What You Need to Know
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Supplement Ii to the Japanese Pharmacopoeia Fifteenth Edition
SUPPLEMENT II TO THE JAPANESE PHARMACOPOEIA FIFTEENTH EDITION Official From October 1, 2009 English Version THE MINISTRY OF HEALTH, LABOUR AND WELFARE Notice: This English Version of the Japanese Pharmacopoeia is published for the conven- ience of users unfamiliar with the Japanese language. When and if any discrepancy arises between the Japanese original and its English translation, the former is authentic. The Ministry of Health, Labour and Welfare Ministerial Notification No. 425 Pursuant to Paragraph 1, Article 41 of the Pharmaceutical Affairs Law (Law No. 145, 1960), we hereby revise a part of the Japanese Pharmacopoeia (Ministerial Notification No. 285, 2006) as follows*, and the revised Japanese Pharmacopoeia shall come into ef- fect on October 1, 2009. However, in the case of drugs which are listed in the Japanese Pharmacopoeia (hereinafter referred to as “previous Pharmacopoeia”) [limited to those listed in the Japanese Pharmacopoeia whose standards are changed in accordance with this notification (hereinafter referred to as “new Pharmacopoeia”)] and drugs which have been approved as of October 1, 2009 as prescribed under Paragraph 1, Article 14 of the same law [including drugs the Minister of Health, Labour and Welfare specifies (the Ministry of Health and Welfare Ministerial Notification No. 104, 1994) as those ex- empted from marketing approval pursuant to Paragraph 1, Article 14 of the Pharmaceu- tical Affairs Law (hereinafter referred to as “drugs exempted from approval”)], the Name and Standards established in the previous Pharmacopoeia (limited to part of the Name and Standards for the drugs concerned) may be accepted to conform to the Name and Standards established in the new Pharmacopoeia before and on March 31, 2011. -

(19) United States (12) Patent Application Publication (10) Pub
US 20130289061A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2013/0289061 A1 Bhide et al. (43) Pub. Date: Oct. 31, 2013 (54) METHODS AND COMPOSITIONS TO Publication Classi?cation PREVENT ADDICTION (51) Int. Cl. (71) Applicant: The General Hospital Corporation, A61K 31/485 (2006-01) Boston’ MA (Us) A61K 31/4458 (2006.01) (52) U.S. Cl. (72) Inventors: Pradeep G. Bhide; Peabody, MA (US); CPC """"" " A61K31/485 (201301); ‘4161223011? Jmm‘“ Zhu’ Ansm’ MA. (Us); USPC ......... .. 514/282; 514/317; 514/654; 514/618; Thomas J. Spencer; Carhsle; MA (US); 514/279 Joseph Biederman; Brookline; MA (Us) (57) ABSTRACT Disclosed herein is a method of reducing or preventing the development of aversion to a CNS stimulant in a subject (21) App1_ NO_; 13/924,815 comprising; administering a therapeutic amount of the neu rological stimulant and administering an antagonist of the kappa opioid receptor; to thereby reduce or prevent the devel - . opment of aversion to the CNS stimulant in the subject. Also (22) Flled' Jun‘ 24’ 2013 disclosed is a method of reducing or preventing the develop ment of addiction to a CNS stimulant in a subj ect; comprising; _ _ administering the CNS stimulant and administering a mu Related U‘s‘ Apphcatlon Data opioid receptor antagonist to thereby reduce or prevent the (63) Continuation of application NO 13/389,959, ?led on development of addiction to the CNS stimulant in the subject. Apt 27’ 2012’ ?led as application NO_ PCT/US2010/ Also disclosed are pharmaceutical compositions comprising 045486 on Aug' 13 2010' a central nervous system stimulant and an opioid receptor ’ antagonist. -

Diagnostic Clues in Multiple System Atrophy
DO I:10.4274/Tnd.82905 Case Report / Olgu Sunumu Diagnostic Clues in Multiple System Atrophy: A Case Report and Literature Review Multisistem Atrofi Tanısında İpuçları: Bir Olgu Sunumu ve Literatürün Gözden Geçirilmesi Mehmet Yücel, Oğuzhan Öz, Hakan Akgün, Semai Bek, Tayfun Kaşıkçı, İlter Uysal, Yaşar Kütükçü, Zeki Odabaşı Gülhane Military Medical Academy, Ankara, Turkey Sum mary Multiple system atrophy (MSA) is an adult-onset, sporadic, progressive neurodegenerative disease. Based on the consensus criteria, patients with MSA are clinically classified into cerebellar (MSA-C) and parkinsonian (MSA-P) subtypes. In addition to major diagnostic criteria including poor response to levodopa, and presence of pyramidal or cerebellar signs (ataxia) or autonomic failure, certain clinical features or ‘‘red flags’’ may raise the clinical suspicion for MSA. In our case report we present a 67-year-old female patient admitted to our hospital due to inability to walk, with poor response to levodopa therapy, whose neurological examination revealed severe Parkinsonism, ataxia and who fulfilled all criteria for MSA, as rarely seen in clinical practice.(Turkish Journal of Neurology 2013; 19:28-30) Key Words: Multiple system atrophy, autonomic failure, diagnostic criteria Özet Multisistem atrofi (MSA) erişkin dönemde başlayan, ilerleyici, nedeni bilinmeyen sporadik nörodejeneratif bir hastalıktır. MSA kabul görmüş tanı kriterlerine göre klinik olarak serebellar (MSA-C) ve parkinsoniyen (MSA-P) alt tiplerine ayrılmaktadır. Düşük levadopa yanıtı, piramidal, serebellar bulguların (ataksi) ya da otonomik bozukluk olması gibi majör tanı kriterlerininin yanında “red flags” olarak isimlendirilen belirgin klinik bulgular ya da uyarı işaretlerinin olması MSA tanısı için klinik şüpheyi oluşturmalıdır. Olgu sunumunda 67 yaşında yürüyememe şikayeti ile polikliniğimize müracaat eden ve levadopa tedavisine düşük yanıt gösteren ciddi parkinsonizm bulguları ile ataksi bulunan kadın hasta MSA tanı kriterlerini tam olarak karşıladığı ve klinik pratikte nadir görüldüğü için sunduk. -
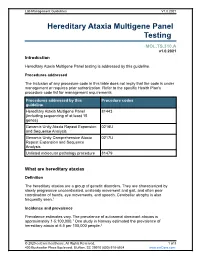
Hereditary Ataxia Multigene Panel Testing
Lab Management Guidelines V1.0.2021 Hereditary Ataxia Multigene Panel Testing MOL.TS.310.A v1.0.2021 Introduction Hereditary Ataxia Multigene Panel testing is addressed by this guideline. Procedures addressed The inclusion of any procedure code in this table does not imply that the code is under management or requires prior authorization. Refer to the specific Health Plan's procedure code list for management requirements. Procedures addressed by this Procedure codes guideline Hereditary Ataxia Multigene Panel 81443 (including sequencing of at least 15 genes) Genomic Unity Ataxia Repeat Expansion 0216U and Sequence Analysis Genomic Unity Comprehensive Ataxia 0217U Repeat Expansion and Sequence Analysis Unlisted molecular pathology procedure 81479 What are hereditary ataxias Definition The hereditary ataxias are a group of genetic disorders. They are characterized by slowly progressive uncoordinated, unsteady movement and gait, and often poor coordination of hands, eye movements, and speech. Cerebellar atrophy is also frequently seen.1 Incidence and prevalence Prevalence estimates vary. The prevalence of autosomal dominant ataxias is approximately 1-5:100,000.1 One study in Norway estimated the prevalence of hereditary ataxia at 6.5 per 100,000 people.2 © 2020 eviCore healthcare. All Rights Reserved. 1 of 8 400 Buckwalter Place Boulevard, Bluffton, SC 29910 (800) 918-8924 www.eviCore.com Lab Management Guidelines V1.0.2021 Symptoms Although hereditary ataxias are made up of multiple different conditions, they are characterized by slowly progressive uncoordinated, unsteady movement and gait, and often poor coordination of hands, eye movements, and speech. Cerebellar atrophy is also frequently seen.1 Cause Hereditary ataxias are caused by mutations in one of numerous genes. -

(12) United States Patent (10) Patent No.: US 6,319,953 B1 Carlson Et Al
US006319953B1 (12) United States Patent (10) Patent No.: US 6,319,953 B1 Carlson et al. (45) Date of Patent: *Nov. 20, 2001 (54) TREATMENT OF DEPRESSION AND WO 95/08549 3/1995 (W0). ANXIETY WITH FLUOXETINE AND AN WO 95/18124 7/1995 (W0). NK-1 RECEPTOR ANTAGONIST W0 96/05181 2/1996 (W0). W0 96/18643 6/1996 (W0). (75) Inventors: Emma Joanne Carlson, Puckeridge; W0 96/19233 6/1996 (W0). Nadia Melanie Rupniak, Bishops W0 96/24353 8/1996 (W0). W0 98/15277 4/1998 (W0). Stortford, both of (GB) OTHER PUBLICATIONS (73) Assignee: Merck Sharp & Dohme Ltd., Hoddesdon (GB) Aguiar, M., et al., Physiology& Behavior, 1996, 60(4) 1183—1186. ( * ) Notice: Subject to any disclaimer, the term of this Barden, N., et al., J. Neurochem., 1983, 41, 834—840. patent is extended or adjusted under 35 BristoW, L., et al., Eur J. Pharmacol., 1994, 253, 245—252. U.S.C. 154(b) by 0 days. Brodin, E., et al., Neuropharmacology, 1987, 26(6) 581—590. This patent is subject to a terminal dis Brodin, E., et al., Neuropeptides, 1994, 26, 253—260. claimer. Culman, J., et al., J. Physiol. Pharmacol., 1995, 73, 885—891. Cutler, et al., J. Psychopharmacol, 1994, 8, A22, 87. (21) Appl. N0.: 09/457,241 Elliott, P. J., Exp. Brain Res. UK, 1988, 73, 354—356. (22) Filed: Dec. 8, 1999 F—D—C Reports—Prescription Pharmaceuticals and Bio technology, Dec. 8, 1997, 59(49), 10. Related US. Application Data File, S. E., Pharm. Biochem. Behavior, 1997, 58, 3, 747—752. (60) Division of application No. -
Multiple System Atrophy
Multiple System Atrophy U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES Public Health Service National Institutes of Health Multiple System Atrophy What is multiple system atrophy? ultiple system atrophy (MSA) is M a progressive neurodegenerative disorder characterized by a combination of symptoms that affect both the autonomic nervous system (the part of the nervous system that controls involuntary action such as blood pressure or digestion) and move- ment. The symptoms reflect the progressive loss of function and death of different types of nerve cells in the brain and spinal cord. Symptoms of autonomic failure that may be seen in MSA include fainting spells and prob- lems with heart rate, erectile dysfunction, and bladder control. Motor impairments (loss of or limited muscle control or movement, or limited mobility) may include tremor, rigidity, and/or loss of muscle coordination as well as difficulties with speech and gait (the way a person walks). Some of these features are similar to those seen in Parkinson’s disease, and early in the disease course it often may be difficult to distinguish these disorders. MSA is a rare disease, affecting potentially 15,000 to 50,000 Americans, including men and women and all racial groups. Symptoms tend to appear in a person’s 50s and advance rapidly over the course of 5 to 10 years, with progressive loss of motor function and 1 eventual confinement to bed. People with MSA often develop pneumonia in the later stages of the disease and may suddenly die from cardiac or respiratory issues. While some of the symptoms of MSA can be treated with medications, currently there are no drugs that are able to slow disease progression and there is no cure. -

CAS Number Index
2334 CAS Number Index CAS # Page Name CAS # Page Name CAS # Page Name 50-00-0 905 Formaldehyde 56-81-5 967 Glycerol 61-90-5 1135 Leucine 50-02-2 596 Dexamethasone 56-85-9 963 Glutamine 62-44-2 1640 Phenacetin 50-06-6 1654 Phenobarbital 57-00-1 514 Creatine 62-46-4 1166 α-Lipoic acid 50-11-3 1288 Metharbital 57-22-7 2229 Vincristine 62-53-3 131 Aniline 50-12-4 1245 Mephenytoin 57-24-9 1950 Strychnine 62-73-7 626 Dichlorvos 50-23-7 1017 Hydrocortisone 57-27-2 1428 Morphine 63-05-8 127 Androstenedione 50-24-8 1739 Prednisolone 57-41-0 1672 Phenytoin 63-25-2 335 Carbaryl 50-29-3 569 DDT 57-42-1 1239 Meperidine 63-75-2 142 Arecoline 50-33-9 1666 Phenylbutazone 57-43-2 108 Amobarbital 64-04-0 1648 Phenethylamine 50-34-0 1770 Propantheline bromide 57-44-3 191 Barbital 64-13-1 1308 p-Methoxyamphetamine 50-35-1 2054 Thalidomide 57-47-6 1683 Physostigmine 64-17-5 784 Ethanol 50-36-2 497 Cocaine 57-53-4 1249 Meprobamate 64-18-6 909 Formic acid 50-37-3 1197 Lysergic acid diethylamide 57-55-6 1782 Propylene glycol 64-77-7 2104 Tolbutamide 50-44-2 1253 6-Mercaptopurine 57-66-9 1751 Probenecid 64-86-8 506 Colchicine 50-47-5 589 Desipramine 57-74-9 398 Chlordane 65-23-6 1802 Pyridoxine 50-48-6 103 Amitriptyline 57-92-1 1947 Streptomycin 65-29-2 931 Gallamine 50-49-7 1053 Imipramine 57-94-3 2179 Tubocurarine chloride 65-45-2 1888 Salicylamide 50-52-2 2071 Thioridazine 57-96-5 1966 Sulfinpyrazone 65-49-6 98 p-Aminosalicylic acid 50-53-3 426 Chlorpromazine 58-00-4 138 Apomorphine 66-76-2 632 Dicumarol 50-55-5 1841 Reserpine 58-05-9 1136 Leucovorin 66-79-5 -

Transdermal Drug Delivery Device Including An
(19) TZZ_ZZ¥¥_T (11) EP 1 807 033 B1 (12) EUROPEAN PATENT SPECIFICATION (45) Date of publication and mention (51) Int Cl.: of the grant of the patent: A61F 13/02 (2006.01) A61L 15/16 (2006.01) 20.07.2016 Bulletin 2016/29 (86) International application number: (21) Application number: 05815555.7 PCT/US2005/035806 (22) Date of filing: 07.10.2005 (87) International publication number: WO 2006/044206 (27.04.2006 Gazette 2006/17) (54) TRANSDERMAL DRUG DELIVERY DEVICE INCLUDING AN OCCLUSIVE BACKING VORRICHTUNG ZUR TRANSDERMALEN VERABREICHUNG VON ARZNEIMITTELN EINSCHLIESSLICH EINER VERSTOPFUNGSSICHERUNG DISPOSITIF D’ADMINISTRATION TRANSDERMIQUE DE MEDICAMENTS AVEC COUCHE SUPPORT OCCLUSIVE (84) Designated Contracting States: • MANTELLE, Juan AT BE BG CH CY CZ DE DK EE ES FI FR GB GR Miami, FL 33186 (US) HU IE IS IT LI LT LU LV MC NL PL PT RO SE SI • NGUYEN, Viet SK TR Miami, FL 33176 (US) (30) Priority: 08.10.2004 US 616861 P (74) Representative: Awapatent AB P.O. Box 5117 (43) Date of publication of application: 200 71 Malmö (SE) 18.07.2007 Bulletin 2007/29 (56) References cited: (73) Proprietor: NOVEN PHARMACEUTICALS, INC. WO-A-02/36103 WO-A-97/23205 Miami, FL 33186 (US) WO-A-2005/046600 WO-A-2006/028863 US-A- 4 994 278 US-A- 4 994 278 (72) Inventors: US-A- 5 246 705 US-A- 5 474 783 • KANIOS, David US-A- 5 474 783 US-A1- 2001 051 180 Miami, FL 33196 (US) US-A1- 2002 128 345 US-A1- 2006 034 905 Note: Within nine months of the publication of the mention of the grant of the European patent in the European Patent Bulletin, any person may give notice to the European Patent Office of opposition to that patent, in accordance with the Implementing Regulations. -

(12) Patent Application Publication (10) Pub. No.: US 2015/0202317 A1 Rau Et Al
US 20150202317A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2015/0202317 A1 Rau et al. (43) Pub. Date: Jul. 23, 2015 (54) DIPEPTDE-BASED PRODRUG LINKERS Publication Classification FOR ALPHATIC AMNE-CONTAINING DRUGS (51) Int. Cl. A647/48 (2006.01) (71) Applicant: Ascendis Pharma A/S, Hellerup (DK) A638/26 (2006.01) A6M5/9 (2006.01) (72) Inventors: Harald Rau, Heidelberg (DE); Torben A 6LX3/553 (2006.01) Le?mann, Neustadt an der Weinstrasse (52) U.S. Cl. (DE) CPC ......... A61K 47/48338 (2013.01); A61 K3I/553 (2013.01); A61 K38/26 (2013.01); A61 K (21) Appl. No.: 14/674,928 47/48215 (2013.01); A61M 5/19 (2013.01) (22) Filed: Mar. 31, 2015 (57) ABSTRACT The present invention relates to a prodrug or a pharmaceuti Related U.S. Application Data cally acceptable salt thereof, comprising a drug linker conju (63) Continuation of application No. 13/574,092, filed on gate D-L, wherein D being a biologically active moiety con Oct. 15, 2012, filed as application No. PCT/EP2011/ taining an aliphatic amine group is conjugated to one or more 050821 on Jan. 21, 2011. polymeric carriers via dipeptide-containing linkers L. Such carrier-linked prodrugs achieve drug releases with therapeu (30) Foreign Application Priority Data tically useful half-lives. The invention also relates to pharma ceutical compositions comprising said prodrugs and their use Jan. 22, 2010 (EP) ................................ 10 151564.1 as medicaments. US 2015/0202317 A1 Jul. 23, 2015 DIPEPTDE-BASED PRODRUG LINKERS 0007 Alternatively, the drugs may be conjugated to a car FOR ALPHATIC AMNE-CONTAINING rier through permanent covalent bonds. -

Lewy Body Diseases and Multiple System Atrophy As ␣-Synucleinopathies
Molecular Psychiatry (1998) 3, 462–465 1998 Stockton Press All rights reserved 1359–4184/98 $12.00 GUEST EDITORIAL Lewy body diseases and multiple system atrophy as ␣-synucleinopathies Parkinson’s disease and dementia with Lewy bodies synuclein are the first known genetic causes of Parkin- are among the most common neurodegenerative dis- son’s disease. They are located in the amino-terminal eases. They share the Lewy body and the Lewy neurite half of ␣-synuclein, which consists of seven imperfect as their defining neuropathological characteristics. repeats of 11 amino acids each, with the consensus Originally described in 1912 as a light-microscopic sequence KTKEGV (Figure 1). It has been suggested entity, the Lewy body was shown to be made of abnor- that ␣-synuclein may bind through these repeats to mal filaments in the 1960s. Over the past year, the bio- membranes rich in acidic phospholipids.3 chemical nature of the Lewy body filament has been This work raised the question whether ␣-synuclein revealed. is a component of Lewy bodies and Lewy neurites of A large number of different proteins has been idiopathic Parkinson’s disease and of dementia with reported to be present in Lewy bodies and Lewy neur- Lewy bodies. Using well-characterised anti-␣-synuc- ites by immunohistochemical methods. However, these lein antibodies, Spillantini et al showed strong staining findings do not permit us to distinguish between of both Lewy bodies and Lewy neurites in idiopathic intrinsic Lewy body components and normal cellular Parkinson’s disease and dementia with Lewy bodies.4 constituents that get merely trapped in the filaments They also reported the lack of staining of these patho- that make up the Lewy body. -

Droxidopa (NORTHERA) Drug Monograph
Droxidopa Drug Monograph Droxidopa (NORTHERA™) National Drug Monograph December 2014 VA Pharmacy Benefits Management Services, Medical Advisory Panel, and VISN Pharmacist Executives The purpose of VA PBM Services drug monographs is to provide a comprehensive drug review for making formulary decisions. Updates will be made when new clinical data warrant additional formulary discussion. Documents will be placed in the Archive section when the information is deemed to be no longer current. FDA Approval Information1 Description/Mechanism of Droxidopa is a synthetic amino acid analog that is metabolized by dopa- Action decarboxylase to norepinephrine. Norepinephrine increases blood pressure through peripheral arterial and venous vasoconstriction. Indication(s) Under Review in Droxidopa is indicated for the treatment of orthostatic dizziness, this document lightheadedness, or the “feeling that you are about to black out” in adult patients with symptomatic neurogenic orthostatic hypotension (NOH) caused by primary autonomic failure (Parkinson's disease, multiple system atrophy, and pure autonomic failure), dopamine beta-hydroxylase deficiency, and nondiabetic autonomic neuropathy. Effectiveness beyond 2 weeks of treatment has not been demonstrated. The continued effectiveness of droxidopa should be assessed periodically.1 Dosage Form(s) Under Droxidopa is available as 100 mg, 200 mg, 300 mg hard gelatin capsules. Review REMS REMS No REMS See Other Considerations for additional REMS information Pregnancy Rating Droxidopa is Pregnancy Category -
![Nouriast Tablets 20 Mg [Non-Proprietary Name] Istradefylline (JAN*) [Applicant] Kyowa Hakko Kirin Co., Ltd](https://docslib.b-cdn.net/cover/7814/nouriast-tablets-20-mg-non-proprietary-name-istradefylline-jan-applicant-kyowa-hakko-kirin-co-ltd-1557814.webp)
Nouriast Tablets 20 Mg [Non-Proprietary Name] Istradefylline (JAN*) [Applicant] Kyowa Hakko Kirin Co., Ltd
Report on the Deliberation Results March 15, 2013 Evaluation and Licensing Division, Pharmaceutical and Food Safety Bureau Ministry of Health, Labour and Welfare [Brand name] Nouriast Tablets 20 mg [Non-proprietary name] Istradefylline (JAN*) [Applicant] Kyowa Hakko Kirin Co., Ltd. [Date of application] March 30, 2012 [Results of deliberation] In the meeting held on March 8, 2013, the First Committee on New Drugs concluded that the product may be approved and that this result should be reported to the Pharmaceutical Affairs Department of the Pharmaceutical Affairs and Food Sanitation Council. The product is not classified as a biological product or a specified biological product, the re-examination period is 8 years, and neither the drug substance nor the drug product is classified as a poisonous drug or a powerful drug. *Japanese Accepted Name (modified INN) This English version of the Japanese review report is intended to be a reference material to provide convenience for users. In the event of inconsistency between the Japanese original and this English translation, the former shall prevail. The PMDA will not be responsible for any consequence resulting from the use of this English version. Review Report February 22, 2013 Pharmaceuticals and Medical Devices Agency The results of a regulatory review conducted by the Pharmaceuticals and Medical Devices Agency on the following pharmaceutical product submitted for registration are as follows. [Brand name] Nouriast Tablets 20 mg [Non-proprietary name] Istradefylline [Name of applicant]