Improving the Health of a Population Through Collaborative Care
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Healthcare IT & Consulting
7 Mile Advisors Sectorwatch: Healthcare IT & Consulting Q3 2021 Healthcare IT & Consulting 7 Mile Advisors appreciates the opportunity to present this confidential information to the Company. This document is meant to be delivered only in conjunction with a verbal presentation, and is not authorized for distribution. Please see the Confidentiality Notice & Disclaimer at the end of the document. All data cited in this document was believed to be accurate at the time of authorship and came from publicly available sources. Neither 7 Mile Advisors nor 7M Securities make warranties or representations as to the accuracy or completeness of third-party data contained herein. This document should be treated 2 as confidential and for the use of the intended recipient only. Please notify 7 Mile Advisors if it was distributed in error. Overview DASHBOARD • Summary metrics on the sector • Commentary on market momentum by comparing the most recent 12-month performance against the last 3- year averages. PUBLIC BASKET PERFORMANCE • Summary valuation and operating metrics for a basket of We advise on M&A and private capital transactions and provide market comparable public companies. assessments and benchmarking. As a close-knit team with a long history together and a laser focus on our target markets, we help our clients sell their companies, raise capital, grow through acquisitions, and evaluate new markets. VALUATION COMPARISON We publish our sectorwatch, a review of M&A and operational trends in • Graphical, detailed comparison of valuation multiples -

Ehr Software Vendor Directory
EHR SOFTWARE VENDOR DIRECTORY 2017 Edition C M CONVERTED MEDIA 1ST PROVIDERS CHOICE 1st Providers Choice was set up in 1983 and was developed by a private company of the same name operating out of headquarters in Chandler, Arizona. Customers of the 1st Providers Choice EHR include foot clinics, allergy and asthma centers and chiropractors. Customers of the 1st Providers Choice EHR include foot clinics, allergy and asthma centers and chiropractors. 1st Providers Choice EHR - An EHR software system with templates suitable for a wide variety of practice specialties. ADVANCEDMD AdvancedMD, previously ADP AdvancedMD, is an EHR provider owned by Marlin Equity Partners, trading as a standalone company. AdvancedMD offers fully integrated EHR, practice management, and patient relationship management software solutions, as well as data reporting and business intelligence tools for us in all areas of a practice. AdvancedMD EHR provides a complete healthcare solution for practices of any size. Their products are cloud-based, mobile accessible but can also be installed as desktop only. AdvancedMD EHR - AdvancedMD EHR provides a complete, cloud-based healthcare solution for practices of any size which can be accessed on mobile or desktop devices. ALLERGY EHR Allergy EHR is developed and marketing by Meditab Software which is based in northern California. The company was founded in 1998 by practicing pharmacists and physicians and offers health information management services in North America and Canada. Current users of Allergy EHR include the Allergy & Asthma Center of Texas, and the Advanced Allergy & Asthma Associates Crystal Lake. Allergy EHR - A cloud based EHR software designed specifically for the allergy and immunology sector. -

Software & Services
SOFTWARE & SERVICES Recognizing the software and service organizations that excelled in helping providers deliver better patient care PHYSICIAN PRACTICE SOLUTIONS BEST IN KLAS AMBULATORY EMR (1–10 PHYSICIANS) HOW DO VENDOR SOLUTIONS COMPARE? WHO IS KONFIDENCE SCORE TREND LEVEL 1. Cerner PowerChart Ambulatory BEST IN KLAS? 84.3 +13% üü 2. Amazing Charts 83.3 +4% üüü 3. SRSsoft EHR 81.0 -11% üü 4. athenahealth athenaClinicals 80.9 -7% üüü 5. Greenway PrimeSUITE Chart 79.1 -2% üüü HOW DO THEY SCORE? 6. Aprima EHR IN FIVE KEY PERFORMANCE CATEGORIES 78.2 -1% üüü 100 92.4 7. ADP AdvancedMD EHR +3% üüü 90 84.9 78.0 80.6 81.7 81.2 80 8. e-MDs Chart -13% üüü 70 74.0 60 AVG. SEGMENT MKT. 9. GE Healthcare Centricity Practice Solution EMR +1% üü PHYSICIAN PRACTICE PHYSICIAN 50 73.8 40 T10. eClinicalWorks EHR 73.4 -7% üüü 30 20 T10. Henry Schein MicroMD EMR 73.4 +4% üü 10 12. NextGen Healthcare EHR 0 65.1 -3% üüü SALES & FUNCTIONALITY GENERAL CONTRACTING & UPGRADES 13. Allscripts Professional EHR 64.7 -6% üüü SERVICE & IMPLEMENTATION SUPPORT 14. McKesson Practice Partner -14% & TRAINING 48.0 üü 0 10 20 30 40 50 60 70 80 90 100 SEE HOW OTHER VENDOR SOLUTIONS SCORE AT KLASRESEARCH.COM HOW DO THE TOP THREE SOLUTIONS TREND? SOLUTIONS NOT RANKED PRELIMINARY DATA PRODUCTS CompuGroup Medical Enterprise EHR (HEHR)*..................71.0 MIE WebChart EMR* ............................................................75.7 MTBC EMR* .........................................................................82.1 Optum Physician EMR* ........................................................79.6 -

MENTAL HEALTH EMR SOFTWARE May 2017
MENTAL HEALTH EMR SOFTWARE May 2017 ¨ CONTENTS 4 Introduction 6 Defning Mental Health EMR Software 7 The Quadrant 8 Mental Health EMR FrontRunners Index 32 Runners Up 35 Methodology Basics FRONTRUNNERS 9 NextGen Healthcare 10 Intelligent Medical Software 11 Kareo 12 AdvancedMD EHR 13 PrognoCIS 14 drchrono 15 MediTouch EHR 16 NueMD 17 Compulink 18 Antworks 19 RxNT Suite 20 Sevocity EHR 21 SOAPware 22 Azalea Health 23 ReLiMed 24 EHR 24/7 25 InSync EMR 26 CureMD 27 Valant 28 TotalMD 29 CareLogic Enterprise 30 ICANotes 31 PIMSY INTRODUCTION his FrontRunners analysis is a data-driven Tassessment identifying products in the Mental Health EMR market that ofer the best capability and value for small businesses. For a given market, products are evaluated and given a score for the capability (x-axis) and value (y-axis) they bring to users. FrontRunners then plots the top 25-30 products in a quadrant format. In the Mental Health EMR FrontRunners graphic, the Capability axis starts at 2.80 and ends at 4.40, while the Value axis starts at 3.00 and ends at 4.60. To be considered for the Mental Health EMR FrontRunners, a product needed a minimum of 10 user reviews, a minimum capability user rating score of 2.5 and a minimum value user rating score of 2.0. In most cases, we evaluate hundreds of products and feature 20-25 as FrontRunners; all products that qualify as FrontRunners are top performing products in their market. MAY 2017 4 I NTRODUCTION Each product falls within a designated quadrant based on their axis scores. -
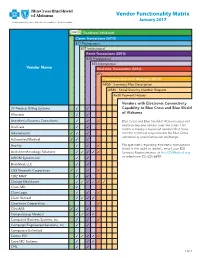
Vendor Functionality Matrix January 2017 an Independent Licensee of the Blue Cross and Blue Shield Association
Vendor Functionality Matrix January 2017 An Independent Licensee of the Blue Cross and Blue Shield Association Readiness Validated Claims Transactions (5010) 837 Professional 837 Institutional Remit Transactions (5010) 835 Professional 835 Institutional Vendor Name Real-time Transactions (5010) 27x Proprietary Real-time Messages (5010) AB50 - Summary Plan Description AB80 - Social Security Number Request Ax20 Payment History Vendors with Electronic Connectivity 2K Medical Billing Systems 3 3 Capability to Blue Cross and Blue Shield of Alabama Allscripts 3 3 Anesthesia Business Consultants 3 3 3 Blue Cross and Blue Shield of Alabama does not endorse any one vendor over the other. This AnviCare 3 3 matrix is merely a record of vendors that have Athenahealth 3 3 3 met the technical requirements for Blue Cross connectivity and information exchange. Automated Medical 3 3 3 Availity 3 3 3 For questions regarding electronic transactions listed in the table to the left, email your EDI Avid Anesthesiology Solutions 3 3 3 3 3 Services Representative at [email protected] AXIOM Systems Inc. 3 3 or telephone 205-220-6899. BrickMed, LLC 3 3 C&S Research Corporation 3 3 3 3 CBIZ MMP 3 3 Change Healthcare 3 3 3 3 3 3 Claim.MD 3 ClaimLogic 3 3 3 Claim Remedi 3 3 3 3 Clearwave Corporation 3 ClinixMIS 3 3 3 CompuGroup Medical 3 3 3 3 Compulink Business Systems, Inc. 3 3 3 Computer Engineered Solutions, Inc. 3 3 Computers Unlimited Cortex EDI 3 3 3 3 3 Cove MD Systems 3 3 3 CPU 3 3 1 of 4 Readiness Validated Claims Transactions (5010) 837 Professional 837 Institutional Remit Transactions (5010) 835 Professional 835 Institutional Vendor Name Real-time Transactions (5010) 27x Proprietary Real-time Messages (5010) AB50 - Summary Plan Description AB80 - Social Security Number Request Ax20 Payment History Creative Concepts in Communications 3 3 Custom Software Systems, Inc. -

Top 20 Ehr Software
TOP 20 EHR SOFTWARE C M CONVERTED MEDIA TOP 20 EHR SOFTWARE 1 AdvancedMD AdvancedEHR 11 Allscripts Allscripts Professional EHR 2 Cerner Cerner Ambulatory EHR 12 CareCloud CareCloud Charts 3 athenahealth athenahealth EHR 13 CureMD All in One EHR 4 Epic Epic EHR 14 Practice Velocity VelociDoc EHR Azalea Health 5 Practice Fusion Practice Fusion EHR 15 Azalea EHR Innovations 6 Kareo Kareo Clinical 16 ReLi Med Solutions ReLiMed EMR 7 Henry Schein MicroMD EMR 17 MedEZ MedEZ 8 drchrono drchrono EHR 18 iSALUS Healthcare OfficeEMR 9 NextGen Healthcare NextGen Healthcare EHR 19 ChartLogic ChartLogic EMR Modernizing 10 EMA 20 ICANotes ICANotes EHR Medicine C M CONVERTED MEDIA EHR IN PRACTICE HOW THESE RANKINGS WERE GENERATED This ranking was determined using a number of factors including industry standing, public opinion of software, social media presence, and available software features relevant to the needs of a small business. This ranking should serve as a rough estimate of software suitability, and more in-depth analysis can be taken below or by using our EHR software comparison. C M CONVERTED MEDIA SHORTLISTING EHR VENDORS CHECKLIST Research EHR employed by similar sized practices in 1 6 Produce an RFI document and send to vendor shortlist the same specialty Identify market leading solutions which offer some 2 7 Narrow shortlist based on RFI responses support in your specialty Leverage professional network for recommendations Compile requirements and business processes in an 3 8 based on their experience RFP document Narrow shortlist based -

J.P. Morgan Healthcare Conference January 2011 Safe Harbor Provisions
J.P. Morgan Healthcare Conference January 2011 Safe Harbor Provisions SAFE HARBOR PROVISIONS FOR FORWARD-LOOKING STATEMENTS: Statements made during this presentation, the proxy statements filed with the Securities and Exchange Commission (“Commission”), communications to shareholders, press releases and oral statements made by our representatives that are not historical in nature, or that state our or management’s intentions, hopes, beliefs, expectations or predictions of the future, may constitute “forward-looking statements” within the meaning of Section 21E of the Securities and Exchange Act of 1934, as amended. Forward-looking statements can often be identified by the use of forward-looking terminology, such as “could,” “should,” “will,” “will be,” “will lead,” “will assist,” “intended,” “continue,” “believe,” “may,” “expect,” “hope,” “anticipate,” “goal,” “forecast,” “plan,” or “estimate” or variations thereof or similar expressions. Forward-looking statements are not guarantees of future performance. Forward-looking statements involve risks, uncertainties and assumptions. It is important to note that any such performance and actual results, financial condition or business, could differ materially from those expressed in such forward-looking statements. Factors that could cause or contribute to such differences include, but are not limited to, the risk factors discussed under “Risk Factors” in our Annual Report on Form 10-K for fiscal year ended March 31, 2010, as well as factors discussed elsewhere in other reports and documents we file with the Commission. Other unforeseen factors not identified herein could also have such an effect. We undertake no obligation to update or revise forward-looking statements to reflect changed assumptions, the occurrence of unanticipated events or changes in future operating results, financial condition or business over time unless required by law. -

Small Practice Ambulatory Emr/Pm (10 Or Fewer Physicians) 2019
SMALL PRACTICE AMBULATORY EMR/PM (10 OR FEWER PHYSICIANS) 2019 BUILDING STRONG FOUNDATIONS FOR CUSTOMER SUCCESS ® %/ Performance Report | January 2019 DRILL DEEPER TABLE OF CONTENTS 2 Executive Insights 6 Expanded Insights 29 Vendor Insights 31 AdvancedMD 45 eClinicalWorks 33 Allscripts 47 eMDs 35 Aprima 49 Greenway Health 37 athenahealth 51 Kareo 39 CareCloud 53 NextGen Healthcare 41 Cerner 55 Virence Health (GE Healthcare) 43 CureMD 57 Data Index 68 Vendor Executive Interview Details 1 EXECUTIVE INSIGHTS SMALL PRACTICE AMBULATORY EMR/PM (10 OR FEWER PHYSICIANS) 2019 BUILDING STRONG FOUNDATIONS FOR CUSTOMER SUCCESS As healthcare has moved beyond meaningful use, small practices have begun to expect more from their vendors and to look for EMRs that do more than meet basic regulatory requirements. As a result, EMR/PM satisfaction among small practices (10 or fewer physicians) has varied greatly over the past year—scores for a number of vendors have swung more than 10 percentage points (some positively, some negatively). To explore what the future holds for this market, KLAS spoke to hundreds of small practice customers about their EMR/PM experiences and needs and also interviewed executives and representatives from AdvancedMD, Allscripts, Aprima, athenahealth, Azalea Health, CareCloud, Cerner, CureMD, eMDs, Greenway Health, Kareo, NextGen, Quest Diagnostics, and Virence Health (GE Healthcare) to find out how these vendors plan to increase customer satisfaction going forward. What Are the Most Important Vendor/ NextGen Healthcare, CureMD, and Aprima Product Attributes for Small Practices? Most Aligned to Deliver Customer Success (n=57) The green bars represent the total tallies after New 7 Technology each need was weighted When asked to name the top things EMR/PM vendors should focus based on whether the respondent ranked it first, on, small practices overwhelmingly say that before addressing more Advanced Needs second, or third. -

Clinical Integration Through Electronic Data Interchange
VENDOR LIST Clinical Integration Through Electronic Data Interchange As of July 2021 As of July 2021 Vendor Name Vendor Name Vendor Name 4Medica CareCloud DataLink LLC Accumedic Computer Systems CareHere-Champ IT Solutions DataTel Solutions ACE Health Solutions, LLC CareSpan USA Inc DaVinci Technology Acumen Physician Solutions Cascades Clinical Systems, Inc. DaVita Acurus Solutions Centura Health Corporate DavLong Business Solutions, LLC ADL Data Systems Cerner Corp DigiDMS Advanced Data Systems Corp Change Healthcare Digital MD Systems Advanced Technologies Group ChartLogic DocComply AdvancedMD Software ChartPerfect, Inc Doctor On Demand Agastha ChenMed DoctorWellington Ageology, Inc. ChiroTouch DocuTrac AllegianceMD Software Inc ClaimPower, Inc. Dr J Exceptional Medicine AllMeds, Inc ClinicTracker JAG DrChrono Allscripts Clinlab Drscribe American Medical Software Clovi DrugPak LLC American Medical Solutions CoCENTRIX Echo Group Anagen Systems CodoniX eClinicalWorks Angel Systems, Inc. Community Computer Service, Inc. eData Platform Ankhos Oncology Software, LLC Complete Healthcare Solutions, Inc EHealthLine.com, Inc. AntWorks Complete Medical Solutions, Inc. eHealthObjects, Inc AP Easy Software Solutions CompuGroup Medical EHR Your Way Apex Energetics CompuLink Business Systems Elation Health Apex Healthware Computalogic ELEKTA IMPAC Medical Systems Aprima Computer Service & Support Ellkay Aragon Development Comtron eMD Office.com Arise Lab, LLC Conceptual Mindworks eMDs Artisan Medical Solutions Confluence Health Systems LLC eMedical -

Ehr Software Vendor Directory
EHR SOFTWARE VENDOR DIRECTORY 2017 Edition C M CONVERTED MEDIA OVERVIEW CONTACT ADP acquired AdvancedMD, an established provider of EHR solutions for private practice healthcare environments in 2011. ADP AdvancedMD With ADP, the AdvancedMD product offerings have expanded to include an enhanced in-house billing suite, medical coding 10876 S River Front Pkwy capabilities and integration with outsourced medical billing providers. Suite 400 South Jordan ADP AdvancedMD EHR provides functionality for medical practices as well as components designed for administrative and UT billing use. 84095 United States For medical practices, ADP AdvancedMD EHR provides a patient portal for admissions and check-ins alongside document 800-825-0224 management, e-prescriptions and more. All of this is available as a mobile platform on iOS devices. [email protected] Role-based access to the EHR for nurses and physicians improves workflow by limiting system complexity for each role. During the medical coding and billing phase, there are options to present the information for in-house coders or to integrate it with the API from an outsourced medical billing company. The ADP AdvancedMD EHR and revenue cycle management solutions are available to clients via a tiered subscription access program. There is an initial installation and training fee, and then clients may select “a-la-carte” options for their subscription package that are best suited to their practice. COMPARE ADP ADVANCEDMD EHR & MANY MORE ADP AdvancedMD EHR provides a complete healthcare solution for practices of any size. Their products are cloud based, Compare software features, mobile accessible but can also be installed as desktop only. -

Nextgen Healthcare Nextgen Ambulatory EHR, Version 5.9
DocuSign Envelope ID: FA9CA56C-9075-4A65-B060-A42739CB9D51 NextGen Healthcare NextGen Ambulatory EHR, version 5.9 Robert Murry, MD Chief Medical Informatics Officer NextGen Healthcare 18111 Von Karman Avenue Irvine, CA 92612 For public release: NextGen Healthcare attests that the usability standard/process and usability report submitted for the certification of NextGen Ambulatory EHR, version 5.9 is accurate and complete per the requirements of the ONC criterion 170.315(g)(3). Robert Murry, MD Chief Medical Informatics Officer DocuSign Envelope ID: FA9CA56C-9075-4A65-B060-A42739CB9D51 NextGen Healthcare NextGen Ambulatory EHR version 5.9 Robert Murry, MD Chief Medical Informatics Officer NextGen Healthcare 18111 Von Karman Avenue Irvine, CA 92612 For public release: NextGen Healthcare used the following usability design industry standard in developing and designing their health IT module, NextGen Ambulatory EHR, version 5.9: NISTIR 7741. National Institute of Standards and Technology. (2010). NIST Guide to the Processes Approach for Improving the Usability of Electronic Health Records (NISTIR 7741). Gaithersburg, MD. http://ws680.nist.gov/publication/get_pdf.cfm?pub_id=907313 Per the National Institute of Standards and Technology (NIST) Guide to the Processes Approach for Improving the Usability of Electronic Health Records, EHRs should support a process that provides a high level of usability for all users. The goals are for users to interact with the system safely, effectively, efficiently, and with an acceptable level of satisfaction. -

Nextgen Healthcare Annual Report 2020
NextGen Healthcare Annual Report 2020 Form 10-K (NASDAQ:NXGN) Published: June 1st, 2020 PDF generated by stocklight.com UNITED STATES SECURITIES AND EXCHANGE COMMISSION Washington, D.C. 20549 FORM 10-K ☑ ANNUAL REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 For the fiscal year ended March 31, 2020 or ☐ TRANSITION REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 Commission file number: 001-12537 NEXTGEN HEALTHCARE, INC. (Exact name of registrant as specified in its charter) California 95-2888568 (State or other jurisdiction of incorporation or organization) (IRS Employer Identification No.) 18111 Von Karman Avenue, Suite 800, Irvine, California 92612 (Address of principal executive offices) (Zip Code) (949) 255-2600 (Registrant’s telephone number, including area code) Securities registered pursuant to Section 12(b) of the Act: Title of each class Trading Symbol Name of each exchange on which registered Common Stock, $0.01 Par Value NXGN NASDAQ Global Select Market Securities registered pursuant to Section 12(g) of the Act: None Indicate by check mark if the registrant is a well-known seasoned issuer, as defined in Rule 405 of the Securities Act. Yes ☑ No ☐ Indicate by check mark if the registrant is not required to file reports pursuant to Section 13 or Section 15(d) of the Act. Yes ☐ No ☑ Indicate by check mark whether the registrant (1) has filed all reports required to be filed by Section 13 or 15(d) of the Securities Exchange Act of 1934 during the preceding 12 months (or for such shorter period that the registrant was required to file such reports), and (2) has been subject to such filing requirements for the past 90 days.