General Ataxia Leaflet
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Syndrome-Based Clinical Approach for Clerkship Students General Comments 1. This Is Not an All-Inclusive “Cookbook” for Ev
A Syndrome-Based Clinical Approach for Clerkship Students General Comments 1. This is not an all-inclusive “cookbook” for every Neurology patient, but a set of guidelines to help you rationally approach patients with certain syndromes (sets of signs and symptoms which suggest a lesion in particular parts of the nervous system). 2. As you obtain a history and perform a neurological physical exam, try initially to localize all the patient’s signs and symptoms to one, single lesion in the nervous system. It may be surprising that a variety of signs and symptoms, at first glance apparently unrelated, on second thought can localize accurately to a single lesion. If this approach fails, then consider multiple, separate lesions for the patient’s signs and symptoms. 3. The tempo or rate at which signs and symptoms develop or occur often suggests the underlying pathological process. a. sudden onset---favors stroke (ischemia or hemorrhage), seizure, migraine (or other headache syndromes), and trauma b. subacute onset---favors inflammatory, infectious or immune-mediated disorders c. chronic onset---favors degenerative disorders, tumors Toximetabolic disorders, potentially treatable and reversible, may mimic lesions in the nervous system, and can evolve at variable tempos. Hereditary conditions may be congenital (present at birth) and nonprogressive or static, or develop later in life, with variable rates of progression. Family members affected by the same genetic disorder may be remarkably similar with regards to onset and clinical severity, while some genetic disorders vary widely regarding when and how severely family members are affected. 4. In the central nervous system, “positive symptoms or phenomena,” such as flashes of light, or a tingling sensation, suggest “excitation” or increased activity in the nervous system: migraine or seizure. -

Child Neurology: Hereditary Spastic Paraplegia in Children S.T
RESIDENT & FELLOW SECTION Child Neurology: Section Editor Hereditary spastic paraplegia in children Mitchell S.V. Elkind, MD, MS S.T. de Bot, MD Because the medical literature on hereditary spastic clinical feature is progressive lower limb spasticity B.P.C. van de paraplegia (HSP) is dominated by descriptions of secondary to pyramidal tract dysfunction. HSP is Warrenburg, MD, adult case series, there is less emphasis on the genetic classified as pure if neurologic signs are limited to the PhD evaluation in suspected pediatric cases of HSP. The lower limbs (although urinary urgency and mild im- H.P.H. Kremer, differential diagnosis of progressive spastic paraplegia pairment of vibration perception in the distal lower MD, PhD strongly depends on the age at onset, as well as the ac- extremities may occur). In contrast, complicated M.A.A.P. Willemsen, companying clinical features, possible abnormalities on forms of HSP display additional neurologic and MRI abnormalities such as ataxia, more significant periph- MD, PhD MRI, and family history. In order to develop a rational eral neuropathy, mental retardation, or a thin corpus diagnostic strategy for pediatric HSP cases, we per- callosum. HSP may be inherited as an autosomal formed a literature search focusing on presenting signs Address correspondence and dominant, autosomal recessive, or X-linked disease. reprint requests to Dr. S.T. de and symptoms, age at onset, and genotype. We present Over 40 loci and nearly 20 genes have already been Bot, Radboud University a case of a young boy with a REEP1 (SPG31) mutation. Nijmegen Medical Centre, identified.1 Autosomal dominant transmission is ob- Department of Neurology, PO served in 70% to 80% of all cases and typically re- Box 9101, 6500 HB, Nijmegen, CASE REPORT A 4-year-old boy presented with 2 the Netherlands progressive walking difficulties from the time he sults in pure HSP. -

Diagnostic Clues in Multiple System Atrophy
DO I:10.4274/Tnd.82905 Case Report / Olgu Sunumu Diagnostic Clues in Multiple System Atrophy: A Case Report and Literature Review Multisistem Atrofi Tanısında İpuçları: Bir Olgu Sunumu ve Literatürün Gözden Geçirilmesi Mehmet Yücel, Oğuzhan Öz, Hakan Akgün, Semai Bek, Tayfun Kaşıkçı, İlter Uysal, Yaşar Kütükçü, Zeki Odabaşı Gülhane Military Medical Academy, Ankara, Turkey Sum mary Multiple system atrophy (MSA) is an adult-onset, sporadic, progressive neurodegenerative disease. Based on the consensus criteria, patients with MSA are clinically classified into cerebellar (MSA-C) and parkinsonian (MSA-P) subtypes. In addition to major diagnostic criteria including poor response to levodopa, and presence of pyramidal or cerebellar signs (ataxia) or autonomic failure, certain clinical features or ‘‘red flags’’ may raise the clinical suspicion for MSA. In our case report we present a 67-year-old female patient admitted to our hospital due to inability to walk, with poor response to levodopa therapy, whose neurological examination revealed severe Parkinsonism, ataxia and who fulfilled all criteria for MSA, as rarely seen in clinical practice.(Turkish Journal of Neurology 2013; 19:28-30) Key Words: Multiple system atrophy, autonomic failure, diagnostic criteria Özet Multisistem atrofi (MSA) erişkin dönemde başlayan, ilerleyici, nedeni bilinmeyen sporadik nörodejeneratif bir hastalıktır. MSA kabul görmüş tanı kriterlerine göre klinik olarak serebellar (MSA-C) ve parkinsoniyen (MSA-P) alt tiplerine ayrılmaktadır. Düşük levadopa yanıtı, piramidal, serebellar bulguların (ataksi) ya da otonomik bozukluk olması gibi majör tanı kriterlerininin yanında “red flags” olarak isimlendirilen belirgin klinik bulgular ya da uyarı işaretlerinin olması MSA tanısı için klinik şüpheyi oluşturmalıdır. Olgu sunumunda 67 yaşında yürüyememe şikayeti ile polikliniğimize müracaat eden ve levadopa tedavisine düşük yanıt gösteren ciddi parkinsonizm bulguları ile ataksi bulunan kadın hasta MSA tanı kriterlerini tam olarak karşıladığı ve klinik pratikte nadir görüldüğü için sunduk. -
Hereditary Ataxia Multigene Panel Testing
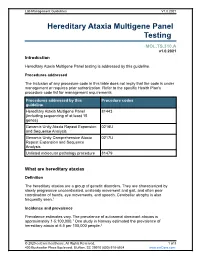
Lab Management Guidelines V1.0.2021 Hereditary Ataxia Multigene Panel Testing MOL.TS.310.A v1.0.2021 Introduction Hereditary Ataxia Multigene Panel testing is addressed by this guideline. Procedures addressed The inclusion of any procedure code in this table does not imply that the code is under management or requires prior authorization. Refer to the specific Health Plan's procedure code list for management requirements. Procedures addressed by this Procedure codes guideline Hereditary Ataxia Multigene Panel 81443 (including sequencing of at least 15 genes) Genomic Unity Ataxia Repeat Expansion 0216U and Sequence Analysis Genomic Unity Comprehensive Ataxia 0217U Repeat Expansion and Sequence Analysis Unlisted molecular pathology procedure 81479 What are hereditary ataxias Definition The hereditary ataxias are a group of genetic disorders. They are characterized by slowly progressive uncoordinated, unsteady movement and gait, and often poor coordination of hands, eye movements, and speech. Cerebellar atrophy is also frequently seen.1 Incidence and prevalence Prevalence estimates vary. The prevalence of autosomal dominant ataxias is approximately 1-5:100,000.1 One study in Norway estimated the prevalence of hereditary ataxia at 6.5 per 100,000 people.2 © 2020 eviCore healthcare. All Rights Reserved. 1 of 8 400 Buckwalter Place Boulevard, Bluffton, SC 29910 (800) 918-8924 www.eviCore.com Lab Management Guidelines V1.0.2021 Symptoms Although hereditary ataxias are made up of multiple different conditions, they are characterized by slowly progressive uncoordinated, unsteady movement and gait, and often poor coordination of hands, eye movements, and speech. Cerebellar atrophy is also frequently seen.1 Cause Hereditary ataxias are caused by mutations in one of numerous genes. -

Hereditary Spastic Paraplegia
8 Hereditary Spastic Paraplegia Notes and questions Hereditary Spastic Paraplegia What is Hereditary Spastic Paraplegia? Hereditary Spastic Paraplegia (HSP) is a medical term for a condition that affects muscle function. The terms spastic and paraplegia comes from several words in Greek: • ‘spastic’ means afflicted with spasms (an alteration in muscle tone that results in affected movements) • ‘paraplegia’ meaning an impairment in motor or sensory function of the lower extremities (from the hips down) What are the signs and symptoms of HSP? Muscular spasticity • Individuals with HSP commonly will have lower extremity weakness, spasticity, and muscle stiffness. • This can cause difficulty with walking or a “scissoring” gait. We are grateful to an anonymous donor for making a kind and Other common signs or symptoms include: generous donation to the Neuromuscular and Neurometabolic Centre. • urinary urgency • overactive or over responsive “brisk” reflexes © Hamilton Health Sciences, 2019 PD 9983 – 01/2019 Dpc/pted/HereditarySpasticParaplegia-trh.docx dt/January 15, 2019 ____________________________________________________________________________ 2 7 Hereditary Spastic Paraplegia Hereditary Spastic Paraplegia HSP is usually a chronic or life-long disease that affects If you have any questions about DM1, please speak with your people in different ways. doctor, genetic counsellor, or nurse at the Neuromuscular and Neurometabolic Centre. HSP can be classified as either “Uncomplicated HSP” or “Complicated HSP”. Notes and questions Types of Hereditary Spastic Paraplegia 1. Uncomplicated HSP: • Individuals often experience difficulty walking as the first symptom. • Onset of symptoms can begin at any age, from early childhood through late adulthood. • Symptoms may be non-progressive, or they may worsen slowly over many years. -

Functional Neurologic Disorders and Related Disorders Victor W Mark MD ( Dr
Functional neurologic disorders and related disorders Victor W Mark MD ( Dr. Mark of the University of Alabama at Birmingham has no relevant financial relationships to disclose. ) Originally released April 18, 2001; last updated December 13, 2018; expires December 13, 2021 Introduction This article includes discussion of psychogenic neurologic disorders, functional neurologic disorder, functional movement disorder, conversion disorder, and hysteria. The foregoing terms may include synonyms, similar disorders, variations in usage, and abbreviations. Overview Several behavioral disorders are related by (1) their resemblance to other, more familiar neurologic disorders; (2) lack of well-established biomarkers (eg, structural lesions on brain imaging studies, seizure waveforms on EEGs); and (3) aggravation of symptoms with the patient s attention to the disorder. However, the features and causes for these disorders are very different among themselves. This topic reviews functional neurologic disorder, Munchausen syndrome, Munchausen syndrome by proxy, and Ganser syndrome. Key points • Functional neurologic disorders are commonly encountered in general neurologic practices and, hence, knowing their manifestations and treatment is crucial for clinical care. • The disturbance is involuntary, yet at the same time it can be controlled by the patient intermittently. • Despite being self-controllable, the disturbance is generally disabling unless expert professional care is provided. • There is no consistent association between functional neurologic disorder and either posttraumatic emotional stress or sexual abuse. • Functional neurologic disturbances disorder responds best to empathetic concern by the clinician; demonstration that the disorder lacks a structural or permanent etiology; explanation that it can be improved with distraction; and guided attempts to reduce triggers of onset. Cognitive behavioral therapy, combined with physical therapy when warranted, is emerging as a successful intervention. -

KIF1A Missense Mutations in SPG30, an Autosomal Recessive Spastic Paraplegia: Distinct Phenotypes According to the Nature of the Mutations
European Journal of Human Genetics (2012) 20, 645–649 & 2012 Macmillan Publishers Limited All rights reserved 1018-4813/12 www.nature.com/ejhg ARTICLE KIF1A missense mutations in SPG30, an autosomal recessive spastic paraplegia: distinct phenotypes according to the nature of the mutations Stephan Klebe1,2,3,4,5,6, Alexander Lossos7, Hamid Azzedine1,3,4, Emeline Mundwiller1,3,4, Ruth Sheffer7, Marion Gaussen1,3,4, Cecilia Marelli2, Magdalena Nawara1,3,4, Wassila Carpentier8, Vincent Meyer9,10, Agne`s Rastetter1,3,4,11, Elodie Martin1,3,4,11, Delphine Bouteiller1,3,4, Laurent Orlando1,3,4,11, Gabor Gyapay9, Khalid H El-Hachimi1,3,4,11, Batel Zimmerman7, Moriya Gamliel7, Adel Misk12, Israela Lerer7, Alexis Brice*,1,2,3,4,6, Alexandra Durr1,2,3,4,6 and Giovanni Stevanin*,1,2,3,4,11 The hereditary spastic paraplegias (HSPs) are a clinically and genetically heterogeneous group of neurodegenerative diseases characterised by progressive spasticity in the lower limbs. The nosology of autosomal recessive forms is complex as most mapped loci have been identified in only one or a few families and account for only a small percentage of patients. We used next-generation sequencing focused on the SPG30 chromosomal region on chromosome 2q37.3 in two patients from the original linked family. In addition, wide genome scan and candidate gene analysis were performed in a second family of Palestinian origin. We identified a single homozygous mutation, p.R350G, that was found to cosegregate with the disease in the SPG30 kindred and was absent in 970 control chromosomes while affecting a strongly conserved amino acid at the end of the motor domain of KIF1A. -
Multiple System Atrophy
Multiple System Atrophy U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES Public Health Service National Institutes of Health Multiple System Atrophy What is multiple system atrophy? ultiple system atrophy (MSA) is M a progressive neurodegenerative disorder characterized by a combination of symptoms that affect both the autonomic nervous system (the part of the nervous system that controls involuntary action such as blood pressure or digestion) and move- ment. The symptoms reflect the progressive loss of function and death of different types of nerve cells in the brain and spinal cord. Symptoms of autonomic failure that may be seen in MSA include fainting spells and prob- lems with heart rate, erectile dysfunction, and bladder control. Motor impairments (loss of or limited muscle control or movement, or limited mobility) may include tremor, rigidity, and/or loss of muscle coordination as well as difficulties with speech and gait (the way a person walks). Some of these features are similar to those seen in Parkinson’s disease, and early in the disease course it often may be difficult to distinguish these disorders. MSA is a rare disease, affecting potentially 15,000 to 50,000 Americans, including men and women and all racial groups. Symptoms tend to appear in a person’s 50s and advance rapidly over the course of 5 to 10 years, with progressive loss of motor function and 1 eventual confinement to bed. People with MSA often develop pneumonia in the later stages of the disease and may suddenly die from cardiac or respiratory issues. While some of the symptoms of MSA can be treated with medications, currently there are no drugs that are able to slow disease progression and there is no cure. -

ICD9 & ICD10 Neuromuscular Codes
ICD-9-CM and ICD-10-CM NEUROMUSCULAR DIAGNOSIS CODES ICD-9-CM ICD-10-CM Focal Neuropathy Mononeuropathy G56.00 Carpal tunnel syndrome, unspecified Carpal tunnel syndrome 354.00 G56.00 upper limb Other lesions of median nerve, Other median nerve lesion 354.10 G56.10 unspecified upper limb Lesion of ulnar nerve, unspecified Lesion of ulnar nerve 354.20 G56.20 upper limb Lesion of radial nerve, unspecified Lesion of radial nerve 354.30 G56.30 upper limb Lesion of sciatic nerve, unspecified Sciatic nerve lesion (Piriformis syndrome) 355.00 G57.00 lower limb Meralgia paresthetica, unspecified Meralgia paresthetica 355.10 G57.10 lower limb Lesion of lateral popiteal nerve, Peroneal nerve (lesion of lateral popiteal nerve) 355.30 G57.30 unspecified lower limb Tarsal tunnel syndrome, unspecified Tarsal tunnel syndrome 355.50 G57.50 lower limb Plexus Brachial plexus lesion 353.00 Brachial plexus disorders G54.0 Brachial neuralgia (or radiculitis NOS) 723.40 Radiculopathy, cervical region M54.12 Radiculopathy, cervicothoracic region M54.13 Thoracic outlet syndrome (Thoracic root Thoracic root disorders, not elsewhere 353.00 G54.3 lesions, not elsewhere classified) classified Lumbosacral plexus lesion 353.10 Lumbosacral plexus disorders G54.1 Neuralgic amyotrophy 353.50 Neuralgic amyotrophy G54.5 Root Cervical radiculopathy (Intervertebral disc Cervical disc disorder with myelopathy, 722.71 M50.00 disorder with myelopathy, cervical region) unspecified cervical region Lumbosacral root lesions (Degeneration of Other intervertebral disc degeneration, -

Hyperpigmentation
J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.46.8.743 on 1 August 1983. Downloaded from Journal of Neurology, Neurosurgery, and Psychiatry 1983;46:743-744 Familial spinocerebellar ataxia with skin hyperpigmentation MICHAEL DARAS, ALAN J TUCHMAN, SHANTHA DAVID From the Department ofNeurology, New York Medical College, Lincoln Hospital, Bronx, New York, USA SUMMARY Previous reports have shown the association between familial spastic paraplegia and hypopigmentation of the skin. A family is reported in which three siblings presented with pro- gressive spastic paraparesis and cerebellar ataxia. All the siblings had large hyperpigmented naevi of the lower extremities while none of the unaffected members had a skin lesion. A definite association appears to exist between heredo-familial ataxias and disordered skin pigmentation, but the exact mechanism remains unclear. Many syndromes with disordered skin pigmentation pin and temperature senses were normal but position and and abnormalities of the nervous system have been vibration sense were decreased in both feet. Routine described. In two recent reports' 2 two families with laboratory investigations, including blood count and familial spastic paraplegia were described, in which chemistry, urinalysis, serum B-12 level, VDRL, EKG, and Protected by copyright. hypopigmentation of the skin was present in the chest, skull and complete spine radiographs were normal. affected members. We describe a family with,late Examination of the spinaflfluid was also normal. Computed onset progressive spastic paraplegia with cerebellar tomography of the head revealed bilateral cerebellar ataxia in which the three affected members have hemispheric atrophy. Motor nerve conduction velocities, hyperpigmented naevi in the lower sensory nerve latencies and electromyogram were normal. -

Hereditary Spastic Paraplegias
Hereditary Spastic Paraplegias Authors: Doctors Enza Maria Valente1 and Marco Seri2 Creation date: January 2003 Update: April 2004 Scientific Editor: Doctor Franco Taroni 1Neurogenetics Istituto CSS Mendel, Viale Regina Margherita 261, 00198 Roma, Italy. e.valente@css- mendel.it 2Dipartimento di Medicina Interna, Cardioangiologia ed Epatologia, Università degli studi di Bologna, Laboratorio di Genetica Medica, Policlinico S.Orsola-Malpighi, Via Massarenti 9, 40138 Bologna, Italy.mailto:[email protected] Abstract Keywords Disease name and synonyms Definition Classification Differential diagnosis Prevalence Clinical description Management including treatment Diagnostic methods Etiology Genetic counseling Antenatal diagnosis References Abstract Hereditary spastic paraplegias (HSP) comprise a genetically and clinically heterogeneous group of neurodegenerative disorders characterized by progressive spasticity and hyperreflexia of the lower limbs. Clinically, HSPs can be divided into two main groups: pure and complex forms. Pure HSPs are characterized by slowly progressive lower extremity spasticity and weakness, often associated with hypertonic urinary disturbances, mild reduction of lower extremity vibration sense, and, occasionally, of joint position sensation. Complex HSP forms are characterized by the presence of additional neurological or non-neurological features. Pure HSP is estimated to affect 9.6 individuals in 100.000. HSP may be inherited as an autosomal dominant, autosomal recessive or X-linked recessive trait, and multiple recessive and dominant forms exist. The majority of reported families (70-80%) displays autosomal dominant inheritance, while the remaining cases follow a recessive mode of transmission. To date, 24 different loci responsible for pure and complex HSP have been mapped. Despite the large and increasing number of HSP loci mapped, only 9 autosomal and 2 X-linked genes have been so far identified, and a clear genetic basis for most forms of HSP remains to be elucidated. -

Ectopic Calcification Around Joints of Paralysed Limbs in Hemiplegia, Diffuse Brain Damage, and Other Neurological Diseases*
Ann Rheum Dis: first published as 10.1136/ard.34.6.499 on 1 December 1975. Downloaded from Ann. rheum. Dis. (1975) 34, 499 Ectopic calcification around joints of paralysed limbs in hemiplegia, diffuse brain damage, and other neurological diseases* ARNOLD J. ROSIN From Harzfeld Hospital, Gedera, Israel Rosin, A. J., (1975). Annals of the Rheumatic Diseases, 34, 499-505. Ectopic calcification around joints ofparalysed limbs in hemiplegia, diffuse brain damage, and other neurological diseases. Mechanical deformity associated, with neurological disease is commonly encountered in the form of contractures, or pre-existing arthritis. Less common is the occurrence of ectopic calcification around the joints of a paralysed limb. Two forms of this are presented in a series of twenty patients. Para-articular calcification with the appearance of myositis ossificans around large joints of the affected limbs occurred most often. The interior of the joints was not affected, nor was there evidence of bony injury. In some cases, however, the excessive outgrowth of bone around the joint eventually copyright. resulted in a functional ankylosis by a uniting bar of bone outside the joint. The second form of calcification was periosteal, which unlike the first type was resorbed and left an area of cortical bony thickening. The twenty patients with para-articular calcification included ten with hemiplegia due to cerebrovascular accidents, two with paraplegia due to trauma, one case of cauda equina syndrome, and seven cases of head injury with periods of unconsciousness ranging from weeks to months. The hip and shoulder joints were most commonly affected, but elbows and knees were sometimes involved.