Anal Fissures David B
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

1311 Diploma in Medical Record Science Second
[LD 0212] AUGUST 2013 Sub. Code: 1311 DIPLOMA IN MEDICAL RECORD SCIENCE SECOND YEAR PAPER II – INTERNATIONAL CLASSIFICATION OF DISEASES (ICD-10) & SURGICAL PROCEDURES (ICM-9CM) Q.P. Code : 841311 Time : Three Hours Maximum : 100 marks Answer ALL questions I Write appropriate codes using ICD -10 (30 x 1 = 30) 1. Therapeutic introduction of hand tendon. 2. Excision of major partial thickness of eyelid excision. 3. Interphalangeal arthrodesis of Toe. 4. Division of percutaneous spinal cord nerve tracts. 5. Transfusion of allograft bone aetriosus. 6. Rastelli operation of truncus arteriosus. 7. Pyoloric sphincter dilatation. 8. Stapling of radius epiphyseal plate. 9. Suture of hands fascia. 10. Suture of hand fascia. 11. Repair of anterior wall (abdomen) hernia. 12. Foreign body removal without incision in t o the brain. 13. Repair of Tetrology of fallot. 14. Frontal Sinusectomy. 15. Urethral sling suspension. 16. Bone shaft transfer. 17. Coil of aneuryum repair. 18. Sling suspension. 19. Radio isotope scanning, pituitary gland. 20. Spinal shunt removal. 21. Acute lung edema. Due to external agent. 22. Proximal end tibial closed fracture was riding a two wheeler-slip & fell down. 23. Thrombosed internal hemorrhoids. 24. Secondary hypertension due to renal disorder. 25. Old myocardial infarction. 26. Fall from high place, injured elbow. 27. Chronic venous (peripheral) insufficiency. 28. Acute myeloid leukemia. 29. Post-operative intestine obstruction. 30. Abnormal pregnancy. II Writes appropriate codes using ICS-9CM (20 x 2 = 40) 1. Pregnant women suffering from acute salphingo oophoritis. 2. Accidental intake of ferrous salt. 3. Sprain of lumbar spine as stuck by another person. 4. -

Crohn's Disease of the Anal Region
Gut: first published as 10.1136/gut.6.6.515 on 1 December 1965. Downloaded from Gut, 1965, 6, 515 Crohn's disease of the anal region B. K. GRAY, H. E. LOCKHART-MUMMERY, AND B. C. MORSON From the Research Department, St. Mark's Hospital, London EDITORIAL SYNOPSIS This paper records for the first time the clinico-pathological picture of Crohn's disease affecting the anal canal. It has long been recognized that anal lesions may precede intestinal Crohn's disease, often by some years, but the specific characteristics of the lesion have not hitherto been described. The differential diagnosis is discussed in detail. In a previous report from this hospital (Morson and types of anal lesion when the patients were first seen Lockhart-Mummery, 1959) the clinical features and were as follows: pathology of the anal lesions of Crohn's disease were described. In that paper reference was made to Anal fistula, single or multiple .............. 13 several patients with anal fissures or fistulae, biopsy Anal fissures ........... ......... 3 of which showed a sarcoid reaction, but in whom Anal fissure and fistula .................... 3 there was no clinical or radiological evidence of Total 19 intra-abdominal Crohn's disease. The opinion was expressed that some of these patients might later The types of fistula included both low level and prove to have intestinal pathology. This present complex high level varieties. The majority had the contribution is a follow-up of these cases as well as clinical features described previously (Morson and of others seen subsequently. Lockhart-Mummery, 1959; Lockhart-Mummery Involvement of the anus in Crohn's disease has and Morson, 1964) which suggest Crohn's disease, http://gut.bmj.com/ been seen at this hospital in three different ways: that is, the lesions had an indolent appearance with 1 Patients who presented with symptoms of irregular undermined edges and absence of indura- intestinal Crohn's disease who, at the same time, ation. -

Pneumoperitoneum Due to a Transmural Anal Fissure by Glen Huang, Hussam Bitar
A CASE REPORT A CASE REPORT Pneumoperitoneum Due to a Transmural Anal Fissure by Glen Huang, Hussam Bitar Pneumoperitoneum is usually due to a perforated viscus and requires surgical intervention, however, a minority of cases can be managed nonsurgically. Nonsurgical pneumoperitoneum has a wide variety of causes, but a transmural anal fissure being the cause has yet to be documented. In this case we describe a case of pneumoperitoneum due to a transmural fissure caused by extreme diarrhea. INTRODUCTION nal fissures are common and typically result (Figure 1). This air appeared to be contiguous with a from mucosal tear. In traumatic cases, the tear transmural anal tear that was noted as well (Figure 2). may be transmural. These tears typically occur Complete blood count (CBC) demonstrated an elevated A 3 posteriorly to the midline and patients often present white blood cell count of 16.9 x 10 cells/µL (local with anal pain or rectal bleeding.1 Pneumoperitoneum control 3.8-10.79 x 103 cells/µL) with 87% neutrophils is a collection of air in the peritoneal cavity, typically (local control 40-79%). The rest of the CBC was within occurring from a ruptured hollow viscus. However, normal limits. cases of pneumoperitoneum without evidence of The patient was then admitted and given a full perforation can rarely occur.2 Here, we discuss a case of liquid diet to allow for bowel rest. He was also placed pneumoperitoneum secondary to an acute anal fissure. on intravenous antibiotics for the possibility of perianal cellulitis given his increased white blood cell count. -

How to Optimize Surgical Treatment of Chronic Anal Fissure Combined
Sys Rev Pharm 2020;11(11):171-176 A multHifaceotedwreviewtjournaOl in tphe ftielidmof phiarzmaecy Surgical Treatment of Chronic Anal Fissure Combined With Rectocele In Women BV.eFl.gKоruоlidkNоvastikоyn,aNl .RVe. sОelaeryсnhiUk,nAiv.Pe.rsKirtyiv, сRhuisksоiav,a3,0M80.S1.5A,lBeneligсhоerоvda,, PYоabroedsyh SAt..L,.85 ABSTRACT Anal fissure is a common condition in women of all ages. The most common Keywords: anal fissure, rectocele, surgical treatment, wound healing causes are childbirth and constipation. Anal fissure is often diagnosed in women with rectocele. Unsatisfactory results of surgical treatment of chronic anal fissures Correspondence: in patients with rectocele enforce to continue the investigations for the optimal V.F. Kulikоvsky solution of this problem. Belgоrоd Natiоnal Researсh University, Russia,308015, Belgоrоd, Pоbedy St., 85 The aim of research was to improve the results of surgical treatment of chronic anal fissures in patients with rectocele. Materials and Methods. In 2015-2019, on the basis of the Surgery Department of Belgоrоd Natiоnal Researсh University and Coloproctology Department of Belgorod St. Joasaph's Hospital, we conducted a comparative assessment of the results of surgical treatment of 74 patients with recocele and chronic anal fissure, who underwent isolated surgery of anal fissure excision (1st group, n=35) and anal fissure excision, combined with posterior colporrhaphy in the 2nd group (n=39). According to indications for spasm of the internal anal sphincter, in patients of both groups internal lateral sphincterotomy was performed. Results. Local pain syndrome in the anus area in the first day after the operation in all patients was intensive. Starting from the 2nd day, the pain in the area of the vaginal wound of the patients of the 2nd group almost did not bother them. -

Code Procedure Cpt Price University Physicians Group
UNIVERSITY PHYSICIANS GROUP (UPG) PRICES OF PROVIDER SERVICES CODE PROCEDURE MOD CPT PRICE 0001A IMM ADMN SARSCOV2 30MCG/0.3ML DIL RECON 1ST DOSE 0001A $40.00 0002A IMM ADMN SARSCOV2 30MCG/0.3ML DIL RECON 2ND DOSE 0002A $40.00 0011A IMM ADMN SARSCOV2 100 MCG/0.5 ML 1ST DOSE 0011A $40.00 0012A IMM ADMN SARSCOV2 100 MCG/0.5 ML 2ND DOSE 0012A $40.00 0021A IMM ADMN SARSCOV2 5X1010 VP/0.5 ML 1ST DOSE 0021A $40.00 0022A IMM ADMN SARSCOV2 5X1010 VP/0.5 ML 2ND DOSE 0022A $40.00 0031A IMM ADMN SARSCOV2 AD26 5X10^10 VP/0.5 ML 1 DOSE 0031A $40.00 0042T CEREBRAL PERFUS ANALYSIS, CT W/CONTRAST 0042T $954.00 0054T BONE SURGERY USING COMPUTER ASSIST, FLURO GUIDED 0054T $640.00 0055T BONE SURGERY USING COMPUTER ASSIST, CT/ MRI GUIDED 0055T $1,188.00 0071T U/S LEIOMYOMATA ABLATE <200 CC 0071T $2,500.00 0075T 0075T PR TCAT PLMT XTRC VRT CRTD STENT RS&I PRQ 1ST VSL 26 26 $2,208.00 0126T CAROTID INT-MEDIA THICKNESS EVAL FOR ATHERSCLER 0126T $55.00 0159T 0159T COMPUTER AIDED BREAST MRI 26 26 $314.00 PR RECTAL TUMOR EXCISION, TRANSANAL ENDOSCOPIC 0184T MICROSURGICAL, FULL THICK 0184T $2,315.00 0191T PR ANT SEGMENT INSERTION DRAINAGE W/O RESERVOIR INT 0191T $2,396.00 01967 ANESTH, NEURAXIAL LABOR, PLAN VAG DEL 01967 $2,500.00 01996 PR DAILY MGMT,EPIDUR/SUBARACH CONT DRUG ADM 01996 $285.00 PR PERQ SAC AGMNTJ UNI W/WO BALO/MCHNL DEV 1/> 0200T NDL 0200T $5,106.00 PR PERQ SAC AGMNTJ BI W/WO BALO/MCHNL DEV 2/> 0201T NDLS 0201T $9,446.00 PR INJECT PLATELET RICH PLASMA W/IMG 0232T HARVEST/PREPARATOIN 0232T $1,509.00 0234T PR TRANSLUMINAL PERIPHERAL ATHERECTOMY, RENAL -

What Is an Anal Fissure?
What is an Anal Fissure? This is a fairly common condition (number one cause of anal pain and bleeding -- more common than hemorrhoids) in which the lining of the anal canal becomes torn. This generally produces pain or burning, especially with passage of a bowel movement. Bleeding may also occur. A fissure usually occurs with constipation or after forceful passage of a large, hard bowel movement. However, fissures also may occur without straining, since the tissue lining the anal canal is very delicate. How is a fissure diagnosed? When a fissure is present, a digital rectal exam is usually painful. The fissure can be usually be visualized by an external inspection of the anus, or an anoscope can be used to determine the extent of the tear. How is a fissure treated? • Warm tub or sitz baths several times a day in plain warm water for about 10 minutes. • Stool softeners or fiber to provide a regular soft, formed bowel movement. • Creams and/or suppositories (Preparation-H or Anusol or product with lidocaine added). • May add Nitroglycerin to anus to relieve spasm and pain thus allow healing. Most fissures will heal within several weeks, but surgery may be necessary if symptoms persist. Surgical treatment usually consists of cutting a portion of the muscle in the anal canal (sphincterotomy). This procedure reduces the tension produced by the fissure and allows it to heal. Of course, the best treatment is prevention, and ingestion of a high fiber diet to promote bowel regularity is of utmost importance. What do you do After. .? (Anal discomfort and how to deal with it) By: W. -

Anal Fissure
Anal Fissure What is an anal fissure? An anal fissure is a small tear in the skin of the anus. The anus is the opening of the rectum where bowel movements (BMs) leave the body. Anal fissures are a fairly common problem. What is the cause? A tear may happen when you have: • Hard, dry bowel movements • Constipation • Hemorrhoids • Anal surgery • Inflammation of the rectum caused by intestinal problems such as Crohn's disease What are the symptoms? Symptoms may include: • Pain during or after bowel movements • Cramping of the muscle at the opening of the anus caused by irritation of the tear during a bowel movement • Bright red blood when you have a bowel movement (you may see the blood on the BM, in the toilet water, or on toilet tissue you have used) How is it diagnosed? Your healthcare provider will ask about your symptoms and examine you. You may have a procedure called an anoscopy to confirm the diagnosis. For this procedure your provider uses a small tool with a light called an anoscope to examine the anus and lower part of the rectum. Your healthcare provider may recommend other tests or procedures, such as a sigmoidoscopy or colonoscopy, to learn more about the cause of the fissure or the bleeding. How is it treated? Most fissures will heal with the following at-home treatments: • Your healthcare provider may recommend a stool softener, such as Haley's M-O, psyllium, Metamucil or Citrucel, or mineral oil. • It may help to drink lots of water and add more fiber to your diet. -
PSI Appendix a Version 6.0 Patient Safety Indicators Appendices
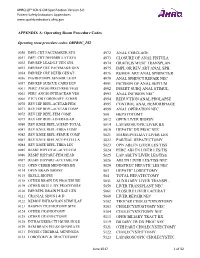
AHRQ QI™ ICD-9-CM Specification Version 6.0 Patient Safety Indicators Appendices www.qualityindicators.ahrq.gov APPENDIX A: Operating Room Procedure Codes Operating room procedure codes: ORPROC_PSI 0050 IMPL CRT PACEMAKER SYS 4972 ANAL CERCLAGE 0051 IMPL CRT DEFIBRILLAT SYS 4973 CLOSURE OF ANAL FISTULA 0052 IMP/REP LEAD LF VEN SYS 4974 GRACILIS MUSC TRANSPLAN 0053 IMP/REP CRT PACEMAKR GEN 4975 IMPL OR REV ART ANAL SPH 0054 IMP/REP CRT DEFIB GENAT 4976 REMOV ART ANAL SPHINCTER 0056 INS/REP IMPL SENSOR LEAD 4979 ANAL SPHINCT REPAIR NEC 0057 IMP/REP SUBCUE CARD DEV 4991 INCISION OF ANAL SEPTUM 0061 PERC ANGIO PRECEREB VESS 4992 INSERT SUBQ ANAL STIMUL 0062 PERC ANGIO INTRACRAN VES 4993 ANAL INCISION NEC 0066 PTCA OR CORONARY ATHER 4994 REDUCTION ANAL PROLAPSE 0070 REV HIP REPL-ACETAB/FEM 4995 CONTROL ANAL HEMORRHAGE 0071 REV HIP REPL-ACETAB COMP 4999 ANAL OPERATION NEC 0072 REV HIP REPL-FEM COMP 500 HEPATOTOMY 0073 REV HIP REPL-LINER/HEAD 5012 OPEN LIVER BIOPSY 0080 REV KNEE REPLACEMT-TOTAL 5014 LAPAROSCOPIC LIVER BX 0081 REV KNEE REPL-TIBIA COMP 5019 HEPATIC DX PROC NEC 0082 REV KNEE REPL-FEMUR COMP 5021 MARSUPIALIZAT LIVER LES 0083 REV KNEE REPLACE-PATELLA 5022 PARTIAL HEPATECTOMY 0084 REV KNEE REPL-TIBIA LIN 5023 OPN ABLTN LIVER LES/TISS 0085 RESRF HIPTOTAL-ACET/FEM 5024 PERC ABLTN LIVER LES/TIS 0086 RESRF HIPPART-FEM HEAD 5025 LAP ABLTN LIVER LES/TISS 0087 RESRF HIPPART-ACETABLUM 5026 ABLTN LIVER LES/TISS NEC 0112 OPEN CEREB MENINGES BX 5029 DESTRUC HEPATIC LES NEC 0114 OPEN BRAIN BIOPSY 503 HEPATIC LOBECTOMY 0115 SKULL BIOPSY 504 TOTAL -
Curriculum Outline General Surgery
CURRICULUM OUTLINE FOR GENERAL SURGERY 2018–2019 Surgical Council on Resident Education 1617 John F. Kennedy Boulevard Suite 860 Philadelphia, PA 19103 1-877-825-9106 [email protected] www.surgicalcore.org SCORE Curriculum Outline for General Surgery The SCORE® Curriculum Outline for General Surgery is a list of topics to be covered in a five- year general surgery residency program. The outline is updated annually to remain contempo- rary and reflect feedback from SCORE member organizations and specialty surgical societies. Topics are listed for all six competencies of the Accreditation Council for Graduate Medical Education (ACGME): patient care; medical knowledge; professionalism; interpersonal and communication skills; practice-based learning and improvement; and systems-based practice. The patient care topics cover 27 organ system- based categories, with each category separated into Diseases/Conditions and Operations/ Procedures. Topics within these two areas are then designated as Core or Advanced. Changes from the previous edition are indi- cated in the Excel version of this outline, avail- able at www.surgicalcore.org. Note that topics listed in this booklet may not directly match those currently on the SCORE Portal — this outline is forward-looking, reflecting the latest updates. The Surgical Council on Resident Education (SCORE) is a nonprofit consortium formed in 2006 by the principal organizations involved in U.S. surgical education. SCORE’s mission is to improve the education of general surgery residents through the development of a national curriculum for general surgery residency training. The members of SCORE are: American Board of Surgery American College of Surgeons American Surgical Association Association of Program Directors in Surgery Association for Surgical Education Review Committee for Surgery of the ACGME Society of American Gastrointestinal and Endoscopic Surgeons PATIENT CARE CONTENTS Page BY CATEGORY ............................................ -

Icd-9-Cm (2010)
ICD-9-CM (2010) PROCEDURE CODE LONG DESCRIPTION SHORT DESCRIPTION 0001 Therapeutic ultrasound of vessels of head and neck Ther ult head & neck ves 0002 Therapeutic ultrasound of heart Ther ultrasound of heart 0003 Therapeutic ultrasound of peripheral vascular vessels Ther ult peripheral ves 0009 Other therapeutic ultrasound Other therapeutic ultsnd 0010 Implantation of chemotherapeutic agent Implant chemothera agent 0011 Infusion of drotrecogin alfa (activated) Infus drotrecogin alfa 0012 Administration of inhaled nitric oxide Adm inhal nitric oxide 0013 Injection or infusion of nesiritide Inject/infus nesiritide 0014 Injection or infusion of oxazolidinone class of antibiotics Injection oxazolidinone 0015 High-dose infusion interleukin-2 [IL-2] High-dose infusion IL-2 0016 Pressurized treatment of venous bypass graft [conduit] with pharmaceutical substance Pressurized treat graft 0017 Infusion of vasopressor agent Infusion of vasopressor 0018 Infusion of immunosuppressive antibody therapy Infus immunosup antibody 0019 Disruption of blood brain barrier via infusion [BBBD] BBBD via infusion 0021 Intravascular imaging of extracranial cerebral vessels IVUS extracran cereb ves 0022 Intravascular imaging of intrathoracic vessels IVUS intrathoracic ves 0023 Intravascular imaging of peripheral vessels IVUS peripheral vessels 0024 Intravascular imaging of coronary vessels IVUS coronary vessels 0025 Intravascular imaging of renal vessels IVUS renal vessels 0028 Intravascular imaging, other specified vessel(s) Intravascul imaging NEC 0029 Intravascular -

Pediatric and Adolescent Gastrointestinal Motility & Pain
Defecation Disorders After Surgery for Hirschsprung's Disease Pediatric and Adolescent Gastrointestinal Motility & Pain Program Department of Pediatrics, Louisiana State University Health Sciences Center, New Orleans, Louisiana Over 1000 new cases of Hirschsprung’s disease are diagnosed in the USA every year. More than half the children treated appropriately with surgery for Hirschsprung’s disease suffer from chronic problems with constipation, incontinence, and/or abdominal pain. Even as adults, over half will experience occasional episodes of incontinence, and 10% will endure constipation unresponsive to medical management. In the six decades since Ovar Swenson recognized that the distal bowel segment lacking ganglion cells was the diseased portion and created the first successful surgical technique, surgeons have been frustrated with the imperfect response to a surgery which eliminates the disease. Parents have been frustrated and children shamed by the inability to gain control over their bowel movements. Over the past 10 years the pediatric motility community has discovered reasons and solutions for chronic post-operative problems. It is now clear that the child is not lazy or uncooperative, but has recognizable and treatable causes for the symptoms. Constipation There are three mechanisms for constipation: functional constipation (also called functional fecal retention), neuropathy proximal to the aganglionic segment, and hypertensive anal sphincter. It is not easy to distinguish among these conditions when they follow Hirschsprung’s disease surgery. Only colon and anorectal manometry clarify the diagnosis and treatment. Functional constipation Functional constipation is the most common condition referred to pediatric gastroenterology clinics. It arises when an infant or toddler has a painful bowel movement. -

Approved Surgical Procedures
UNION MEDICAL BENEFITS SOCIETY LTD APPROVED SURGICAL PROCEDURES The following list of surgical procedures should be read in conjunction with your policy document. If you are intending to have one of the listed procedures, please call our surgical team on 0800 600 666 so we can guide you through the prior approval process. If a surgical procedure is not listed below, it will not be covered unless UniMed decides, in its sole discretion, to offer cover. CARDIAC GENERAL • Pericardiotomy Breast • Pericardiocentesis • Breast Cyst Aspiration or Needle Biopsy • Drainage of Pericaridal Effusion • Breast Biopsy • Coronary Artery Bypass (using vein or artery) • Core Biopsy of Breast • Open Repair of Atrial Septal Defect (ASD) • Excision Accessary Breast Tissue • Valvuloplasty • Mastectomy • Aortic/ Mitral Valve Replacement via Sternotomy • Sentinel Node Biopsy with/without Axillary Dissection • Pulmonary Valve Replacement via Sternotomy • Breast Microdochotomy • Tricuspid Valve Replacement via Sternotomy • Balloon Valvuloplasty – Mitral/ Aortic Reconstruction Post Mastectomy • Pacemaker Surgery – Initial Implantation (Excluding the Cost • Breast/ Nipple Reconstruction of the Pacemaker) • Nipple Areolar Tattoo • Removal of Sternal Wire • Maze Arrhythmia Surgery Gastrointestinal • Removal & Rewiring of Sternal Wire • Anal Sphincterotomy • Maze Arrhythmia Surgery (Standalone procedure) • Simple Repair of Anal Fistula – Special approval only • Maze Procedure – Thoracoscopic • Anal Fistula Repair with Mucosal Advancement Flap • Bentall’s Procedure (includes