable them to give birth to healthy children. They involve using donor mitochondria in an in vitro fertilisation (IVF) treatment. The techniques (maternal spindle transfer and pronuclear transfer) have been subject to three scientific reviews (2011, 2013 and a further update in 2014) by a Human Embryology and Fertilisation Authority expert panel, an ethical review by the Nuffield Council on Bioethics and a HFEA public consultation. In 2013, the HFEA advised the Government that there is general support for the introduction of these treatments. They recommended that further research is still needed and the treatment should be offered within a strict regulatory framework. On 17 December 2014, the Under-Secretary of State for Health announced that the Regulations to allow for the introduction of these techniques had been laid before the House. This followed a consultation on draft regulations and a scientific review update by the HFEA expert panel in 2014. A House of Commons debate on the Regulations has been tabled for 3 February 2015. A number of safety and ethical considerations have been raised in regard to mitochondrial donation. The treatments involve changing the embryo’s mitochondrial DNA prior to implantation. However, the nuclear DNA, which makes up over 99% of our total DNA will not be altered by these treatments. There has been some opposition to their proposed introduction and the media have reported that the techniques will lead to three parent babies. -

August 2017 1
Minnesota Women’s Press, August 2017 1 Changing the Universe through Women’s Stories Body Awareness issue What do you love about your body? Jennifer Almanza: Midwife with a cause Lara Tate: Menopausal Superhero! Learning how to live and die Girls on the Run Women at the Fringe DAWN ROSSBACH DAWN AUGUST 2017 Volume 33, Issue 8 www.womenspress.com Are you ... 2 Minnesota Women’s Press, August 2017 Program Information Program Outcomes I have become more WHO? articulate in voicing my under- The Women In Leadership program is designed for you We welcome all women. Women who runWomen “standing of leadershipin and whyA seriesAreto of explore fouryou and retreats set your ... own for path companies, small businesses, manage de- I make the decisions I do. women seekingLearn how tonew use differences insight to create collective partments, or provide informal leadershipLeadership –WIL Participant • find benefit from these gatherings. wisdom. 20132018 PROGRAMProgram • Increase personal power and leadership integrity. WHEN? WIL is about finding your own leadership style and getting Develop a clear sense of personal purpose and vocation. Women In Leadership meets four times. • “the space and the time to reflect The three-day retreats • Gain momentum for personal transformation. for 2013 are held on: Bringingon what kind our of leader whole you selves into the world March 20-22: ARC could be. Not to make yourself • Learn how to create conditions for effective teamwork If you are into something else, but giving May 15-17: ARC and community. you the time to discover what July 17-19: Lutsen b Asking questions about identity, meaning and you have inside of yourself. -

Should the U.S. Approve Mitochondrial Replacement Therapy?
SHOULD THE U.S. APPROVE MITOCHONDRIAL REPLACEMENT THERAPY? An Interactive Qualifying Project Report Submitted to the Faculty of WORCESTER POLYTECHNIC INSTITUTE In partial fulfillment of the requirements for the Degree of Bachelor of Science By: ____________________ ____________________ ____________________ Daniela Barbery Emily Caron Daniel Eckler IQP-43-DSA-6594 IQP-43-DSA-7057 IQP-43-DSA-5020 ____________________ ____________________ Benjamin Grondin Maureen Hester IQP-43-DSA-5487 IQP-43-DSA-2887 August 27, 2015 APPROVED: _________________________ Prof. David S. Adams, PhD WPI Project Advisor 1 ABSTRACT The overall goal of this project was to document and evaluate the new technology of mitochondrial replacement therapy (MRT), and to assess its technical, ethical, and legal problems to help determine whether MRT should be approved in the U.S. We performed a review of the current research literature and conducted interviews with academic researchers, in vitro fertility experts, and bioethicists. Based on the research performed for this project, our team’s overall recommendation is that the FDA approve MRT initially for a small number of patients, and follow their offspring’s progress closely for a few years before allowing the procedure to be done on a large scale. We recommend the FDA approve MRT only for treating mitochondrial disease, and recommend assigning parental rights only to the two nuclear donors. In medical research, animal models are useful but imperfect, and in vitro cell studies cannot provide information on long-term side-effects, so sometimes we just need to move forward with closely monitored human experiments. 2 TABLE OF CONTENTS Title Page ……………………………….……………………………………..……. 01 Abstract …………………………………………………………………..…………. 02 Table of Contents ………………………………………………………………..… 03 Acknowledgements …………………………………………………………..……. -

Mitochondrial Medicine 2019: Washington DC Scientific and Clinical Meetings June 26-29, 2019 Hilton Alexandria Mark Center Alexandria, VA
Mitochondrial Medicine 2019: Washington DC Scientific and Clinical Meetings June 26-29, 2019 Hilton Alexandria Mark Center Alexandria, VA 2019 Course Chairs: Amel Kara, MD and Carla Koehler, PhD 2019 CME Chair: Bruce H. Cohen, MD Mitochondrial Medicine 2019: Washington DC Scientific/Clinical Program June 26-29, 2019 Course Description The United Mitochondrial Disease Foundation and PeerPoint Medical Education Institute have joined efforts to sponsor and organize a CME-accredited symposium. Mitochondrial diseases are more common than previously recognized and mitochondrial pathophysiology is now a recognized part of many disease processes, including heart disease, cancer, AIDS and diabetes. There have been significant advances in the molecular genetics, proteomics, epidemiology and clinical aspects of mitochondrial pathophysiology. This conference is directed toward the scientist and clinician interested in all aspects of mitochondrial science. The content of this educational program was determined by rigorous assessment of educational needs and includes surveys, program feedback, expert faculty assessment, literature review, medical practice, chart review and new medical knowledge. The format will include didactic lectures from invited experts intermixed with peer-reviewed platform presentations. There will be ample time for professional discussion both in and out of the meeting room, and peer-reviewed poster presentations will be given throughout the meeting. This will be a four-day scientific meeting aimed at those with scientific and -

D D M M Y Y D D M M Y Y This Form Is Produced by the Human
Following MST, the eggs containing your mitochondria will be fertilised with the intended This form is produced by the Human father’s (or a donor’s) sperm to create embryos Fertilisation and Embryology Authority (HFEA), which will be used in the intended mother's the UK’s independent regulator of fertility treatment. This means that the intended mother, treatment and human embryo research. For not you, will be the genetic parent of any child more information about us, visit that is born. www.hfea.gov.uk. In PNT, your eggs will be fertilised with the intended father’s (or a donor’s) sperm to create Fill in this form if you are donating eggs and/or embryos. The nuclear genetic material within embryos created with your eggs for use in these embryos will then be removed and another person’s mitochondrial donation discarded. It will be replaced with the nuclear treatment so that they can avoid passing on genetic material removed from embryos created inheritable mitochondrial diseases to their using the intended mother’s eggs and father’s children. (or donor’s) sperm. This means that they, not you, will be the genetic parents of the child. If you’re unsure of anything, please ask your clinic for more information. You will be donating eggs (containing your mitochondria) to women who have mitochondria containing gene abnormalities, for use in IVF- based treatment so that they can avoid passing Before you fill in this form, you should have on an inheritable mitochondrial disease to their completed the ‘Mitochondrial Donor Registration child. -

Surviving Spouse Checklist
Surviving Spouse Checklist When your spouse dies, you may be faced with a dark shadow of grief, fear and uncertainty along with a flood of emotions that can make tasks like managing financial obligations seem almost impossible. At a time when you feel least able to cope with life, when you are low on mental and physical energy, there are many decisions to be made that can permanently affect your family, finances, livelihood, and much more. This checklist is designed to help those dealing with this challenging time keep the process organized and as easy to understand as possible. Funeral – Memorial Period: Veterans Affairs at 1-800-827-1000 or at: Follow directives if body or organ donation was http://www.cem.va.gov/bbene/benvba.asp pre-planned. Have someone at your house during the funeral if Contact a funeral home to make arrangements possible, since burglars read obituaries and for funeral preparations and payment. Order pre- funeral notices to target empty homes. printed “thank you” cards. Decide on cremation or burial if not pre-planned. Allow family to assist with food preparation, housekeeping tasks and care for young children, Contact friends and family who need to be if needed. informed about the death and services. Allow close friends and family to help with the contact Set up a system to keep track of and later of others. acknowledge cards, letters, phone calls, etc. Ask the funeral director to help you get at least Next action items: 12 certified copies of the death certificate, or contact the County Clerk’s office yourself to get If applicable, contact your spouse’s employer to them. -

DS-5511 Affidavit for the Surviving Spouse Or Next Of
U. S. Department of State CONSULAR OFFICES OF THE UNITED STATES OF AMERICA AFFIDAVIT FOR THE SURVIVING SPOUSE OR NEXT OF KIN *Provide information below to the extent that it is available. VENUE State ss. City I, being duly sworn according to law, declare that I reside at Your Name and that on Street Address (Including City, State/or Country) Date of Death (mm-dd-yyyy) had permanent legal residence at Name of Deceased . I am the Complete Address of the Deceased Specify: widow, widower, child, father, mother, sibling, other and as such am entitled to receive the decedent's estate under the laws of . To the best of my knowledge, Name of state/foreign state in the United States or foreign country where the deceased last had a permanent legal residence did/did not have a will or trust specifying the disposition of his or her estate. Name of Deceased NAME(S) OF SURVIVORS, IN ORDER OF KINSHIP Please insert the name of living relatives in the following order of relationship: surviving spouse, children, father and/or mother, brothers and/or sisters, other: Date of Birth Name (mm-dd-yyyy) Address Telephone Number Relationship DS-5511 Page 1 of 3 10-2008 Name Date of Birth Address Telephone Number Relationship Subscribed and sworn to before me by Signature of Affiant Type Name of Affiant Date (mm-dd-yyyy) Address of Notary Public Signature of Notary Public Type Name of Notary Public DS-5511 Page 2 of 3 PRIVACY ACT STATEMENT The information on this form is requested to assist U.S.