Mental Health in Remote and Rural Communities
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

'Mightier Than the Sword': the Life and Times of Sir John Waters Kirwan
‘Mightier than the Sword’: The Life and Times of Sir John Waters Kirwan (1866-1949) By Anne Partlon MA (Eng) and Grad. Dip. Ed This thesis is presented for the degree of Doctor of Philosophy of Murdoch University 2011 I declare that this thesis is my own account of my research and contains as its main content work which has not been previously submitted for a degree at any tertiary education institution. ............................................................... Anne Partlon ii Table of Contents Abstract iv Acknowledgements v Introduction: A Most Unsuitable Candidate 1 Chapter 1:The Kirwans of Woodfield 14 Chapter 2:‘Bound for South Australia’ 29 Chapter 3: ‘Westward Ho’ 56 Chapter 4: ‘How the West was Won’ 72 Chapter 5: The Honorable Member for Kalgoorlie 100 Chapter 6: The Great Train Robbery 120 Chapter 7: Changes 149 Chapter 8: War and Peace 178 Chapter 9: Epilogue: Last Post 214 Conclusion 231 Bibliography 238 iii Abstract John Waters Kirwan (1866-1949) played a pivotal role in the Australian Federal movement. At a time when the Premier of Western Australia Sir John Forrest had begun to doubt the wisdom of his resource rich but under-developed colony joining the emerging Commonwealth, Kirwan conspired with Perth Federalists, Walter James and George Leake, to force Forrest’s hand. Editor and part- owner of the influential Kalgoorlie Miner, the ‘pocket-handkerchief’ newspaper he had transformed into one of the most powerful journals in the colony, he waged a virulent press campaign against the besieged Premier, mocking and belittling him at every turn and encouraging his east coast colleagues to follow suit. -
Stories Poems Reviews Articles
ESTERLY stories poems reviews articles FOCUS ON WESTERN AUSTRALIA John La Nauze and Walter Murdoch Perth in the Thirties Paul Hasluck and Western Australia John Boyle O'Reilly F. C. B. Vosper and the Goldfields Era a quarterly review price two dollars registered at gpo perth for transmission by post as a periodical Category '8 ' UNIVERSITY OF WESTERN AUSTRALIA PRESS Giving the widest representation to Western Australian writers E. J. STORMON: The Salvado Memoirs $13.95 MARY ALBERTUS BAIN: Ancient Landmarks: A Social and Economic History of the Victoria District of Western Australia 1839-1894 $12.00 G. C. BOLTON: A Fine Country to Starve In $11.00 MERLE BIGNELL: The Fruit of the Country: A History of the Shire of Gnowangerup, Western Australia $12.50 R. A. FORSYTH: The Lost Pattern: Essays on the Emergent City Sensibility in Victorian England $13.60 L. BURROWS: Browning the Poet: An Introductory Study $8.25 T. GIBBONS: Rooms in the Darwin Hotel: Studies in English Literary Criticism and Ideas 1880-1920 $8.95 DOROTHY HEWETT, ED.: Sandgropers: A Western Australian Anthology $6.25 ALEC KING: The Un prosaic Imagination: Essays and Lectures on the Study of Literature $8.95 AVAILABLE ALL GOOD BOOKSELLERS Forthcoming Publications Will Include: MERAB T AUMAN: The Chief: Charles Yelverton O'Connor IAN ELLIOT: Moondyne Joe: The Man and the Myth J. E. THOMAS & Imprisonment in Western Australia: Evolution, Theory A. STEWART: and Practice The prices set out are recommended prices only. Eastern States Agents: Melbourne University Press, P.O. Box 278, Carlton South, Victoria, 3053. WESTERLY a quarterly review EDITORS: Bruce Bennett and Peter Cowan EDITORIAL ADVISORS: Patrick Hutchings, Leonard Jolley, Margot Luke, Fay Zwicky Westerly is published quarterly by the English Department, University of Western Australia, with assistance from the Literature Board of' the Australia Council and the Western Australian Literary Fund. -

Sir John Kirwan on Mental Health and Wellbeing
JULY 2020 VOLUME 32 | ISSUE 06 Breaking down barriers SIR JOHN KIRWAN ON MENTAL HEALTH AND WELLBEING ELDER FINANCIAL WORKPLACE DIVISION ABUSE WELLBEING 293 TAX IDENTIFYING THE FINANCIAL PART OF EARLY WARNING WELLBEING THE ADVICE SIGNS PROGRAM PROCESS JULY 2020 CONTENTS FOCUS INSIGHT GROW LIFE LEARN 06 NEWS 16 BREAKING 27 FINANCIAL 33 A VOICE FOR 35 UNDERSTANDING BARRIERS ABUSE RURAL WOMEN DIVISION 293 TAX FPA [Virtual] Conference. Former All Black Sir Financial planners Craig Phillips AFP® is Understanding when John Kirwan talks can play a critical role supporting Country and how a client needs about his own battle in protecting their to Canberra in to pay a Division 293 09 FASEA EXAM with depression and clients from elder empowering young tax liability is an his advocacy work financial abuse. women to reach important part of Registrations open for with mental wellbeing. their full leadership the advice process, says August 2020 exam potential. Brooke Logan. 24 LIVING THE 31 SPOT THE GOOD LIFE WARNING SIGNS Ryan Watson and Michelle Gibbings Tribeca Financial’s provides five tips to unique workplace help team leaders Financial Wellbeing create mentally Program. healthier workplaces. PUBLISHER Zeina Khodr M +61 414 375 371 The material should not be relied on without seeking independent professional advice and the Financial E zeina@ paperandspark.com.au MONEY & LIFE MAGAZINE is the official Planning Association of Australia Limited is not liable P.O. Box publication of the Financial Planning Association for any loss suffered in connection with the use of Paper + Spark ADVERTISING 443, Pyrmont NSW 2009 Suma Wiggins of Australia such material. -

The Life and Times of Sir John Waters Kirwan (1866-1949)
‘Mightier than the Sword’: The Life and Times of Sir John Waters Kirwan (1866-1949) By Anne Partlon MA (Eng) and Grad. Dip. Ed This thesis is presented for the degree of Doctor of Philosophy of Murdoch University 2011 I declare that this thesis is my own account of my research and contains as its main content work which has not been previously submitted for a degree at any tertiary education institution. ............................................................... Anne Partlon ii Table of Contents Abstract iv Acknowledgements v Introduction: A Most Unsuitable Candidate 1 Chapter 1:The Kirwans of Woodfield 14 Chapter 2:‘Bound for South Australia’ 29 Chapter 3: ‘Westward Ho’ 56 Chapter 4: ‘How the West was Won’ 72 Chapter 5: The Honorable Member for Kalgoorlie 100 Chapter 6: The Great Train Robbery 120 Chapter 7: Changes 149 Chapter 8: War and Peace 178 Chapter 9: Epilogue: Last Post 214 Conclusion 231 Bibliography 238 iii Abstract John Waters Kirwan (1866-1949) played a pivotal role in the Australian Federal movement. At a time when the Premier of Western Australia Sir John Forrest had begun to doubt the wisdom of his resource rich but under-developed colony joining the emerging Commonwealth, Kirwan conspired with Perth Federalists, Walter James and George Leake, to force Forrest’s hand. Editor and part- owner of the influential Kalgoorlie Miner, the ‘pocket-handkerchief’ newspaper he had transformed into one of the most powerful journals in the colony, he waged a virulent press campaign against the besieged Premier, mocking and belittling him at every turn and encouraging his east coast colleagues to follow suit. -
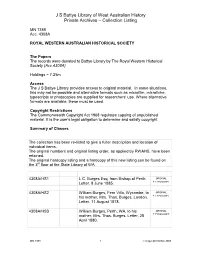
JS Battye Library of West Australian History Private Archives
J S Battye Library of West Australian History Private Archives – Collection Listing MN 1388 Acc. 4308A ROYAL WESTERN AUSTRALIAN HISTORICAL SOCIETY The Papers The records were donated to Battye Library by The Royal Western Historical Society (Acc.4308A) Holdings = 7.25m Access The J S Battye Library provides access to original material. In some situations, this may not be possible and alternative formats such as microfilm, microfiche, typescripts or photocopies are supplied for researchers’ use. Where alternative formats are available, these must be used. Copyright Restrictions The Commonwealth Copyright Act 1968 regulates copying of unpublished material. It is the user’s legal obligation to determine and satisfy copyright. Summary of Classes The collection has been re-listed to give a fuller description and location of individual items. The original numbers and original listing order, as applied by RWAHS, have been retained. The original hardcopy listing and a hardcopy of this new listing can be found on the 3rd floor at the State Library of WA 4308A/HS1 L.C. Burges Esq. from Bishop of Perth. ORIGINAL Letter, 8 June 1885. + TYPESCRIPT 4308A/HS2 William Burges, Fern Villa, Wycombe, to ORIGINAL his mother, Mrs. Thos. Burges, London. + TYPESCRIPT Letter, 11 August 1878. 4308A/HS3 William Burges, Perth, WA, to his ORIGINAL mother, Mrs. Thos. Burges. Letter, 28 + TYPESCRIPT April 1880. MN 1388 1 Copyright SLWA 2008 J S Battye Library of West Australian History Private Archives – Collection Listing 4308A/HS4 Tom (Burges) from Wm. Burges, ORIGINAL Liverpool, before sailing for Buenos + TYPESCRIPT Ayres. Letter, 9 June 1865. 4308A/HS5 Richard Burges, Esq. -
Campaign Federation
The Western Australian Historical Society The Federation Campaign 5 INCORPORATED After listening to the paper* prepared by the late Sir John Kirwan, I said that it was a valuable contribution and JOURNAL AND PROCEEDINGS should be plac~d on the permanent records of the Society. At the same time I expressed the opinion that there was VOL. IV. 1951 Part III. another side of the campaign and that Sir John Kirwan's paper did not do full justice to Forrest's endeavours in the The Society does not hold itself responsible tor statements made Interests of Western Australia. Since it is my purpose to or opinions expressed by authors oj the papers remedy this defect, I want it to be understood that I was associat~d pUblished in this Journal. with J ohn Kirwan on the "Kalgoorlie Miner" in the closmg months of 1895. Then was established a warm friendship that was never to the time of his death even te~porarily disturbed by differences of political opinion. The chief of these arose in connection wth the federation cam THE FEDERATION CAMPAIGN paign. A Paper prepared by Sir HAL COLEBATCH, C.M.G., and read My chief at the time of the campaign, Archibald ~ost to the W.A. Historical Society on March 30, 1951. Sanderson,. was one ?f the scholarly, courageous, and accurately mformed journalists Western Australia has had. Today, after fifty ~ears of federation, not one of the argu In a paper presented to the Historical Society the first ments he usee! against our then entry into federation can essential is that the facts set out should bear the authorita ive hall-mark of exact knowledge. -

RWAHS - Index of Early Days
RWAHS - Index of Early Days Vol 13 Part 5 2011 Mary Durack: the diarist Millett, Patsy 678 Vol 13 Part 5 2011 Lou Henry Hoover in Western Australia Layman, Lenore 653 Vol 13 Part 5 2011 The search for perfection: Western Australian postcards Pocock, Dereck 649 Vol 13 Part 5 2011 George Maxwell: bushman and naturalist Henderson, Bill 626 Vol 13 Part 5 2011 Louis Langoulant: a Frenchman in the colony O’Donnell, James & Thomas 607 Vol 13 Part 5 2011 A most singular man’: Robert Lyon Milne Reece, Bob 585 Vol 13 Part 5 2011 Arthur Shenton: gentle defender Shenton Turner, June 568 Vol 13 Part 5 2011 Swan River newspapers and their editors Steve Errington 543 Vol 13 Part 4 2010 Settling seasons: climate and agrarian enterprise Morgan, Ruth 514 Vol 13 Part 4 2010 The hidden community–Woodman Point quarantine station Seubert, Earle 496 Vol 13 Part 4 2010 J. B. Gribble: “Blackfellows’ friend" Green, Neville 478 Vol 13 Part 4 2010 Eating and drinking at early Swan River Colony Reece, Bob 462 Vol 13 Part 4 2010 Changing fashions in the Swan River Colony 1829-1929 Pearson, Jo 443 Vol 13 Part 4 2010 The Cornish - A rich seam in WA's Heritage Cornish, Patrick-joint 429 Vol 13 Part 4 2010 George Rutledge: success and tragedy Peter Enlund 411 Vol 13 Part 4 2010 To the golden west St Leon, Mark Valentine 389 Vol 13 Part 4 2010 Silbert: much more than a name Silbert, Hilary 323 Vol 13 Part 4 2010 The Cornish - a rich seam in WA’s heritage Wood, Jan -joint Vol 13 Part 3 2009 Reflections on the Swan River Graham-Taylor, Sue 371 Vol 13 Part 3 2009 British -

Western Australia People and Places
GETTING IT TOGETHER From Colonies to Federation western australia People and Places InVESTIGATIONS OF AUSTRALIa’s JOURNEYInvestigations of Australia’s journey tO NATIOnHOOD FOr tHe MIDDLE to nationhood for the middle years classroom YEARS CLASSRGETTOOMING IT TOGETHER western australIa – PeOPLE AND PLACES © COMMONWEALTH OF AUSTRALIa i Getting It Together: From Colonies to Federation has been funded by the Museum of Australian Democracy at Old Parliament House. Getting It Together: From Colonies to Federation – Western Australia ISBN: 978 1 74200 097 8 SCIS order number: 1427627 Full bibliographic details are available from Curriculum Corporation. PO Box 177 Carlton South Vic 3053 Australia Tel: (03) 9207 9600 Fax: (03) 9910 9800 Email: [email protected] Website: www.curriculum.edu.au Published by the Museum of Australian Democracy at Old Parliament House PO Box 7088 Canberra BC ACT 2610 Tel: (02) 6270 8222 Fax: (02) 6270 8111 www.moadoph.gov.au September 2009 © Commonwealth of Australia 2009 This work is copyright. You may download, display, print and reproduce this material in unaltered form only (retaining this notice) for your personal, non-commercial use or use within your organisation. Apart from any use as permitted under the Copyright Act 1968, all other rights are reserved. Requests and inquiries concerning reproduction and rights should be addressed to Commonwealth Copyright Administration, Attorney General’s Department, National Circuit, Barton ACT 2600 or posted at www.ag.gov.au/cca This work is available for download from the Museum of Australian Democracy at Old Parliament House: http://moadoph.gov.au/learning/resources-and-outreach Edited by Katharine Sturak and Zoe Naughten Designed by Deanna Vener GETTING IT TOGETHER western australIa – PeOPLE AND PLACES © COMMONWEALTH OF AUSTRALIa People and Places Each colony had particular concerns, challenges and opportunities to take into account when considering Federation. -
A Social History of Music in Coolgardie, Kalgoorlie and Boulder
A Social History of Music in Coolgardie, Kalgoorlie and Boulder 1892 to 1908 by Jean E Farrant BA MusB (Hons) Thesis submitted in fulfilment of the requirements for the degree of Master of Arts, Music Department, University of Western Australia February 1992 Resume The Eastern Goldfields of Western Australia developed very rapidly from the time that gold was first discovered at Coolgardie in 1892. Many of the townships which sprang up so quickly all over the region had a very short life, while others continued to thrive for some years. Kalgoorlie, which was soon to become the centre for the goldfields, is still a city today with a sizeable population, although its fortunes have waxed and waned over the years. This study traces the growth of musical activities in three of the towns of the area from their earliest beginnings to the peak of their prosperity. (In the case of Coolgardie, its rapid decline at the beginning of the century will also be noted.) The survey finishes in 1908, the year that imressive town hall buildings were opened in Boulder and Kalgoorlie respectively. Music was part of nearly every social acitivity of the day and there were attempts to establish the same types of musical organisations in each town. However, it will be demonstrated that certain musical groups flourished more successfully than others in the three townships selected for study, reflecting differences in background and interests of the local inhabitants. There was a strong community spirit in these townships clearly shown in the large sums of money raised for charity through music and the notion of a special goldfields ethos kept alive, in part, in organisations such as the Coolgardie Liedertafel, which held reunions long after its members had left the town. -
Hocking Family Struck a Rich Newspaper Lode at Kalgoorlie
PANPA Bulletin, April 2005, pp.56-57. Hocking family struck a rich newspaper lode at Kalgoorlie By Rod Kirkpatrick When you walk through the front door of the Kalgoorlie Miner, you enter a time warp. The jarrah-trimmed display windows and cabinet and the jarrah door are redolent of a bygone era, an era captured in the photographs on the walls showing the Miner building and its staff from the early days. The Miner is 110 years old in September this year. The three-storey building itself, although not the original office, was constructed in 1900 on the original site and the façade still proclaims: Hocking & Co. Limited: The Miner & Western Argus Offices. It is a landmark building in Kalgoorlie’s CBD. The rotary letterpress installed in 1901 gathers dust in the disused pressroom at the rear of the building. Kalgoorlie and other West Australian goldfields towns that emerged in the 1890s were “a Mecca of masculine labour” – and a Mecca for some newspaper proprietors and a misery for others. The first newspaper for Kalgoorlie came off a press established by the sons of a pioneer of the provincial press in Victoria and NSW. Decimus Horace Mott and Stanley Arthur Mott, two of the 10 sons of George Henry Mott, founder of the Border Post at Albury and an editor and owner or part-owner of various Victorian papers during the second half of the nineteenth century, launched the Western Argus at Kalgoorlie on November 24, 1894, only nine days after their press and type had arrived. For months the weekly paper lost money. -

The Western Australian Historical Society
The Story ot a Goldfields Newspaper so many there was a keen struggle for existence. A The Western Australian Historical Society high standard had to be maintained to live, especially INCORPORATED as the Goldfields community was cosmopolitan, amongst them being numerous well-educated, adven JOURNAL AND PROCEEDINGS turous and enterprising spirits attracted from all parts of the world by the lure of gold. None but the VOL. IV] 1949 [PART I most readable could survive. Of all those publications, only one is alive to-day-the Kalgoorlie Miner, which The Society does not hold itselj responsible tor statements made several years ago celebrated the fiftieth anniversary or opinions expressed by authors ot the papers of its first issue. published in this Journal The story of that paper, which I edited for the first thirty years of its existence, is one of the romances of the Australian Press. The story begins seventeen months after Paddy Hannan picked up the piece of THE STORY OF A GOLDFIELDS gold that made his name famous. The scene of the NEWSPAPER find was still called Hannans. It had become a collec tion of hessian humpies and tents with little or no A ROMANCE OF THE PRESS resemblance of a town. There was a miserable erec tion that served as a Post Office; trees stood in what KALGOORLIE EARLY DAYS is to-day Hannan Street. There were a few bag A Paper prepared by the Hon. SIR JOHN KIRWAN, K.C.M.G., shanties, at one of which -iquor was sold, and at others and read to the W.A. -

Local Hero Brought Spirit of a New Age to the State
Kalgoorlie Miner Monday 14/1/2019 Brief: PARLWA-WA1 Page: 8 Page 1 of 7 Section: General News Region: Kalgoorlie WA Circulation: 3,224 Type: Regional Size: 1,928.00 sq.cms. Frequency: MTWTFS- Local hero brought spirit of a new age to the State Sir John Kirwan, former Kalgoorlie Miner editor, campaigned passionately and successfully for many progressive causes ᔡ Jan Mayman Irishman John Kirwan (1869- with friends and family in the East- Adventure. 1949) was a crusading editor of ern colonies. “Notwithstanding hardships the Kalgoorlie Miner in the late By 1899, opposition to the Forrest and dangers, the country around 19th century when WA’s East- government inspired moves for ern Goldfields held a third of separation of the Eastern Gold- Coolgardie was explored for hun- the vast State’s population. A fields from the rest of Australia to dreds of miles and it was found that passionate democrat, Kirwan create a new state in the desert it was not a mere ‘goldfield’ that inspired his readers to force called “Auralia”. was discovered, but what could be reluctant Premier John Forrest Kirwan’s fiery writing led to a characterised as a golden conti- to bring Australia’s western petition to Queen Victoria to sepa- nent. third into the national Federa- rate the Eastern Goldfields from “By May 1893, there were over tion in 1900. He learned his WA if it did not join the new Feder- 1000 men on the field. Valuable trade in Dublin, then emigrated ation. finds were reported in various out- to Brisbane, working in Sydney, The miners sent their appeal to side localities.