Hochu-Ekki-To Improves Motor Function in an Amyotrophic Lateral Sclerosis Animal Model
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Stinging Nettle
Top Three Herbs for Your Health Top Three Herbs for Your Health Text and photos by Rosalee de la Forêt. ©2015 Rosalee de la Foret, LLC. All rights reserved. No part of this publication may be reproduced in whole or in part, or stored in a retrieval system, or transmitted in any form or by any means, electronic, mechanical, photocopying, recording, or otherwise, without written permission of the author. The herbal and plant information in this eBook is for educational purposes only. The information within the Top Three Herbs for Your Health eBook is not intended as a substitute for the advice provided by your physician or other medical professional. If you have or suspect that you have a serious health problem, promptly contact your health care provider. Always consult with a health care practitioner before using any herbal remedy or food, especially if pregnant, nursing, or have a medical condition. This ebook contains affiliate links. Using these links to make herb purchases supports the free information in this ebook. Thank you! Published by Rosalee de la Forêt, LLC, Twisp, WA First digital edition, January 2015. Published in the U.S.A. 2 Top Three Herbs for Your Health Table of Contents Top Three Reasons to Use Herbs............................................................................................4 Stinging Nettle.............................................................................................................................6 Nourishing Herbal Infusion Recipe........................................................................9 -

Who's Got What
WHO’S GOT WHAT JAKE FRATKIN’S COMPREHENSIVE INDEX OF CHINESE HERBAL PRODUCTS IN AMERICA Available GMP Products from United States, China and Taiwan Version 1.7 © 2016 For free download of Who’s Got What, go to: www.drjakefratkin.com/whos-got-what Jake Paul Fratkin, OMD, L.Ac. www.drjakefratkin.com Author, ESSENTIAL CHINESE FORMULAS (2014) CHINESE HERBAL PATENT MEDICINES, The Clinical Desk Reference (2001) For Table of Contents of Essential Chinese Formulas, go to: http://drjakefratkin.com/essential-formulas-index TABLE OF CONTENTS, BY GROUP 1. PATHOGENIC WIND DISORDERS p. 7 2. FORMULAS THAT CLEAR HEAT 13 3. RESPIRATORY DISORDERS 19 4. BI SYNDROME (Arthritis, Rheumatism, Back Pain) 27 5. TRAUMA AND PAIN 34 6. DIGESTIVE DISORDERS 38 7. LIVER AND GALLBLADDER DISORDERS 51 8. GYNECOLOGICAL DISORDERS 62 9. DISTURBED SHEN (Insomnia, Anxiety, Palpitation) 72 10. HEART BLOOD STASIS AND HEART PHLEGM 75 11. UROGENITAL DISORDERS 77 12. WATER RETENTION AND EDEMA 80 13. DERMATOLOGICAL DISORDERS 82 14. EYE AND VISION DISORDERS 86 2 15. MISCELLANEOUS DISORDERS 87 16. QI AND BLOOD TONICS 89 17. KIDNEY TONICS 95 18. COMBINATION AND SINGLE HERB TONICS 101 How to Use this Index 105 Code Letters of Herbal Companies 106 TABLE OF CONTENTS 1. EXOGENOUS WIND DISORDERS p. 7 1A. Exogenous Wind-Cold 7 1A1. Pathogenic Wind-Cold (Common Cold - Cold Type) 7 1A2. Pathogenic Wind-Cold Into Shaoyang 9 1B. Pathogenic Wind-Heat (Common Cold – Mild Heat Type) 9 1C. Nasal and Ear Congestion 10 1C1. Nasal Congestion 10 1C2. Ear Infection 12 2. FORMULAS THAT CLEAR HEAT 13 2A. -

Stopping Relapsing Lyme Disease Pain, Fatigue, & Mental Fog With
Beyond Wack-A-Mole Lyme Treatment What Has Helped People to Heal Lyme MCIDs Concurrent with or Post Drug Therapy Integrative Lyme Solutions Conference Dallas, Texas June 21-22, 2013 Two Frogs Healing Center 170 West Patrick Street, Frederick, MD 21701 301.228.3764 www.GoodbyeLyme.com [email protected] Greg Lee, M. Ac Disclosure statement • No grants • No industry funding from drug, herb, medical device suppliers • Not a paid consultant • Not on any committees, board of directors, advisory panels, review boards • Just me and my two frogs Background • Technologist: Software engineer in NASA Robotics Lab, Hubble Space Telescope, spacecraft integration and testing, climate modeling projects • Leadership: Managing partner at LionHeart Consulting • Medical: Masters Degree of Acupuncture and Chinese herbal certification • Master Sufi Healer The Question • Why do some people heal Lyme disease and their multiple chronic infections and others do not? Objectives • Overview of GoodbyeLyme system – Treatment challenges in Lyme / Multiple Chronic Infectious Disease patients – Natural medicines, strategies, and treatments for overcoming treatment challenges • Case studies • More questions Patient Challenges • Patients are highly toxic from antibiotic tx, environment & childhood exposure to toxins, lifestyle, dental procedures, compromised detox pathways • Multiple infections (TBDs, parasites, secondary infx, fungi, viral) Patient Challenges (cont’d) • Infections hide in reservoirs: biofilms, cartilage, collagen, skin, nervous system, inside -
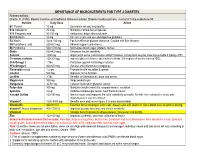
IMPORTANCE of MICRONUTRIENTS for TYPE 2 DIABETES Referenced From: Choate, C
IMPORTANCE OF MICRONUTRIENTS FOR TYPE 2 DIABETES Referenced from: Choate, C. (1998). Modern medicine and traditional Chinese medicine: Diabetes mellitus part one. Journal of Chinese Medicine 58. Nutrient Daily Dose Action B1 Thiamin 10 mg Decreases sensory neuropathy B12 Cobalamin 25 mcg Maintains normal nerve impulses B15 Pangamic acid 50-100 mg Antioxidant, helps atherosclerosis B2 Riboflavin 10 mg For skin ulcers and eye and digestive problems B3 Niacin Up to 100 mg Positive effect on glucose tolerance. Caution with liver disease B5 Pantothenic acid 250-500 mg Adrenal support (anti-stress) B6 Pyridoxine 500-1000 mg Normalizes blood sugar, protects nerves Biotin 200-400 mcg Enhances insulin sensitivity Calcium 1000 mg Important in nerve transmission and pH balance. Citrate form may be more bioavailable if taking a PPI Chromium picolinate 150-200 mg Improves glucose tolerance and insulin sensitivity. 500 mcg bid x 4 months lowered FBGL EFA-Omega 3 1 Tbs Protection against hardening of arteries EFA-Omega 6 400-600 mg General anti-inflammatory properties Flavonoids mixed 1-2 gm Promote insulin secretion & uptake Inositol 500 mg Improves nerve function Lecithin 3 Tbs Benefits cell membranes, brain and nerves Magnesium 500 mg Helps protect eyes Manganese 30-50 mg Cofactor involved in glycemic control Potassium 300 mg Maintains insulin sensitivity, responsiveness, secretion Spirulina 3-6 gr Stabilizes blood sugar levels. Cold thermal nature! Vanadyl Sulfate 100-150 mg Mimics insulin and improves the cells’ sensitivity to insulin. Benefits often extended for weeks after Supplementation was discontinued Vitamin C 1000-4000 mg Benefits eyes and nerves [lipoic C is more bioavailable] Vitamin D3 400-800 IU Essential for functioning of islets cells. -

The Use of Chinese Yang/ Qi-Invigorating Tonic Botanical Drugs/ Herbal Formulations in Ameliorating Chronic Kidney Disease by Enhancing Mitochondrial Function
REVIEW published: 24 June 2021 doi: 10.3389/fphar.2021.622498 The Use of Chinese Yang/ Qi-Invigorating Tonic Botanical Drugs/ Herbal Formulations in Ameliorating Chronic Kidney Disease by Enhancing Mitochondrial Function Jiayi Tian 1,2†, Yuqi Huang 1,2†, Tong Wu 1,2, Hsien-Da Huang 2,3, Kam Ming Ko 4*, Bao Ting Zhu 1,2* and Jihang Chen 1,2* 1Shenzhen Key Laboratory of Steroid Drug Discovery and Development, School of Life and Health Sciences, The Chinese University of Hong Kong, Shenzhen, China, 2School of Life and Health Sciences, The Chinese University of Hong Kong, Edited by: Shenzhen, China, 3Warshel Institute for Computational Biology, The Chinese University of Hong Kong, Shenzhen, China, 4Division Uraiwan Panich, of Life Science, The Hong Kong University of Science & Technology, Hong Kong, China Mahidol University, Thailand Reviewed by: Mingjiang Yao, Background: Chronic kidney disease (CKD) is a leading cause of morbidity and mortality. Xiyuan Hospital, China Mitochondrial dysfunction has been implicated as a key factor in the development of CKD. Rodrigo Castaneda, According to traditional Chinese medicine (TCM) theory, many Chinese Yang/Qi- Universidad de San Carlos de Guatemala, Guatemala invigorating botanical drugs/herbal formulations have been shown to produce *Correspondence: promising outcomes in the clinical management of CKD. Experimental studies have Jihang Chen indicated that the health-promoting action of Yang/Qi invigoration in TCM is related to [email protected] Bao Ting Zhu the up-regulation of mitochondrial energy generation and antioxidant status. [email protected] Kam Ming Ko Objective: In this review, we aim to test whether Chinese Yang/Qi-invigorating tonic [email protected] botanical drugs/herbal formulations can provide medical benefits in CKD and its †These authors have contributed complications. -
Who's Got What-1.4
Dr. Jake Paul Fratkin OMD, L.A c. Who's Got What Jake Fratkin's Comprehensive Index of Chinese Herbal Products in America Available GMP Products from United States, China and Taiwan WHO’S GOT WHAT JAKE FRATKIN’S COMPREHENSIVE INDEX OF CHINESE HERBAL PRODUCTS IN AMERICA Available GMP Products from United States, China and Taiwan Jake Paul Fratkin, OMD, L.Ac. Version 1.4 © 2012 PLEASE DO NOT SHARE THIS PDF. DOWNLOAD PURCHASES CAN BE MADE AT: www.drjakefratkin.com/products/whos-got-what TABLE OF CONTENTS Detailed Table of Contents Follows on page 2 1. PATHOGENIC WIND DISORDERS 7 2. HEAT DISORDERS 13 3. LUNG DISORDERS 17 4. MUSCULOSKELETAL DISORDERS 24 5. DIGESTIVE DISORDERS 32 6. GYNECOLOGICAL DISORDERS 42 7. LIVER DISORDERS 49 8. HEART AND SHEN DISORDERS 57 9. UROGENITAL DISORDERS 62 10. SKIN DISORDERS 65 11. EYE AND VISION DISORDERS 68 12. TONICS 69 How to Use this Index 80 Code Letters of Herbal Companies 81 2 TABLE OF CONTENTS 1. PATHOGENIC WIND DISORDERS 1A. Wind-Cold 1A1. Pathogenic Wind-Cold (Common Cold - Cold Type) 7 1A2. Pathogenic Wind-Cold Into Shaoyang 8 1B. Wind-Heat 1B1. Pathogenic Wind-Heat (Early Cold-Flu) 9 1B2. Pathogenic Wind with Heat-Toxins (Severe Cold-Flu) 10 1C. Nasal and Ear Congestion 1C1. Nasal Congestion 11 1C2. Ear Infection 12 2. HEAT DISORDERS 2A. Heat Toxins (Viral Infections) 13 2B. Damp-Heat Toxins (Bacterial Infections) 14 2C. Fever 15 2D. Stomach Fire 16 3. LUNG DISORDERS 3A. Lung Heat and Fire (Painful Barking Cough) 17 3B. Lung Phlegm-Heat (Acute Productive Cough) 17 3C. -

Development and Hygiene of Functional Foods with Immunomodulation Activity Using Radiation
KR0000086 KAERI/RR-1912/98 Development of Food Science and Technology by Radiation Development and Hygiene of Functional Foods with Immunomodulation Activity Using Radiation 7] 3Z|- 71 31/ 30 KAERI/RR-1912/98 Development of Food Science and Technology by Radiation Development and Hygiene of Functional Foods with Immunomodulation Activity Using Radiation 7] 7l 1999. 4. •ftl.J3.Sl C3 TT =?• SI ^ "a 'o 2. ?i o| ^ € °J =? 0| ii. Aj-s] jfe n £ 71 ^ III - i - 2. 3. Apoptosis Apoptosis 4. cells)^ wfl^ 2-cI - ii - <£#%• ^(Nitric Oxide) 5.7]^^ ^#db7jK^^^)^j 7jv\# *]•%• 1-^ 2:A} ^j 2:A} 4^^ -a-Sl^^- ^^^4 HPLCS. Paeoniflorin<>l 1-^^°]€A^ £-°)z\ #•%••£ Ames test°lM ^^ . Paeoniflorin^l ^^- CHO DPPHi IV. -i°fl4 SRBCi : 10 : 10 2. - IV - Apoptosis ^. apoptosis €3*5= Apoptosis apoptosis - v - 3. marrow stem cells)^1 f^ £(stromal cells) ^ ^aj-g-o] nfl-f ^A^JL ^ZJ-SIJI 5^4. 87M 50% - vi - ^, 37H -2-S.fe NO ^A^ - , ^3^.S NO ^S^^: -^-S^l-^Jl, iNOS ^*MS1 NGMMi IL-liff, IL-6, LT, iNOS^) mRNA 4. 7l^>g ^ , SIS. ^ ^^-^1^-, 1^t^S M-^f^ £4^ ^4, 10 KGy 54 paeoniflorin^- £e|, ^^I*>^ HPLC^ 97%^ 13C-NMR AT*! paeoniflorin^ retention timeo] 7.915, - VI! ~ 1 44 ^#5] $4. lOkGy 24 4^4 paeoniflorin ^ ^^^ 14 2.59%4 2.42%7> chromatogram^ pattern0!]^H 1141- -<?l decursin4 decursin angelatefe SiO2 column chromatographyS. ^-^«>^l*.H, HPLC* ^f-Sfl ^ signal-i- E-$*1^ ylJI^H 3- ^2:1- ^^^-^i 1:51 tb ^^-S ^"^^^ ^^l- column (Shim-pack CLC-ODS(M))*fH #^r ^-el^-i- i-^^^A^, normal phase column^ 4fe Hexane: EtOAc -§-*1l7lHH ^^tb ^-^^^r ^.^ ^r&4- 4D}^i 2: 4(10kGy) ^^^ «12:4 ^^^ -frjL^^- ^^=^4fe decursin^l decursinol angelate^ Salmonella typhimurium TA98, TA100, TA102 ^^^ 4^1"^^oll- °l-§- Sj-fe Ames testi4 444(10 KGy) ^S^l CHO KGy) - Paeoniflorin^ #^^°l€^^r S-°14 &-§-# Ames tesH4 paeoniflorin-i- ^^fF ^4, 4 Paeoniflorino] CHO 24 4^H ^-s!€ paeoniflorin $7} 444, - viii - x\g,«\ benzo(a)pyrene-°-S. -
Kan Herbals Formula Guide
FORMULA GUIDE Chinese Herbal Products You Can Trust Kan Herbals – Formulas by Ted Kaptchuk, O.M.D. Written and researched by Ted J. Kaptchuk, O.M.D.; Z’ev Rosenberg, L.Ac. Copyright © 1992 by Sanders Enterprises with revisions of text and formatting by Kan Herb Company. Copyright © 1996 by Andrew Miller with revisions of text and formatting by Kan Herb Company. Copyright © 2008 by Lise Groleau with revisions of text and formatting by Kan Herb Company. All rights reserved. No part of this written material may be reproduced or stored in any retrieval system, by any means – photocopy, electronic, mechanical or otherwise – for use other than “fair use,” without written consent from the publisher. Published by Golden Mirror Press, California. Printed in the United States of America. First Edition, June 1986 Revised Edition, October 1988 Revised Edition, May 1992 Revised Edition, November 1994 Revised Edition, April 1996 Revised Edition, January 1997 Revised Edition, April 1997 Revised Edition, July 1998 Revised Edition, June 1999 Revised Edition, June 2002 Revised Edition, July 2008 Revised Edition, February 2014 Revised Edition, January 2016 FORMULA GUIDE 25 Classical Chinese Herbal Formulas Adapted by Ted Kaptchuk, OMD, LAc Contents Product Information.....................................................................................................................................1 Certificate of Analysis Sample .................................................................................................................6 High Performance -

Treating Irritable Bowel Syndrome with Chinese Herbs by Jake Schmalzriedt, DOM
TREATING IRRITABLE BOWEL SYNDROME WITH CHINESE HERBS By Jake Schmalzriedt, DOM Irritable Bowel syndrome (IBS) is a chronic functional bowel The enteric nervous system, specifically a neurotransmitter disorder that mainly affects the large intestine (colon). It is imbalance, may play a role in IBS. Neurotransmitters—spe- characterized by abdominal pain, bloating, and distention cifically serotonin—are associated with intestinal secretion, with a change in frequency and/or consistency of stool recur- sensory function, motor function, and sensitivity to pain. It is rent over months or years. thought that increased serotonin levels in the intestinal tract IBS is also known as spastic colon, functional bowel disease, cause an increase in peristalsis. Serotonin also plays a role and, commonly, “nervous stomach.” Spastic colon implies in mood disorders such as stress, anxiety, and depression— an increase in muscle contractions and is not the most ac- making the connection between mood disorders and IBS, and curate term, as IBS is associated with both an increase and a explaining why antidepressant drugs are often prescribed. decrease of motility. IBS is also known by spastic colitis and Another factor that may play a role in IBS is an increase or mucus colitis; however, these terms tend to be problematic, overgrowth of bacteria in the small intestine, often due to a as they imply substantial inflammation of the colon, which is bacterial migration from the large intestine, causing excessive not the case with IBS. gas, bloating, and diarrhea. This is why probiotics and antibi- otics can help with the signs and symptoms of IBS. Increases IBS has only been recognized by Western medicine during in the volume of mast cells are found in patients with IBS,ii the past half century, though the signs and symptoms of the which may attribute to a low-grade inflammatory response. -
Herbal Formulas 32
2017 NCCAOM® Examination Study Guide for the Diplomate of Chinese Herbology Certification NCCAOM® 76 S. Laura Street • Suite 1290 Jacksonville, FL 32202 Phone 904.598.1005 • Fax 904.598.5001 © 2017 NCCAOM® Table of Contents THE EXAMINATION PROCESS Introduction 2 Examination Development 3 Examination Content Validation 3 The NCCAOM® Job Analysis 3 Item Writing 4 Item Review 4 Examination Administration 5 2017 EXPANDED CONTENT OUTLINES Foundations of Oriental Medicine Content Outline 6 Biomedicine Content Outline 15 -Appendix A: Pharmaceuticals 21 -Appendix B: Nutrients and Supplements 22 -Appendix C: Clinical Conditions 23 Chinese Herbology Content Outline 27 -Appendix of Chinese Herbal Formulas 32 B I B L I O G R A P H I E S Foundations of Oriental Medicine Bibliography 38 Biomedicine Bibliography 40 Chinese Herbology Bibliography 41 R E F E R E N C E M A T E R I A L Examination Nomenclature Cross-Reference 43 S A M P L E Q U E S T I O N S Sample Questions for Each Examination Module 45 F R E Q U E N T L Y A S K E D Q U E S T I O N S Frequently Asked Examination Questions 48 Revised: 03/28/2017 1 Chinese Herbology Study Guide Introduction This study guide is designed to help prepare candidates for the NCCAOM certification examinations. Passage of the NCCAOM certification examinations is one of the requirements to become a Diplomate of Chinese Herbology (NCCAOM) and demonstrates the core knowledge, skills and abilities expected for an entry level practitioner of Chinese Herbology. -

Development of Functional Foods for Radiation Workers
KR0000208 KAERI/RR-2028/99 Development of Radiation Food and Biotechnology Development of Functional Foods for Radiation Workers 7} Please be aware that all of tbe Missing Pages in this document were originally blank pages 2000. 3. 31. <=> 04 bH TT CD td H| 5|| ^ W ^ -Ml o| ^ o| AH ?=f o ot i. WR ^5]^, glucan ^ interleukin-1, GM-CSF f- -77]- ^ ^l A} 1 III. si (1) ].§- 7f^ A (2) 7fl^ol 5:4 ^^ (2) cells)^ (Nitric oxide) ^ ^ Afl 24 4|i^i Apoptosis (1) 71 AJIS. « 2:1 7]^ ^ (2) j: -fi--fi-33: (3) 2. - in - 2:4 2:4 2:4 ^] paeoniflorin ^5^ f-^ :4 4^AS^fEi ^s]^ paeoniflorin^ - Paeoniflorino| #^^°]^-^# iL^l^l ^^g-1- Ames test°114 ^^ - Paeoniflorin<>1 i^^1^^* iL°l^l S^^-# ^^ decursin 4 decursin angelate-^ -§-s] -§-^§ HPLC ^^ a?i Ad^ 3-A]- ^-^^ -H-M^-^l decursin^l- decursinol angelate^ HPLC iv. 1-1. 71". (1) 44)° - iv - (2) ^IS^l 107H1: 6 (3) 71^ (4) >«^1^ ^^ ^^1 14 ^^ 4-f^i^ SRBCi (1) ^^ ^^^^(stromal cells)^ «!)<£ #^^>^lS(bone marrow stem cells)^ 4£(stromal cells)^-S] - v - (2) 5f7]^ ^ ^|#db^| 1, 87M ^-*1^ ^ 50% ^££ ^ (3) td^Aflio] ^xj-^. ^^(Nitric oxide) S^r NO ^^]# ^-£^^1 ^^Hi^l1?}, IFN-rl- S- NO ^^1- -fr^^^i, iNOS ^l^ NGMMi IL-6, LT, iNOS^ mRNA XI X) apoptosis - vi - (l) (2) ^44 24 4^^6ll4 fl^^ sl^ls ^^ ^7} ^j1) o] (3) i^-g- Afl3£^l Apoptosis apoptgsis 1-2. 7}. (1) ^(herb mixture, HM) (2) 2(HM-II) vii - (3) (7\) HM-I (4) (7\) 47}x] I^r 5.5^11, (4) i^-S- >fli^ Apoptosis ^-^r ^^1 HM-I, HM-H ^ HM-IV^^ s^]^o_^ ^ojA^o|i, apOptosis apoptosis ^1 - vin - HM-I, HM-n ^ ^ 4*1 HM-IMH 2(HM-n)# 44 TTS 3:^-^1-i-(herbal immunomodulator mixture) HIM-I , HM-nS. -

Efficacy of Herbal Drugs in Human Diseases and Disorders
Evidence-Based Complementary and Alternative Medicine Efficacy of Herbal Drugs in Human Diseases and Disorders Guest Editors: Suaib Luqman, Syed Ibrahim Rizvi, André-Michael Beer, Sunil Kumar Khare, and Pinar Atukeren Efficacy of Herbal Drugs in Human Diseases and Disorders Evidence-Based Complementary and Alternative Medicine Efficacy of Herbal Drugs in Human Diseases and Disorders Guest Editors: Suaib Luqman, Syed Ibrahim Rizvi, Andre-Michael´ Beer, Sunil Kumar Khare, and Pinar Atukeren Copyright © 2014 Hindawi Publishing Corporation. All rights reserved. This is a special issue published in “Evidence-Based Complementary and Alternative Medicine.” All articles are open access articles distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Editorial Board Mahmood A. Abdulla, Malaysia Jen-Hwey Chiu, Taiwan Ching-Liang Hsieh, Taiwan Jon Adams, Australia William C. S. Cho, Hong Kong Jing Hu, China Zuraini Ahmad, Malaysia Jae Youl Cho, Republic of Korea Gan Siew Hua, Malaysia Ulysses Albuquerque, Brazil Seung-H. Cho, Republic of Korea Sheng-Teng Huang, Taiwan Gianni Allais, Italy Chee Yan Choo, Malaysia BennyTanKwongHuat,Singapore Terje Alraek, Norway Ryowon Choue, Republic of Korea Roman Huber, Germany Souliman Amrani, Morocco Shuang-En Chuang, Taiwan Angelo Antonio Izzo, Italy Akshay Anand, India Joo-Ho Chung, Republic of Korea Kong J., USA Shrikant Anant, USA Edwin L. Cooper, USA Suresh Jadhav, India Manuel Arroyo-Morales, Spain Gregory D. Cramer, USA Kanokwan Jarukamjorn, Thailand Syed Asdaq, Saudi Arabia Meng Cui, China Yong Jiang , China Seddigheh Asgary, Iran Roberto Cuman, Brazil Zheng L. Jiang, China Hyunsu Bae, Republic of Korea Vincenzo De Feo, Italy Stefanie Joos, Germany Lijun Bai, China Roc´ıo Vazquez,´ Spain Sirajudeen K.N.S., Malaysia Sandip K.