ﺑﺴﻢ اﷲ اﻟﺮﺣﻤﻦ اﻟﺮﺣﻴﻢ Cephradine Bioequivalence and Its Interaction with Khat and Food (Al-Sayadeyah) in Yemen
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Susceptibility of Escherichia Coli to 3-Lactam Antibiotics
ANTIMICROBIAL AGENTS AND CHEMOTHERAPY, Mar. 1994, p. 494-498 Vol. 38, No. 3 0066-4804/94/$04.00+0 Copyright © 1994, American Society for Microbiology Effect of Hyperproduction of TEM-1 1-Lactamase on In Vitro Susceptibility of Escherichia coli to 3-Lactam Antibiotics PEI-JUN WU,t KEVIN SHANNON,*t AND IAN PHILLIPS Department of Microbiology, United Medical and Dental Schools, St. Thomas' Hospital, London SE1 7EH, United Kingdom Received 21 July 1993/Returned for modification 4 November 1993/Accepted 4 January 1994 The susceptibility of 173 TEM-1-producing isolates of Escherichia coli was assessed by determination of MICs by the agar dilution method. MICs of amoxicillin, mezlocillin, cephaloridine, and, to a smaller extent, amoxicillin-clavulanic acid (but not cephalexin, cefuroxime, cefotaxime, ceftazidime, or imipenem) were higher for isolates that produced large amounts of f8-lactamase than for isolates that produced smaller amounts. The effect of fixed concentrations of clavulanic acid on resistance to amoxicillin was assessed for 34 selected TEM-1-producing isolates. Low concentrations of the inhibitor (0.5 to 1 ,ug/ml) reduced the amoxicillin MICs substantially for almost all the isolates, although the reductions were not sufficient to render any of the isolates amoxicillin susceptible. Higher concentrations of clavulanic acid had progressively greater effects on amoxicillin MICs, but even at 8 ,ug/ml some of the isolates with high P-lactamase activities remained resistant or only moderately susceptible to amoxicillin. All the isolates were inhibited by clavulanic acid (in the absence of amoxicillin) at concentrations of 16 to 32 ,ug/ml. TEM-1 ,-lactamase activity was inhibited in vitro by clavulanic acid, but not totally, with approximately 2% of the initial activity remaining at 2 ,ug/ml and 0.4% remaining at 8 ,guml. -

WO 2010/025328 Al
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date 4 March 2010 (04.03.2010) WO 2010/025328 Al (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every A61K 31/00 (2006.01) kind of national protection available): AE, AG, AL, AM, AO, AT, AU, AZ, BA, BB, BG, BH, BR, BW, BY, BZ, (21) International Application Number: CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, DO, PCT/US2009/055306 DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (22) International Filing Date: HN, HR, HU, ID, IL, IN, IS, JP, KE, KG, KM, KN, KP, 28 August 2009 (28.08.2009) KR, KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, (25) Filing Language: English NO, NZ, OM, PE, PG, PH, PL, PT, RO, RS, RU, SC, SD, (26) Publication Language: English SE, SG, SK, SL, SM, ST, SV, SY, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. (30) Priority Data: 61/092,497 28 August 2008 (28.08.2008) US (84) Designated States (unless otherwise indicated, for every kind of regional protection available): ARIPO (BW, GH, (71) Applicant (for all designated States except US): FOR¬ GM, KE, LS, MW, MZ, NA, SD, SL, SZ, TZ, UG, ZM, EST LABORATORIES HOLDINGS LIMITED [IE/ ZW), Eurasian (AM, AZ, BY, KG, KZ, MD, RU, TJ, —]; 18 Parliament Street, Milner House, Hamilton, TM), European (AT, BE, BG, CH, CY, CZ, DE, DK, EE, Bermuda HM12 (BM). -

Distinct Penicillin Binding Proteins Involved in the Division
Proc. Nat. Acad. Sci. USA Vol. 72, No. 8, pp. 2999- , August 1975 Biochemistry Distinct penicillin binding proteins involved in the division, elongation, and shape of Escherichia coli K12 (P-lactam antibiotics/slab gel electrophoresis/binding protein mutants) BRIAN G. SPRATT Department of Biochemical Sciences, Moffett Laboratories, Princeton University, Princeton, New Jersey 08540 Communicated by Arthur B. Pardee, May 20,1975 ABSTRACT The varied effects of #-lactam antibiotics on ied effects of f3-lactam antibiotics by their relative affinities cell division, cell elongation, and cell shape in E. coil are for three proteins involved in cell division, elongation, and shown to be due to the presence of three essential penicillin binding proteins with distinct roles in these three processes. the maintenance of cell shape. (A) Cell shape: ,-Lactams that specifically result in the pro- duction of ovoid cells bind to penicillin binding protein 2 METHODS (molecular weight 66,000). A mutant has been isolated that The organism used in these studies was E. coil K12 (strain fails to bind ft-lactams to protein 2, and that grows as round cells. (B) Cell division: f-Lactams that specifically inhibit cell KN126). It was grown in Difco Pennassay broth at 370 with division bind preferentially to penicillin binding protein 3 vigorous aeration and harvested at late logarithmic phase. (molecular weight 60,000). A temperature-sensitive cell divi- Mutants B6 and 6-30 were grown in the same medium at sion mutant has been shown to have a thermolabile protein 300. 3. (C) Cell elongation: One ft-lactam that preferentially inhib- Assay of Penicillin Binding Proteins. -

Appraisal of Multifarious Brands of Cephradine for Their in Vitro Antibacterial Activity Against Varied Microorganisms
Appraisal of multifarious brands of Cephradine for their in vitro antibacterial activity against varied microorganisms Sajid Bashir1, Shamshad Akhtar1, Shahzad Hussain*2, Farnaz Malik2, Sidra Mahmood3, Alia Erum1 and Ume-Ruqiatulain1 1Department of Pharmacy, Sargodha University, Sargodha, Pakistan 2National Institute of Health, Islamabad, Pakistan 3Department of Bioinformatics and Biotechnology, International Islamic University, Islamabad, Pakistan Abstract: The astounding and exceptional growth of generic pharmaceutical Industry in Pakistan has raised certain questions for drug regulatory authorities contemplating their efficacy and quality. The current study focuses on assessing the in-vitro antimicrobial activity of 24 brands of Cephradine 500mg capsules against 4 different strains by employing standardized methods. Disk diffusion method was performed on all brands to look into the susceptibility and resistance patterns. Standard disk of 5µg Cephradine powder were used during evaluation. The zones of inhibitions were ranged from 24-40mm against S. aureus, 24-40mm against E. coli, 20-25mm against K. pneumonia and 19-23mm P. mirabilis. On the basis of mean value, the multinational brands were found to have better zone of inhibitions and were better than local Pharmaceutical companies but ANOVA cooperative study showed that all brands of Cephradine showed similar comparable results. Further investigations by employing MIC method, quality of raw material with special emphasis on the shelf-life, excepients and method of manufacturing will be needed to obtain more authenticated results. The price of National and Multinational brands ranges from Rs.156.00-212.00 for 10 capsules. It is concluded that Public health is at risk because of noticeable growing widespread curse of the manufacture and trade of sub-standard or below par pharmaceuticals. -

A Thesis Entitled an Oral Dosage Form of Ceftriaxone Sodium Using Enteric
A Thesis entitled An oral dosage form of ceftriaxone sodium using enteric coated sustained release calcium alginate beads by Darshan Lalwani Submitted to the Graduate Faculty as partial fulfillment of the requirements for the Master of Science Degree in Pharmaceutical Sciences with Industrial Pharmacy Option _________________________________________ Jerry Nesamony, Ph.D., Committee Chair _________________________________________ Sai Hanuman Sagar Boddu, Ph.D, Committee Member _________________________________________ Youssef Sari, Ph.D., Committee Member _________________________________________ Patricia R. Komuniecki, PhD, Dean College of Graduate Studies The University of Toledo May 2015 Copyright 2015, Darshan Narendra Lalwani This document is copyrighted material. Under copyright law, no parts of this document may be reproduced without the expressed permission of the author. An Abstract of An oral dosage form of ceftriaxone sodium using enteric coated sustained release calcium alginate beads by Darshan Lalwani Submitted to the Graduate Faculty as partial fulfillment of the requirements for the Master of Science Degree in Pharmaceutical Sciences with Industrial Pharmacy option The University of Toledo May 2015 Purpose: Ceftriaxone (CTZ) is a broad spectrum semisynthetic, third generation cephalosporin antibiotic. It is an acid labile drug belonging to class III of biopharmaceutical classification system (BCS). It can be solvated quickly but suffers from the drawback of poor oral bioavailability owing to its limited permeability through -

Cefotaxime: Rate of Bacterial Killing and Interactions with Serum and Leukocyte Activity
ACTA M~DICA PORTUGUESA 1983; 4: 167-171 ORIGINAL CEFOTAXIME: RATE OF BACTERIAL KILLING AND INTERACTIONS WITH SERUM AND LEUKOCYTE ACTIVITY GIULIANA GIALDRONI GRASSI, PATRIZIA MANGIAROTTI, ANNA FIETTA Chair of Chemotherapy. Istituto Forlanini. University of Pavia. Italy SUMMARY Cefotaxime (HR 756) was compared with cefazolin and cephaloridine with regard to the rate of bacterial killing and to the influence on the bactericidal activity of human serum and polyrnorphonuclear leukocytes. At concentrations equal to 1-2 x MIC cefotaxime showed a more rapid and complete bactericidal activity on E. coil K 12 than cephaloridine and cefazolin. In presence of the latters in fact, bacterial regrowth was observed after 24 hours. On S. aureus a complete killing activity of cefotaxime appeared at concentrations of 8 x MIC. A synergism seemed to exist between the complement dependent bactericidal activity of normal human serum and cephalosporins. E. coil K 12 (a rough strain) was killed by the combi nation of human serum and both cefotaxime and cefazolin at concentrations that were not bactericidal by themselves. Cephaloridine on the contrary showed an additive activity with normal human serum. Finally evidence that cefotaxime enhanced the bactericidal activity of human polymorphonuclear leukocytes against S. faecaiis, is reported. RESUMO Cefotaxirna: Poder Bactericida e Interaccao corn a Actividade Leucocitãria e do Soro. Cornparou-se o poder bactericida e a interferência da cefotaxima (HR 756) na actividade bactericida dos leucocitos polimorfonucleares e do soro corn os parametros equivalentes referentes a cefazolina e a cefaloridina. A concentracOes equivalentes a 1-2 vezes a concentracao Inibitória Minima (CIM) a cefotaxima revelou uma accAo bactericida mais rápida e completa sobre o E. -

FOR YOUR INFORMATION L I T a Mold Problem in 1972-73 Feed Grains Recognized As a Serious Problem by Various State Gibberella Zeae and Federal Agencies
r 1 Association Practitioners; Bovine open ofdistribution. access American Copyright © FOR YOUR INFORMATION L i t A Mold Problem in 1972-73 Feed Grains recognized as a serious problem by various state Gibberella Zeae and federal agencies. Research has been conducted What is it? largely by university personnel. Mycotoxins in Gibberella zeae is a mold (Fusarium roseum) grains should be recognized as emerging diseases found on com and some other field grains. It is a and of growing importance. The cold, wet growing naturally occurring fungus that is a serious problem season of 1972 was ideal for the production of during a wet, cold growing season and harvesting Fusarium mycoses. The delayed harvest contri period such as was experienced in 1972. The buted to the problem. Shortage of natural gas greatest problem areas in 1972 seem to be in made it more difficult to dry com. Normally, corn Southern Michigan, Northwestern Ohio, and is dried to 14% moisture. Much of this year’s com Northern Indiana — but reports indicate lesser had moisture levels ranging from 20 to 35%. contamination in a number of other corn- Twenty-three percent moisture has been recog producing states. nized as the minimal moisture level where Fusaria What are its effects? mycotoxin activity occurs. Three known factors produced by this mold What Treatment is Available? cause feeding problems to animals consuming it. Producers of Gibberella zeae contaminated com The “refusal factor” — animals refusing to eat it — have very little means available to reduce the the “emetic factor” — vomiting — are present in problem. Both the emetic and refusal factors are the contaminated grain, and result in reduced very stable to pH changes (pH 2.0-11.0) and to nutrition. -

TOBRAMYCIN Injection, USP Rx Only to Reduce the Development of Drug
TOBRAMYCIN Injection, USP Rx only To reduce the development of drug-resistant bacteria and maintain the effectiveness of tobramycin and other antibacterial drugs, tobramycin should be used only to treat or prevent infections that are proven or strongly suspected to be caused by bacteria. BOXED WARNING WARNINGS Patients treated with Tobramycin Injection, USP and other aminoglycosides should be under close clinical observation, because these drugs have an inherent potential for causing ototoxicity and nephrotoxicity. Neurotoxicity, manifested as both auditory and vestibular ototoxicity, can occur. The auditory changes are irreversible, are usually bilateral, and may be partial or total. Eighth-nerve impairment and nephrotoxicity may develop, primarily in patients having pre-existing renal damage and in those with normal renal function to whom aminoglycosides are administered for longer periods or in higher doses than those recommended. Other manifestations of neurotoxicity may include numbness, skin tingling, muscle twitching, and convulsions. The risk of aminoglycoside-induced hearing loss increases with the degree of exposure to either high peak or high trough serum concentrations. Patients who develop cochlear damage may not have symptoms during therapy to warn them of eighth-nerve toxicity, and partial or total irreversible bilateral deafness may continue to develop after the drug has been discontinued. Rarely, nephrotoxicity may not become apparent until the first few days after cessation of therapy. Aminoglycoside-induced nephrotoxicity usually is reversible. Renal and eighth-nerve function should be closely monitored in patients with known or suspected renal impairment and also in those whose renal function is initially normal but who develop signs of renal dysfunction during therapy. -

Suspension Formulation of Amoxicil Lin and Clavulanic Acid
AN ABSTRACT OF THESIS OF Ning-Ning Yang, for the degree of Master of Science in Pharmacy presented on June 11, 1997. Title: Product Formulations and In Vitro-In Vivo Evaluation of a Novel "Tablet-in-a-Bottle" Suspension Formulation of Amoxicil lin and Clavulanic Acid. Abstract approved: Redacted for Privacy This thesis describes a novel "Tablet-in-a-Bottle" oral suspension formulation. Ingredients with unstable physical or chemical characteristics can be placed in a core tablet, and then dry compression coated with an outer layer which provides separation from other components. The new suspension formulation comprises fast disintegrating clavulanic acid (KCA) tablets with a powder mixture containing amoxicillin. Hardness, friability, flow properties and weight uniformity of tablets for three different formulations were investigated and were all improved in a third formulation. Stability tests under different humidities were conducted. Amoxicillin and clavulanic acid in the new formulations showed the same stabilities when compared with the marketed product Augmentin®. Preliminary pharmacokinetics and bioavailability of one new formulation were evaluated by comparing in vitro release rates and in vivo urinary excretion rates. In vitro dissolution studies were carried out according to the USP )OCIII paddle method. The new formulation showed faster release rates during the first hour when stirring speed was 25 rpm. However, when 75 rpm stirring speed was applied, the dissolution profiles for the new formulation and the reference marketed product were identical. A randomized two-way crossover bioequivalence study was designed to evaluate the bioavailabilities. Cmax, Tmax and AUC0_9t of amoxicillin were within ±20% of the reference pharmacokinetic values. -

Penicillins and Cephalosporins to Penicillinase of Staphylococcus Aureus
J Clin Pathol: first published as 10.1136/jcp.30.1.35 on 1 January 1977. Downloaded from J. clin. Path., 1977, 30, 35-39 Susceptibility of the 'penicillinase-resistant' penicillins and cephalosporins to penicillinase of Staphylococcus aureus R. W. LACEY AND ANNE STOKES From the Department of Bacteriology, North Cambridgeshire Hospital, Wisbech, Cambridgeshire SUMMARY The activities of some semisynthetic penicillins and cephalosporins have been tested against clinical strains of Staphylococcus aureus. The apparent activity in vitro varies with the method of testing used. Determination of MICs using light inocula fails to detect the destructive effect of penicillinase on the antibiotic. This was, however, demonstrated reproducibly by the use of a technique in which a heavy inoculum was pre-incubated for two hours before application of antibiotic to wells. This method of testing probably represents most of the clinical situations in which the drugs are used since both in vitro and in vivo a growing culture is exposed to an antibiotic gradient. Flucloxacillin was inactivated by penicillinase considerably more than either methicillin, cloxacil- lin, or nafcillin. Cephaloridine was the most vulnerable of the cephalosporins. Cephazolin, cepha- copyright. lothin, and cephalexin were intermediate. Cephradine was the least hydrolysed by staphylococcal penicillinase. It is recommended that the activities of all penicillins and cephalosporins against staphylococci should be tested by diffusion at 37°C with pre-incubation of the culture for two hours at this temperature. http://jcp.bmj.com/ Determination of minimum inhibitory concentra- These enzymes are released into the media with little tions (MIC) has become accepted as the ideal method residual protein adherent to the cell. -

Phenomenon of Resistance to Augmentin Associated With
J Clin Pathol: first published as 10.1136/jcp.36.6.670 on 1 June 1983. Downloaded from J Clin Pathol 1983;36:670-673 Phenomenon of resistance to Augmentin associated with sensitivity to ampicillin: occurrence and explanation W BRUMFITT, JMT HAMILTON-MILLER, SHIRLEY DIXSON, RA GARGAN, ANN GOODING From the Department ofMedical Microbiology, Royal Free Hospital and School ofMedicine, Pond Street, London NW3 2QG SUMMARY Ampicillin was found to be some tenfold more active than amoxycillin against Enterobacter cloacae. This finding explains the observation that some Ent cloacae strains are sensitive to ampicillin in the disc test but resistant to Augmentin. Ampicillin was also found to be more active than amoxycillin against Citrobacter freundii and Serratia marcescens. In view of these findings, the practice of using ampicillin discs to predict sensitivity to amoxycillin should be reconsidered. The use of both ampicillin and amoxycillin discs is appropriate if errors are to be avoided. Amoxycillin has been shown to be at least as active Material and methods in vitro as ampicillin against many pathogenic bac- copyright. terial with notable exceptions, such as Haemophilus ANTIBIOTICS influenzae. Its bactericidal action in vitro and its Ampicillin trihydrate and amoxycillin trihydrate effectiveness in vivo seems to be superior to that of were Laboratory Reference Standards nos 29 and ampicillin.23 Further, amoxycillin is absorbed by 12, respectively, from Beecham Research mouth almost twice as well as ampicillin.' Because Laboratories. Sodium ampicillin was obtained from of these properties, amoxycillin can be given in a the hospital pharmacy. Sodium amoxycillin and smaller dose and less frequently than ampicillin, and potassium clavulanate were generously supplied by http://jcp.bmj.com/ it now enjoys wide clinical use. -
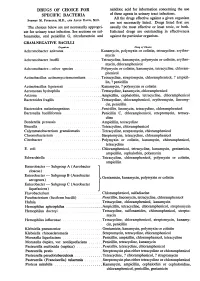
Aerogenes) Gentamicin, Enterobacter - Subgroup C (Aerobacter Liquefaciens) Flavobacterium
DRUGS OF CHOICE FOR nalidixic acid for information concerning the use SPECIFIC BACTERIA of these agents in urinary tract infections. All the drugs effective against a given organism SYDNEY M. FINEGOLD, M.D., AND ALVIN DAVIS, M.D. are not necessarily listed. Drugs listed first are The choices below are not necessarily appropri- usually the most effective or least toxic, or both. ate for urinary tract infection. See sections on sul- Italicized drugs are outstanding in effectiveness fonamides, oral penicillin G, nitrofurantoin and against the particular organism. GRAM-NEGATIVE BACILLI Organism Drag of Choice Achromobacter anitratus ................. Kanamycin, polymyxin or colistin, tetracycline, erythro- mycin Achromobacter lwoffii ................. Tetracycline, kanamycin, polymyxin or colistin, erythro- mycin, chloramphenicol Achromobacter-other species ... Polymyxin or colistin, kanamycin, tetracycline, chloram- phenicol Actinobacillus actinomycetemcomitans ..... Tetracycline, streptomycin, chloramphenicol, ? ampicil- lin, ? penicillin Actinobacillus lignieresii ......... Kanamycin, ? polymyxin or colistin Aeromonas hydrophila .................... Tetracycline, kanamycin, chloramphenicol Arizona ......................... Ampicillin, cephalothin, tetracycline, chloramphenicol Bacteroides fragilis ....................... Tetracycline, chloramphenicol, erythromycin, lincomy- cin, penicillin Bacteroides melaninogenicus .. ............ Penicillin, linomycin, tetracycline, chloramphenicol Bartonella bacilliformis ................... Penicillin