Chronic Lymphocytic Leukemia in Neurofibromatosis Type 1 Patients: Case Report and Literature Review of a Rare Occurrence
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Brca2 Is Required for Embryonic Cellular Proliferation in the Mouse
Downloaded from genesdev.cshlp.org on October 4, 2021 - Published by Cold Spring Harbor Laboratory Press Brca2 is required for embryonic cellular proliferation in the mouse Akira Suzuki, 1'2'6 Jos6 Luis de la Pompa, 1'2'6 RazqaUah Hakem, 1'2 Andrew Elia, 1'2 Ritsuko Yoshida, 1'2 Rong Mo, 3'4 Hiroshi Nishina, 1'2 Tony Chuang, 1'2 Andrew Wakeham, ~'2 Annick Itie, ~'2 Wilson Koo, ~'2 Phyllis Billia, ~'2 Alexandra Ho, 1'2 Manabu Fukumoto, 5 Chi Chung Hui, 3'4 and Tak W. Mak 1'2"7 1Amgen Institute, Toronto, Ontario, Canada M5G 2C1; 2Ontario Cancer Institute, Department of Medical Biophysics and Immunology, 3Department of Molecular and Medical Genetics, University of Toronto, Toronto, Ontario, Canada; 4program in Developmental Biology and Division of Endocrinology Research Institute, The Hospital for Sick Children, Toronto, Ontario, Canada M5G 1X8; SDepartment of Pathology, Graduate School of Medicine, Kyoto University, Kyoto, Japan 606 Mutations of the tumor suppressor gene BRCA2 are associated with predisposition to breast and other cancers. Homozygous mutant mice in which exons 10 and 11 of the Brca2 gene were deleted by gene targeting (Brca2 I°-11) die before day 9.5 of embryogenesis. Mutant phenotypes range from severely developmentally retarded embryos that do not gastrulate to embryos with reduced size that make mesoderm and survive until 8.5 days of development. Although apoptosis is normal, cellular proliferation is impaired in Brca2 ~°-H mutants, both in vivo and in vitro. In addition, the expression of the cyclin-dependent kinase inhibitor p21 is increased. Thus, Brca2 l°-H mutants are similar in phenotype to Brcal 5-6 mutants but less severely affected. -
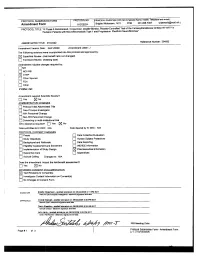
Network Scan Data
CTEP Protocol No: T-99-0090 CC Protocol No: 01-C-0222 Amendment: J Revised: 4/21/09 IRB Approval Date: A Phase II Randomized, Cross-Over, Double-Blinded, Placebo-Controlled Trial of the Farnesyltransferase Inhibitor R115777 in Pediatric Patients with Neurofibromatosis Type 1 and Progressive Plexiform Neurofibromas Coordinating Center: Pediatric Oncology Branch, NCI Principal Investigator: Brigitte Widemann, M.D.* (POB, NCI) NIH Associate Investigators: Frank M. Balis, M.D. (POB, NCI) Beth Fox, M.D. (POB, NCI) Kathy Warren, M.D. (NOB, NCI) Andy Gillespie, R.N. (ND, CC) Eva Dombi, MD (POB, NCI)** Nalini Jayaprakash, (POB, NCI) Diane Cole, (POB, NCI) Seth Steinberg, Ph.D. (BDMB, DCS, NCI) Nicholas Patronas, M.D. (DR, CC)** Maria Tsokos, M.D., (Laboratory of Pathology, NCI)** Pamela Wolters, Ph.D. (HAMB, NCI) Staci Martin, Ph.D. (HAMB, NCI) Jeffrey Solomon, (NIH and Sensor Systems, Inc.) Non-NIH Associate Investigators: Wanda Salzer, M.D. ** Keesler Air Force Base, Biloxi, Mississippi) 81st MDOS/SGOC 301 Fisher Street, Room 1A132 Keesler AFB, MS 39534-2519 Phone: 228-377-6524 E-mail: [email protected] Bruce R. Korf, M.D., Ph.D. ** Chair, Department of Genetics Univeristy of Alabama at Birmingham 1530 3rd Ave. S. Birmingham, AL 35294 Phone: (205)-934-9411, Fax: (205)-934-9488 E-mail: [email protected] David H. Gutmann, M.D., Ph.D. ** Department of Neurology Washington University School of Medicine St. Louis Children’s Hospital Box 8111, 660 S. Euclid Avenue St. Louis, MO 63110 Phone: (314)-632-7149, Fax: (314)-362-9462 E-mail: [email protected] 1 4/21/2009 T-99-0090, 01-C-0222 Arie Perry, M.D. -

BRCA1 and BRCA2 Full Gene Sequence Analysis and Common Deletion/Duplication Variants
BRCA1 and BRCA2 Full Gene Sequence Analysis and Common Deletion/Duplication Variants Testing includes full gene sequencing of exons and 25 base pairs of introns of BRCA 1 and 2 and the common deletions of BRCA1 (exon 13 del 3.835kb, exon 13 dup 6kb, exon 14-20 del 26kb, exon 22 del 510bp, exon 8-9 del 7.1kb). Sequencing does not include the promoter, enhancers or splicing modulators in intronic regions. Deletion duplication analysis is limited to the commonly reported variants; refer to full deletion/duplication testing. Indication: This testing is indicated for individuals that meet the criteria for Hereditary Breast and Ovarian Cancer listed in the National Comprehensive Cancer Network (NCCN) guidelines. For assistance with interpreting guidelines, please contact Henry Ford Precision Genomic Diagnostics, or refer to genetic counseling for evaluation. Testing on minors is not indicated. BRCA1 and BRCA2 are genes that code for proteins that help repair DNA damage. Inherited mutations in BRCA 1 or 2, in combination with additional acquired mutations, can result in increased risk for developing cancer. Specific mutations in BRCA1 and BRCA2 increase the risk of breast and ovarian cancers, and have been associated with increased risk of several additional types of cancer. BRCA1 and BRCA2 mutations account for about 20 to 25 percent of hereditary breast cancers and about 5 to 10 percent of all breast cancers. In addition, BRCA1 and BRCA2 account for about 15 percent of ovarian cancers overall. Breast and ovarian cancers associated with BRCA1 and BRCA2 mutations tend to develop at younger ages than their nonhereditary counterparts. -

Infrequency of BRCA2 Alterations in Head and Neck Squamous Cell Carcinoma
Oncogene (1997) 14, 2189 ± 2193 1997 Stockton Press All rights reserved 0950 ± 9232/97 $12.00 Infrequency of BRCA2 alterations in head and neck squamous cell carcinoma Haskell Kirkpatrick1, Pamela Waber1, To Hoa-Thai1, Robert Barnes1, Sherri Osborne-Lawrence1, John Truelson2, Perry Nisen1 and Anne Bowcock1 1Division of Hematology/Oncology, Department of Pediatrics, University of Texas Southwestern Medical Center, 5323 Harry Hines Boulevard, Dallas, Texas 75235-8591; 2Department of Otolaryngology, University of Texas Southwestern Medical Center, 5323 Harry Hines Boulevard, Dallas, Texas 75235-8591, USA Alterations of BRCA2 result in increased susceptibility chromosome regions 1p, 3p, 7q, 9p, 11q and 17p to breast cancer in both men and women (relative (Cowan et al., 1992; Jin et al., 1993; Maestro et al., lifetime risks of 0.06 and 0.8 respectively). BRCA2 maps 1993; Rowley et al., 1996; Wu et al., 1994; van der Riet to 13q12-q13 and encodes a transcript of 10 157 bp. et al., 1994; Reed et al., 1996; Nawroz et al., 1994). Other cancers that have been described in BRCA2 Loss of heterozygosity (LOH) studies that frequently mutation carriers include those of the larynx. Human reveal the locale of tumor suppressor genes (Ponder, chromosome 13q has been shown previously by LOH 1988) have been performed by us and others and studies to harbor several tumor suppressor genes for head revealed regions on chromosomes 3, 8, 9, 13, 17p12 and neck squamous cell carcinoma (HNSCCs). We and multiple others (Nawroz et al., 1994; Ah-See et al., therefore examined the role of BRCA2 in the develop- 1994; Li et al., 1994). -

(NF1) Defects Are Common in Human Ovarian Serous Carcinomas and Co-Occur with TP53 Mutations
Volume 10 Number 12 December 2008 pp. 1362–1372 1362 www.neoplasia.com Neurofibromin 1 (NF1) Defects Navneet Sangha*, Rong Wu*, Rork Kuick†, Scott Powers‡, David Mu§, Diane Fiander*, Are Common in Human Ovarian Kit Yuen*, Hidetaka Katabuchi¶, Hironori Tashiro¶, Serous Carcinomas and Co-occur Eric R. Fearon*,†,# and Kathleen R. Cho*,†,# 1,2 with TP53 Mutations *Department of Pathology, The University of Michigan Medical School, Ann Arbor, MI 48109, USA; †The Comprehensive Cancer Center, The University of Michigan Medical School, Ann Arbor, MI 48109, USA; ‡Cold Spring Harbor Laboratory, Cold Spring Harbor, NY 11724, USA; §Department of Pathology, Penn State University College of Medicine, Hershey, PA 17033, USA; ¶Department of Gynecology, Kumamoto University, Kumamoto, 860-8556, Japan; #Department of Internal Medicine, The University of Michigan Medical School, Ann Arbor, MI 48109, USA Abstract Ovarian serous carcinoma (OSC) is the most common and lethal histologic type of ovarian epithelial malignancy. Mutations of TP53 and dysfunction of the Brca1 and/or Brca2 tumor-suppressor proteins have been implicated in the molecular pathogenesis of a large fraction of OSCs, but frequent somatic mutations in other well-established tumor-suppressor genes have not been identified. Using a genome-wide screen of DNA copy number alterations in 36 primary OSCs, we identified two tumors with apparent homozygous deletions of the NF1 gene. Subsequently, 18 ovarian carcinoma–derived cell lines and 41 primary OSCs were evaluated for NF1 alterations. Markedly re- duced or absent expression of Nf1 protein was observed in 6 of the 18 cell lines, and using the protein truncation test and sequencing of cDNA and genomic DNA, NF1 mutations resulting in deletion of exons and/or aberrant splicing of NF1 transcripts were detected in 5 of the 6 cell lines with loss of NF1 expression. -

Depo-Provera
PRODUCT MONOGRAPH INCLUDING PATIENT MEDICATION INFORMATION PR ® DEPO-PROVERA medroxyprogesterone acetate injectable suspension, USP Sterile Aqueous Suspension 50 mg/mL and 150 mg/mL Progestogen Pfizer Canada Inc. Date of Revision: 17,300 Trans-Canada Highway February 13, 2018 Kirkland, Quebec H9J 2M5 Submission Control No: 210121 ® Pharmacia & Upjohn Company LLC Pfizer Canada Inc., Licensee © Pfizer Canada Inc., 2018 Table of Contents PART I: HEALTH PROFESSIONAL INFORMATION......................................................... 3 SUMMARY PRODUCT INFORMATION ........................................................................ 3 INDICATIONS AND CLINICAL USE .............................................................................. 3 CONTRAINDICATIONS ................................................................................................... 4 WARNINGS AND PRECAUTIONS: ................................................................................ 5 ADVERSE REACTIONS ................................................................................................. 18 DRUG INTERACTIONS .................................................................................................. 27 DOSAGE AND ADMINISTRATION .............................................................................. 28 OVERDOSAGE ................................................................................................................ 30 ACTION AND CLINICAL PHARMACOLOGY ............................................................ 30 STORAGE AND -

Inherited Cancer Predisposition Syndromes in Greece
ANTICANCER RESEARCH 28: 1341-1348 (2008) Review Inherited Cancer Predisposition Syndromes in Greece ANGELA APESSOS1, EIRINI PAPADOPOULOU1, IOULIA BELOGIANNI1, SOTIRIS BARATSIS2, JOHN K. TRIANTAFILLIDIS3, PARIS KOSMIDIS3, EIRINI KARYDAS4, EVANGELOS BRIASOULIS5, CHRISTOS PISIOTIS6, KOSTAS PAPAZISIS7 and GEORGE NASIOULAS1,3 1Department of Molecular Biology, 4Breast Cancer Center, 6DTCA HYGEIA SA, Kifissias Av. & 4 Er. Stavrou str, 151 23 Maroussi, Athens; 2First Surgical Department, ‘Evangelismos' General Hospital of Athens, 45-47 Ipsilantou Street, Kolonaki, Athens; 3Hellenic Cooperative Oncology Group; 5Department of Medical Oncology, University Hospital of Ioannina, Medical School, University of Ioannina, Ioannina; 7“Theagenion” Cancer Hospital, Al. Simeonides str. 2, 54007 Thessaloniki, Greece Abstract. Hereditary cancer syndromes comprise Hereditary cancer syndromes comprise approximately 5-10% approximately 5-10% of diagnosed carcinomas. They are of diagnosed carcinomas. They are caused by mutations in caused by mutations in specific genes. Carriers of mutations in specific genes. Carriers of such mutations are at an increased these genes are at an increased risk of developing cancer at a risk of developing cancer at an early age. Today, there are a young age. When there is a suspicion of a hereditary cancer number of options available for the prevention and treatment predisposition syndrome a detailed family tree of the patient of inherited cancer predisposition syndrome for patients and requesting screening is constructed. DNA is isolated from all their families. Furthermore, advances in molecular biology available members of the family. Mutation detection is carried and in vitro fertilization techniques have made possible out on DNA from an affected family member. If a mutation is preimplantation genetic diagnosis (PGD) for the prevention found the remaining family is screened. -

Lessons Learned from BRCA1 and BRCA2
Oncogene (2000) 19, 6159 ± 6175 ã 2000 Macmillan Publishers Ltd All rights reserved 0950 ± 9232/00 $15.00 www.nature.com/onc Lessons learned from BRCA1 and BRCA2 Lei Zheng1, Shang Li1, Thomas G Boyer1 and Wen-Hwa Lee*,1 1Department of Molecular Medicine, Institute of Biotechnology, University of Texas Health Science Center at San Antonio, 15355 Lambda Drive, San Antonio, Texas, TX 78245, USA BRCA1 and BRCA2 are breast cancer susceptibility susceptibility genes has provided two human genetic genes. Mutations within BRCA1 and BRCA1 are models for studies of breast cancer. responsible for most familial breast cancer cases. To understand how the loss of BRCA1 or BRCA2 Targeted deletion of Brca1 or Brca2 in mice has function leads to breast cancer formation, mouse revealed an essential function for their encoded products, genetic models for BRCA1 or BRCA2 mutations have BRCA1 and BRCA2, in cell proliferation during been established. This work has revealed that Brca1 embryogenesis. Mouse models established from condi- homozygous deletions are lethal at early embryonic tional expression of mutant Brca1 alleles develop days (E)5.5 ± 13.5 (Gowen et al., 1996; Hakem et al., mammary gland tumors, providing compelling evidence 1996; Liu et al., 1996; Ludwig et al., 1997). Three that BRCA1 functions as a breast cancer suppressor. independent groups generated distinct mutations within Human cancer cells and mouse cells de®cient in BRCA1 Brca1, yet nonetheless observed similar embryonic or BRCA2 exhibit radiation hypersensitivity and phenotypes, including defects in both gastrulation and chromosomal abnormalities, thus revealing a potential cellular proliferation, and death at E6.5 (Hakem et al., role for both BRCA1 and BRCA2 in the maintenance of 1996; Liu et al., 1996; Ludwig et al., 1997). -

Identification of Novel BRCA2-Binding Proteins That Are Essential for Meiotic Homologous Recombination
Identification of novel BRCA2-binding proteins that are essential for meiotic homologous recombination Jingjing Zhang Department of Chemistry and Molecular Biology University of Gothenburg 2021 Identification of novel BRCA2-binding proteins that are essential for meiotic homologous recombination © Author 2021 [email protected] ISBN 978-91-8009-166-4 (PRINT) ISBN 978-91-8009-167-1 (PDF) http://hdl.handle.net/2077/67213 Printed in Gothenburg, Sweden 2021 Printed by STEMA SPECIALTRYCK AB For CD village Identification of novel BRCA2-binding proteins that are essential for meiotic homologous recombination Jingjing Zhang Department of Chemistry and Molecular Biology, University of Gothenburg, SE-40530 Gothenburg, Sweden Abstract Meiotic recombination is a molecular process in which the induction and repair of programmed DNA double-strand breaks (DSBs) creates genetic exchange between homologous chromosomes and thus increases genetic diversity and ensures chromosome segregation. Breast cancer susceptibility gene 2 (BRCA2) is a potent cancer suppressor and is required for DSB repair by homologous recombination (HR) in mitosis. However, due to the embryonic lethality of the Brca2 knockout (KO) mice, the role of BRCA2 in meiotic HR is less well defined. In our work, we have identified two novel meiosis-specific proteins, MEILB2 (meiotic localizer of BRCA2) and BRME1 (BRCA2 and MEILB2-associating protein 1) that form a ternary complex with BRCA2 and shed light on BRCA2 and its co-factors' roles during meiotic HR. In Meilb2 KO male mice, the localization of the recombinases RAD51 and DMC1, which catalyze the homology-directed repair of DSBs, is almost totally abolished, leading to errors in meiotic DSB repair and subsequent sterility. -

Cutaneous Neurofibromas: Clinical Definitions Current Treatment Is Limited to Surgical Removal Or Physical Or Descriptors Destruction
ARTICLE OPEN ACCESS Cutaneous neurofibromas Current clinical and pathologic issues Nicolas Ortonne, MD, PhD,* Pierre Wolkenstein, MD, PhD,* Jaishri O. Blakeley, MD, Bruce Korf, MD, PhD, Correspondence Scott R. Plotkin, MD, PhD, Vincent M. Riccardi, MD, MBA, Douglas C. Miller, MD, PhD, Susan Huson, MD, Dr. Wolkenstein Juha Peltonen, MD, PhD, Andrew Rosenberg, MD, Steven L. Carroll, MD, PhD, Sharad K. Verma, PhD, [email protected] Victor Mautner, MD, Meena Upadhyaya, PhD, and Anat Stemmer-Rachamimov, MD Neurology® 2018;91 (Suppl 1):S5-S13. doi:10.1212/WNL.0000000000005792 Abstract RELATED ARTICLES Objective Creating a comprehensive To present the current terminology and natural history of neurofibromatosis 1 (NF1) cuta- research strategy for neous neurofibromas (cNF). cutaneous neurofibromas Page S1 Methods NF1 experts from various research and clinical backgrounds reviewed the terms currently in use The biology of cutaneous fi for cNF as well as the clinical, histologic, and radiographic features of these tumors using neuro bromas: Consensus published and unpublished data. recommendations for setting research priorities Results Page S14 Neurofibromas develop within nerves, soft tissue, and skin. The primary distinction between fi fi Considerations for cNF and other neuro bromas is that cNF are limited to the skin whereas other neuro bromas development of therapies may involve the skin, but are not limited to the skin. There are important cellular, molecular, for cutaneous histologic, and clinical features of cNF. Each of these factors is discussed in consideration of neurofibroma a clinicopathologic framework for cNF. Page S21 Conclusion Clinical trial design for The development of effective therapies for cNF requires formulation of diagnostic criteria that cutaneous neurofibromas encompass the clinical and histologic features of these tumors. -

BRCA in Gastrointestinal Cancers: Current Treatments and Future Perspectives
cancers Review BRCA in Gastrointestinal Cancers: Current Treatments and Future Perspectives Eleonora Molinaro, Kalliopi Andrikou, Andrea Casadei-Gardini * and Giulia Rovesti Department of Oncology and Hematology, Division of Oncology, University of Modena and Reggio Emilia, 41121 Modena, Italy; [email protected] (E.M.); [email protected] (K.A.); [email protected] (G.R.) * Correspondence: [email protected] Received: 10 October 2020; Accepted: 11 November 2020; Published: 12 November 2020 Simple Summary: BRCA gene mutations are progressively gaining more attention in the context of gastrointestinal malignancies, especially in pancreatic cancer where their identification can have both therapeutic and surveillance relevance. Abstract: A strong association between pancreatic cancer and BRCA1 and BRCA2 mutations is documented. Based on promising results of breast and ovarian cancers, several clinical trials with poly (ADP-ribose) polymerase inhibitors (PARPi) are ongoing for gastrointestinal (GI) malignancies, especially for pancreatic cancer. Indeed, the POLO trial results provide promising and awaited changes for the pancreatic cancer therapeutic landscape. Contrariwise, for other gastrointestinal tumors, the rationale is currently only alleged. The role of BRCA mutation in gastrointestinal cancers is the subject of this review. In particular, we aim to provide the latest updates about novel therapeutic strategies that, exploiting DNA repair defects, promise to shape the future therapeutic scenario of GI cancers. Keywords: BRCA1; BRCA2; gastrointestinal cancers; HRD; pancreatic cancer; Olaparib; PARP inhibitors; surveillance 1. Introduction BRCA1 and BRCA2 are famous tumor susceptibility genes. They encode for proteins playing a crucial role in the correct repair of damaged DNA. Indeed, these genes are key components of the homologous recombination (HR) pathway [1]. -

Genetic Testing for BRCA1 and BRCA2: Information for Texas Health Care Professionals
Genetic Testing for BRCA1 and BRCA2: Information for Texas Health Care Professionals How common are BRCA1 and BRCA2 mutations in the general population? Inherited mutations in BRCA1 and BRCA2 are relatively uncommon in the general population. The carrier frequency is estimated to range from 1 in 300 to 1 in 800.1,3 Certain ethnic groups have been shown to have a higher carrier frequency (i.e., 1 in 40 for individuals of Ashkenazi Jewish descent). What percentage of breast and ovarian cancer cases are estimated to be caused by BRCA1 and BRCA2 mutations? Five to 10 percent of all breast cancer cases and up to 14 percent of all ovarian cancer cases are thought to be caused by BRCA1 and BRCA2 mutations.1,2,3,4 Can BRCA1 and BRCA2 mutations be inherited from either side of the family? Yes, either parent can pass along a BRCA1 or BRCA2 mutation. Therefore, it is important for clinicians to obtain a complete cancer history on both the maternal and the paternal sides of the family when assessing genetic risk.4 Which patients should I consider referring to a genetic counselor for risk assessment and to discuss the option of genetic testing for BRCA1 and BRCA2 mutations? Most individuals do not have a mutation in the BRCA1 or BRCA2 gene. While specific indications for genetic counseling and testing vary among professional organizations, certain aspects of your patient’s personal and/or family history may increase his or her likelihood of carrying a BRCA1 or BRCA2 mutation. The indications below are to be used as a guide and are not a substitute for clinical judgment.