Medicinal Product No Longer Authorised
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Metformin Plus Saxagliptin for Type 2 Diabetes
Treatment evaluation Metformin plus saxagliptin for type 2 diabetes André J. Scheen Division of Diabetes, Nutrition and Metabolic Disorders and Division of Clinical Pharmacology, Department of Medicine, CHU Sart Tilman, University of Liège, Liège, Belgium Running title : Saxagliptin plus metformin Word count : Abstract : 148 Main text : 2404 Tables : 4 Figures : 0 Address for correspondence : Pr André J. SCHEEN Department of Medicine CHU Sart Tilman (B35) B-4000 LIEGE 1 BELGIUM Phone : 32-4-3667238 FAX : 32-4-3667068 Page 1 Email : andre.scheen @ chu.ulg.ac.be SUMMARY Metformin is considered as the first-line drug therapy for the management of type 2 diabetes. Dipeptidyl peptidase-4 (DPP-4) inhibitors, by promoting insulin secretion and reducing glucagon secretion in a glucose-dependent manner, offer new opportunities for oral therapy after failure of metformin. Saxagliptin, a DPP-4 inhibitor, and metformin may be administered together, separately or in fixed-dose combination (FDC), either as saxagliptin added to metformin or as initial combination in drug-naive patients. Both compounds exert complementary pharmacodynamic actions leading to better improvement in blood glucose control (fasting plasma glucose, postprandial glucose, HbA1c) than either compound separately. Adding saxagliptin to metformin monthotherapy results in a consistent, sustained and safe reduction in HbA1c levels. Tolerance is excellent without hypoglycemia or weight gain. The combination saxaglitpin plus metformin may be used as first-line or second-line therapy in the management of type 2 diabetes, especially as a valuable alternative to the classical metformin-sulfonylurea combination. Key-words : DPP-4 inhibitor – Fixed-dose combination - Metformin – Saxagliptin - Type 2 diabetes mellitus Page 2 1. -

CD26/DPP-4: Type 2 Diabetes Drug Target with Potential Influence On
cancers Review CD26/DPP-4: Type 2 Diabetes Drug Target with Potential Influence on Cancer Biology Emi Kawakita 1 , Daisuke Koya 2,3 and Keizo Kanasaki 1,3,* 1 Internal Medicine 1, Shimane University Faculty of Medicine, 89-1 Enya-cho, Izumo 693-8501, Japan; [email protected] 2 Department of Diabetology & Endocrinology, Kanazawa Medical University, Uchinada 920-0293, Japan; [email protected] 3 Division of Anticipatory Molecular Food Science and Technology, Medical Research Institute, Kanazawa Medical University, Uchinada 920-0293, Japan * Correspondence: [email protected]; Tel.: +81-853-20-2183 Simple Summary: Dipeptidyl peptidase (DPP)-4 inhibitor is widely used for type 2 diabetes. Al- though DPP-4/CD26 has been recognized as both a suppressor and inducer in tumor biology due to its various functions, how DPP-4 inhibitor affects cancer progression in diabetic patients is still unknown. The aim of this review is to summarize one unfavorable aspect of DPP-4 inhibitor in cancer-bearing diabetic patients. Abstract: DPP-4/CD26, a membrane-bound glycoprotein, is ubiquitously expressed and has diverse biological functions. Because of its enzymatic action, such as the degradation of incretin hormones, DPP-4/CD26 is recognized as the significant therapeutic target for type 2 diabetes (T2DM); DPP- 4 inhibitors have been used as an anti-diabetic agent for a decade. The safety profile of DPP-4 inhibitors for a cardiovascular event in T2DM patients has been widely analyzed; however, a clear association between DPP-4 inhibitors and tumor biology is not yet established. Previous preclinical Citation: Kawakita, E.; Koya, D.; Kanasaki, K. -

Komboglyze, INN-Saxagliptin, Metformin
ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS 1. NAME OF THE MEDICINAL PRODUCT Komboglyze 2.5 mg/850 mg film-coated tablets Komboglyze 2.5 mg/1,000 mg film-coated tablets 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Komboglyze 2.5 mg/850 mg film-coated tablets Each tablet contains 2.5 mg of saxagliptin (as hydrochloride) and 850 mg of metformin hydrochloride. Komboglyze 2.5 mg/1,000 mg film-coated tablets Each tablet contains 2.5 mg of saxagliptin (as hydrochloride) and 1,000 mg of metformin hydrochloride. For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Film-coated tablet (tablet). Komboglyze 2.5 mg/850 mg film-coated tablets Light brown to brown, biconvex, round, film-coated tablets, with “2.5/850” printed on one side and “4246” printed on the other side, in blue ink. Komboglyze 2.5 mg/1,000 mg film-coated tablets Pale yellow to light yellow, biconvex, oval shaped, film-coated tablets, with “2.5/1000” printed on one side and “4247” printed on the other side, in blue ink. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Komboglyze is indicated in adults with type 2 diabetes mellitus as an adjunct to diet and exercise to improve glycaemic control: in patients inadequately controlled on their maximally tolerated dose of metformin alone in combination with other medicinal products for the treatment of diabetes, including insulin, in patients inadequately controlled with metformin and these medicinal products (see sections 4.4, 4.5 and 5.1 for available data on different combinations) in patients already being treated with the combination of saxagliptin and metformin as separate tablets. -

AVANDIA (Rosiglitazone Maleate Tablets), for Oral Use Ischemic Cardiovascular (CV) Events Relative to Placebo, Not Confirmed in Initial U.S
HIGHLIGHTS OF PRESCRIBING INFORMATION ----------------------- WARNINGS AND PRECAUTIONS ----------------------- These highlights do not include all the information needed to use • Fluid retention, which may exacerbate or lead to heart failure, may occur. AVANDIA safely and effectively. See full prescribing information for Combination use with insulin and use in congestive heart failure NYHA AVANDIA. Class I and II may increase risk of other cardiovascular effects. (5.1) • Meta-analysis of 52 mostly short-term trials suggested a potential risk of AVANDIA (rosiglitazone maleate tablets), for oral use ischemic cardiovascular (CV) events relative to placebo, not confirmed in Initial U.S. Approval: 1999 a long-term CV outcome trial versus metformin or sulfonylurea. (5.2) • Dose-related edema (5.3) and weight gain (5.4) may occur. WARNING: CONGESTIVE HEART FAILURE • Measure liver enzymes prior to initiation and periodically thereafter. Do See full prescribing information for complete boxed warning. not initiate therapy in patients with increased baseline liver enzyme levels ● Thiazolidinediones, including rosiglitazone, cause or exacerbate (ALT >2.5X upper limit of normal). Discontinue therapy if ALT levels congestive heart failure in some patients (5.1). After initiation of remain >3X the upper limit of normal or if jaundice is observed. (5.5) AVANDIA, and after dose increases, observe patients carefully for signs • Macular edema has been reported. (5.6) and symptoms of heart failure (including excessive, rapid weight gain; • Increased incidence of bone fracture was observed in long-term trials. dyspnea; and/or edema). If these signs and symptoms develop, the heart (5.7) failure should be managed according to current standards of care. -

Type 2 Diabetes Adult Outpatient Insulin Guidelines
Diabetes Coalition of California TYPE 2 DIABETES ADULT OUTPATIENT INSULIN GUIDELINES GENERAL RECOMMENDATIONS Start insulin if A1C and glucose levels are above goal despite optimal use of other diabetes 6,7,8 medications. (Consider insulin as initial therapy if A1C very high, such as > 10.0%) 6,7,8 Start with BASAL INSULIN for most patients 1,6 Consider the following goals ADA A1C Goals: A1C < 7.0 for most patients A1C > 7.0 (consider 7.0-7.9) for higher risk patients 1. History of severe hypoglycemia 2. Multiple co-morbid conditions 3. Long standing diabetes 4. Limited life expectancy 5. Advanced complications or 6. Difficult to control despite use of insulin ADA Glucose Goals*: Fasting and premeal glucose < 130 Peak post-meal glucose (1-2 hours after meal) < 180 Difference between premeal and post-meal glucose < 50 *for higher risk patients individualize glucose goals in order to avoid hypoglycemia BASAL INSULIN Intermediate-acting: NPH Note: NPH insulin has elevated risk of hypoglycemia so use with extra caution6,8,15,17,25,32 Long-acting: Glargine (Lantus®) Detemir (Levemir®) 6,7,8 Basal insulin is best starting insulin choice for most patients (if fasting glucose above goal). 6,7 8 Start one of the intermediate-acting or long-acting insulins listed above. Start insulin at night. When starting basal insulin: Continue secretagogues. Continue metformin. 7,8,20,29 Note: if NPH causes nocturnal hypoglycemia, consider switching NPH to long-acting insulin. 17,25,32 STARTING DOSE: Start dose: 10 units6,7,8,11,12,13,14,16,19,20,21,22,25 Consider using a lower starting dose (such as 0.1 units/kg/day32) especially if 17,19 patient is thin or has a fasting glucose only minimally above goal. -
Taking Metformin for Gestational Diabetes This Information Sheet Will Help You Understand More About Taking Metformin for Gestational Diabetes
Taking metformin for gestational diabetes This information sheet will help you understand more about taking metformin for gestational diabetes. This information sheet is not a substitute for talking with your midwife, doctor, nurse or pharmacist. Gestational diabetes Risks for your baby: Gestational diabetes means you have too much • may grow larger than normal (this increases the glucose (a type of sugar) in your blood when you risk of injury during birth) are pregnant. Insulin controls the amount of • born too early (premature) glucose in your blood. Sometimes you don’t make • low blood glucose after birth enough insulin or it doesn’t work as well when you are pregnant. • may need treatment in hospital • jaundice (yellow skin) that needs treatment Gestational diabetes is common. Up to eight pregnant women in every 100 get gestational • breathing problems. diabetes. Taking metformin helps reduce these risks. It can be hard to tell if you have gestational You can see how many women and babies are diabetes. Some women find that they: affected and how treatment helps in the picture • lack energy on the next page. • feel thirsty a lot • go to the toilet a lot Metformin is safe to take for • get lots of infections. gestational diabetes Metformin has been tested in clinical studies and Some women have no symptoms. This is why all is safe to take for gestational diabetes. pregnant women are tested for diabetes so they Metformin helps keep both your weight gain and can get treatment. blood pressure down. Metformin The main side effect is stomach upsets such as Metformin is a medicine that has been used feeling sick and diarrhoea. -
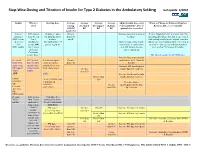
Step-Wise Dosing and Titration of Insulin for Type 2 Diabetes in the Ambulatory Setting Last Update 5/2010
Step -Wise Dosing and Titration of Insulin for Type 2 Diabetes in the Ambulatory Setting last update 5/2010 Insulin When to Starting dose Average Average Average Average Adjust Insulin dose every When to Change to Different Regimen start fasting Pre-lunch Pre-supper Bedtime 3 days until BG < 130, or Recheck A1C every 3 months AM BG BG BG BG optimal dose is reached Goal<130 Lantus A1C greater 10 units or up to Greater Increase dose by 2-4 units at If after 3 months if A1c is greater than 7% (glargine) than 8% on 0.2 units/kg SQ at than 130 bedtime. and optimal bedtime dose has been reached OR Levemir 2 or 3 bedtime mg/dL with fasting blood glucose at goal, consider (detemir) antidiabetic (DC sulfonylurea if Optimal long acting (basal) adding a pre-meal bolus insulin at the largest OR agents OR part of regimen) insulin dose keeps bedtime meal of the day, pre-meal bolus insulin at NPH insulin 1 or 2 agents and AM fasting glucose each meal or 70/30 premix insulin. if Serum values consistent. Creatinine greater than 2 DC all oral agents except Metformin. Increase long acting (basal) Pre-meal A1C greater 2-4 units of rapid Greater insulin dose by 2-4 units at bolus with than 7% with acting or regular than 130 bedtime rapid acting optimal long insulin SQ at each Increase AM rapid/regular OR regular acting (basal) meal (base dose) Greater insulin dose by 2-4 units. insulin insulin. than 130 AND with Increase lunch rapid/regular Greater than insulin dose by 2-4 units. -

KOMBIGLYZE XR Safely and Effectively
HIGHLIGHTS OF PRESCRIBING INFORMATION ------------------------WARNINGS AND PRECAUTIONS----------------------- These highlights do not include all the information needed to use Lactic acidosis: Warn patients against excessive alcohol intake. KOMBIGLYZE XR safely and effectively. See full prescribing KOMBIGLYZE XR not recommended in hepatic impairment and information for KOMBIGLYZE XR. contraindicated in renal impairment. Ensure normal renal function KOMBIGLYZE XR (saxagliptin and metformin HCl extended-release) before initiating and at least annually thereafter. Temporarily tablets discontinue KOMBIGLYZE XR in patients undergoing radiologic Initial U.S. Approval: 2010 studies with intravascular administration of iodinated contrast materials or any surgical procedures necessitating restricted intake of food and WARNING: LACTIC ACIDOSIS fluids. (4, 5.1, 5.3, 5.4, 5.7, 5.10, 5.11) See full prescribing information for complete boxed warning. There have been postmarketing reports of acute pancreatitis in patients Lactic acidosis can occur due to metformin accumulation. The taking saxagliptin. If pancreatitis is suspected, promptly discontinue risk increases with conditions such as sepsis, dehydration, excess KOMBIGLYZE XR. (5.2) alcohol intake, hepatic impairment, renal impairment, and acute Vitamin B12 deficiency: Metformin may lower vitamin B12 levels. congestive heart failure. (5.1) Measure hematological parameters annually. (5.5, 6.1) Symptoms include malaise, myalgias, respiratory distress, Hypoglycemia: When used with an insulin -

Mechanism of Action Pharmacokinetics
NDA 21-748/S-002 Page 3 Glumetza ™, 500 mg (metformin hydrochloride extended release tablets) tablet, film coated, extended release DESCRIPTION GLUMETZA (metformin hydrochloride) extended release tablet is an oral antihyperglycemic drug used in the management of type 2 diabetes. Metformin hydrochloride (N,N- dimethylimidodicarbonimidic diamide hydrochloride) is not chemically or pharmacologically related to any other classes of oral antihyperglycemic agents. The structural formula of metformin hydrochloride (metformin HCl) is as shown: Metformin HCl is a white to off-white crystalline compound with a molecular formula of C4H11N5•HCl and a molecular weight of 165.63. Metformin HCl is freely soluble in water and is practically insoluble in acetone, ether, and chloroform. The pKa of metformin is 12.4. The pH of a 1% aqueous solution of metformin hydrochloride is 6.68. GLUMETZA tablets are modified release dosage forms that contain 500 mg or 1000 mg of metformin HCl. Each 500 mg tablet contains coloring, hypromellose, magnesium stearate, microcrystalline cellulose and polyethylene oxide. Each 1000 mg tablet contains crospovidone, dibutyl sebacate, ethylcellulose, glyceryl behenate, polyvinyl alcohol, polyvinylpyrrolidone, and silicon dioxide. GLUMETZA 500 and 1000 mg tablets both utilize polymer- based, oral drug delivery systems, which allow delivery of metformin HCl to the upper gastrointestinal (GI) tract. CLINICAL PHARMACOLOGY Mechanism of Action Metformin is an antihyperglycemic agent, which improves glucose tolerance in patients with type 2 diabetes, lowering both basal and postprandial plasma glucose. Its pharmacologic mechanisms of action are different from other classes of oral antihyperglycemic agents. Metformin decreases hepatic glucose production, decreases intestinal absorption of glucose, and improves insulin sensitivity by increasing peripheral glucose uptake and utilization. -

Competact. INN: Pioglitazone & Metformin
SCIENTIFIC DISCUSSION 1. Introduction Type 2 diabetes mellitus is a heterogeneous disorder characterised by multiple defects in the pancreatic β-cell, liver, and peripheral tissues such as skeletal muscle and adipose tissue. There is considerable debate about the primacy of insulin resistance or beta cell failure in the disorder. It is well documented that three major metabolic abnormalities contribute to the development of hyperglycaemia in type 2 diabetes mellitus, including impaired insulin secretion in response to glucose, increased hepatic glucose production, and decreased insulin-dependent glucose uptake in the peripheral tissues. The latter two abnormalities are defined as insulin resistance. Insulin resistance is reversed by enhancing the action of insulin, thereby promoting glucose utilisation in peripheral tissues, suppressing gluconeogenesis in the liver, and reducing lipolysis at the adipocyte. Insulin resistance appears in early stages of the disease. It is a major factor in the progression of the disease, contributing to beta cell exhaustion due to demands on insulin secretion. The prolonged hyperglycaemia, which results from the metabolic defects causes microvascular and macrovascular damage, which is a cause of considerable morbidity and mortality. The prevalence of type 2 diabetes in Europeans is at least 2-3 % and increases substantially in those older than 70 years. Microvascular (retinopathy, nephropathy and neuropathy) and macrovascular complications (e.g., ischemic heart disease) of diabetes are common. Microvascular complications appear to be related to hyperglycaemia. Macrovascular complications are more related to dyslipidaemia and blood pressure control. The main goal of treatment for type 2 diabetes is to prevent acute and chronic complications, through better control of blood glucose levels and the management of macrovascular risk factors associated to diabetes (dyslipidaemia, blood pressure control and central obesity). -

Diabetes Medication: Metformin
FACT SHEET FOR PATIENTS AND FAMILIES Diabetes Medication: Metformin What is metformin? Metformin [met-FORE-min] is a medication that is used to treat type 2 diabetes and insulin resistance. Metformin is taken orally (by mouth) as a pill. Like other diabetes medications, it works best when you follow the rest of your treatment plan. This means checking your blood glucose regularly, following your meal plan, and exercising every day. What does it do? Metformin helps lower your blood glucose (blood sugar). It does this by: • Decreasing the amount of glucose released by your Does metformin cause hypoglycemia liver. Less glucose enters your bloodstream. (low blood glucose)? • Increasing the ability of your muscles to use glucose No. Metformin doesn’t cause hypoglycemia by itself. for energy. As more glucose is used, more glucose But combined with other medications, vigorous leaves your bloodstream. exercise, or too little food, it can make your blood glucose drop too low. Why is metformin important for my health? Since low blood glucose can be dangerous, make sure that you and your family know the symptoms. These Metformin can’t cure your diabetes. But, by helping include feeling shaky, sweaty, hungry, and irritable. control your blood glucose, it lowers the chance that If you have these symptoms, take some quick-acting your diabetes will cause serious problems. sugar. Good sources are 3 or 4 glucose tablets, a half- When you have diabetes, you tend to have high blood cup of fruit juice or regular soda, or a tablespoon of glucose. Over time, this can damage your blood honey or sugar. -

Metformin Hydrochloride (Glucophage) Patient Information, EDI
Metformin Hydrochloride (Glucophage) Patient Information, EDI Definitions: Metformin (Glucophage) is a medication designed to lower blood sugar levels. Indications: Metformin is indicated, in addition to weight reduction and a sensible diet, to lower blood glucose levels in patients with Type II Non-Insulin-Dependent Diabetes Mellitus (NIDDM). While not FDA approved for this indication, Metformin may help patients with Poly Cystic Ovarian Syndrome (PCOS) control elevated insulin (insulin resistance) and glucose (glucose intolerance) levels. The excess insulin stimulates the ovary to produce male hormones, which in turn, results in the PCOS problems. Metformin may play a significant role in the treatment of PCOS patients. Anatomy/Physiology/Mode of Action: Patients with insulin resistance are unable to fully utilize the insulin their body produces in combination with the glucose they consume. Without treatment, the elevated levels of insulin and glucose can result in hypertension, heart disease, abnormal uterine bleeding, abnormal hair growth, acne, uterine cancer and even infertility. Metformin works though a number of mechanisms: 1. It reduces glucose production from the liver which reduces both glucose and insulin levels (primary mode of action) 2. Decreases the intestinal absorption of glucose 3. Improves insulin sensitivity by increasing glucose cellular uptake and utilization 4. Decreases total cholesterol, triglycerides and LDL while leaving the “good” cholesterol levels essentially unchanged or even slightly improved 5. Decreases high blood pressure (hypertension) 6. Induces weight reduction Contraindications To Taking The Medications: Absolute Contraindications: Metformin is to be given carefully in patients with known kidney or heart disease. Metformin should not be given to patients with an allergy to the drug.