Data Exchange Interoperability Framework Between LIS and HER
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The BG News April 16, 1991
Bowling Green State University ScholarWorks@BGSU BG News (Student Newspaper) University Publications 4-16-1991 The BG News April 16, 1991 Bowling Green State University Follow this and additional works at: https://scholarworks.bgsu.edu/bg-news Recommended Citation Bowling Green State University, "The BG News April 16, 1991" (1991). BG News (Student Newspaper). 5212. https://scholarworks.bgsu.edu/bg-news/5212 This work is licensed under a Creative Commons Attribution-Noncommercial-No Derivative Works 4.0 License. This Article is brought to you for free and open access by the University Publications at ScholarWorks@BGSU. It has been accepted for inclusion in BG News (Student Newspaper) by an authorized administrator of ScholarWorks@BGSU. April 16, 1991 Tuesday Vol. 73 liiue 109 Bowling Green, Ohio The BG News BRIEFLY University may decrease Union threatens Inside The Weekend for Dem- faculty health care funds national strike of ocrats: by Jeremy Stone Weber The issue also came up at the ings well and he will not continue The Ohio College Demo- staff writer Xil 2 Faculty Senate meeting, in discussions with University crats Convention hosted istopher Dalton, vice presi- representatives," he said. The several noteworthy dent of Planning and Budgeting, firm was given two assignments: freight railroads speakers this weekend, in- Costs in faculty health care will presented a memo from himself conduct a long-range study of the cluding Attorney General increase by $1.3 million next and Vice President of Operations health care plan and suggest by Karen Ball through on their promise to Lee Fisher. year, and faculty members likely Robert Martin warning faculty ways to keep costs low imme- Associated Press Labor Wrupr strike. -
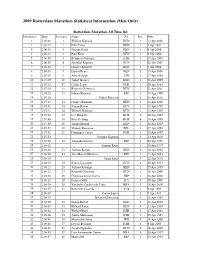
2009 Rotterdam Marathon Statistical Information (Men Only)
2009 Rotterdam Marathon Statistical Information (Men Only) Rotterdam Marathon All Time list Performances Time Performers Name Nat Place Date 1 2:05:49 1 William Kipsang KEN 1 13 Apr 2008 2 2:06:14 2 Felix Limo KEN 1 4 Apr 2004 3 2:06:38 3 Sammy Korir KEN 1 9 Apr 2006 4 2:06:44 4 Paul Kirui KEN 2 9 Apr 2006 5 2:06:50 5 Belayneh Dinsamo ETH 1 17 Apr 1988 6 2:06:50 6 Josephat Kiprono KEN 1 22 Apr 2001 7 2:06:52 7 Charles Kibiwott KEN 3 9 Apr 2006 8 2:06:58 8 Daniel Rono KEN 2 13 Apr 2008 9 2:07:07 9 Ahmed Salah DJI 2 17 Apr 1988 10 2:07:09 10 Japhet Kosgei KEN 1 18 Apr 1999 11 2:07:12 11 Carlos Lopes POR 1 20 Apr 1985 12 2:07:18 12 Kenneth Cheruiyot KEN 2 22 Apr 2001 13 2:07:23 13 Fabian Roncero ESP 2 18 Apr 1999 14 2:07:26 Fabian Roncero 1 19 Apr 1998 15 2:07:33 14 Charles Kamathi KEN 3 13 Apr 2008 16 2:07:41 15 Simon Biwott KEN 3 18 Apr 1999 17 2:07:42 16 William Kiplagat KEN 1 13 Apr 2003 18 2:07:44 17 Lee Bong-Ju KOR 2 19 Apr 1998 19 2:07:49 18 Kim Yi-Yong KOR 4 18 Apr 1999 20 2:07:50 19 Jimmy Muindi KEN 1 10 Apr 2005 21 2:07:51 20 Vincent Rousseau BEL 1 17 Apr 1994 22 2:07:51 21 Domingos Castro POR 1 20 Apr 1997 23 2:07:53 Josephat Kiprono 2 13 Apr 2003 24 2:07:54 22 Alejandro Gomez ESP 2 20 Apr 1997 25 2:08:02 Sammy Korir 3 20 Apr 1997 26 2:08:02 23 Jackson Koech KEN 2 10 Apr 2005 27 2:08:09 24 Jose Manuel Martinez ESP 3 13 Apr 2003 28 2:08:14 Samy Korir 3 22 Apr 2001 29 2:08:19 25 Simon Loywapet KEN 4 20 Apr 1997 30 2:08:21 26 Joshua Chelanga KEN 1 15 Apr 2007 31 2:08:22 27 Kenneth Cheruiyot KEN 1 16 Apr 2000 32 2:08:30 28 Francisco -

Updated 2019 Completemedia
April 15, 2019 Dear Members of the Media, On behalf of the Boston Athletic Association, principal sponsor John Hancock, and all of our sponsors and supporters, we welcome you to the City of Boston and the 123rd running of the Boston Marathon. As the oldest annually contested marathon in the world, the Boston Marathon represents more than a 26.2-mile footrace. The roads from Hopkinton to Boston have served as a beacon for well over a century, bringing those from all backgrounds together to celebrate the pursuit of athletic excellence. From our early beginnings in 1897 through this year’s 123rd running, the Boston Marathon has been an annual tradition that is on full display every April near and far. We hope that all will be able to savor the spirit of the Boston Marathon, regardless whether you are an athlete or volunteer, spectator or member of the media. Race week will surely not disappoint. The race towards Boylston Street will continue to showcase some of the world’s best athletes. Fronting the charge on Marathon Monday will be a quartet of defending champions who persevered through some of the harshest weather conditions in race history twelve months ago. Desiree Linden, the determined and resilient American who snapped a 33-year USA winless streak in the women’s open division, returns with hopes of keeping her crown. Linden has said that last year’s race was the culmination of more than a decade of trying to tame the beast of Boston – a race course that rewards those who are both patient and daring. -

USATF Cross Country Championships Media Handbook
TABLE OF CONTENTS NATIONAL CHAMPIONS LIST..................................................................................................................... 2 NCAA DIVISION I CHAMPIONS LIST .......................................................................................................... 7 U.S. INTERNATIONAL CROSS COUNTRY TRIALS ........................................................................................ 9 HISTORY OF INTERNATIONAL CHAMPIONSHIPS ........................................................................................ 20 APPENDIX A – 2009 USATF CROSS COUNTRY CHAMPIONSHIPS RESULTS ............................................... 62 APPENDIX B –2009 USATF CLUB NATIONAL CHAMPIONSHIPS RESULTS .................................................. 70 USATF MISSION STATEMENT The mission of USATF is to foster sustained competitive excellence, interest, and participation in the sports of track & field, long distance running, and race walking CREDITS The 30th annual U.S. Cross Country Handbook is an official publication of USA Track & Field. ©2011 USA Track & Field, 132 E. Washington St., Suite 800, Indianapolis, IN 46204 317-261-0500; www.usatf.org 2011 U.S. Cross Country Handbook • 1 HISTORY OF THE NATIONAL CHAMPIONSHIPS USA Track & Field MEN: Year Champion Team Champion-score 1954 Gordon McKenzie New York AC-45 1890 William Day Prospect Harriers-41 1955 Horace Ashenfelter New York AC-28 1891 M. Kennedy Prospect Harriers-21 1956 Horace Ashenfelter New York AC-46 1892 Edward Carter Suburban Harriers-41 1957 John Macy New York AC-45 1893-96 Not Contested 1958 John Macy New York AC-28 1897 George Orton Knickerbocker AC-31 1959 Al Lawrence Houston TFC-30 1898 George Orton Knickerbocker AC-42 1960 Al Lawrence Houston TFC-33 1899-1900 Not Contested 1961 Bruce Kidd Houston TFC-35 1901 Jerry Pierce Pastime AC-20 1962 Pete McArdle Los Angeles TC-40 1902 Not Contested 1963 Bruce Kidd Los Angeles TC-47 1903 John Joyce New York AC-21 1964 Dave Ellis Los Angeles TC-29 1904 Not Contested 1965 Ron Larrieu Toronto Olympic Club-40 1905 W.J. -

2020 Virgin Money London Marathon 2020 Virgin Money London Marathon 1
2020 Virgin Money London Marathon 2020 Virgin Money London Marathon 1 CONTENTS 01 MEDIA INFORMATION Page 5 ELITE MEN 42 The Events & Start Times 6 Entries 42 Media Team Contacts 6 Awards & Bonuses 42 Media Facilities 6 Preview 43 Press Conferences 6 Biographies 44 The London Marathon Online 7 Olympic Qualifying Standard 54 Essential Facts 8 What’s New in 2020 10 ELITE WHEELCHAIR PREVIEW 55 The Course 11 Wheelchair Athletes 56 Stephen Lawrence Charitable Trust 11 Abbott World Marathon Elite Race Route Map 12 Majors Accumulator 56 Pace Guide 13 T54 Women Entries 56 Running a Sustainable Marathon 14 Biographies 57 London Marathon Events Limited 15 T54 Men Entries 59 Biographies 60 02 THE 40TH RACE 16 How It All Began 17 05 ABBOTT WORLD Four Decades of Marathon Moments 19 MARATHON MAJORS 65 The Ever Presents 23 How It Works 66 Qualifying Races 67 03 CHARITIES, FUNDRAISING AbbottWMM Wanda Age Group & THE TRUST 25 World Championships 67 Charities & Fundraising 26 The Abbott World Marathon 2020 Charity of the Year – Mencap 27 Majors Races 68 The London Marathon Charitable Trust 33 Abbott World Marathon Majors Series XIII (2019/20) 74 04 ELITE RACES 31 Abbott World Marathon Majors Wheelchair Series 76 ELITE WOMEN 32 Entries 32 Awards & Bonuses 32 Preview 33 Biographies 34 CONTENTS CONTINUED >> 2020 Virgin Money London Marathon 2 06 THE MASS EVENT 79 BRITISH MARATHON STATISTICS 119 Starters & Finishers 80 British All-Time Top 20 119 2020 Virgin Money British Record Progression 120 London Marathon Virtual Race Stats 81 The Official Virgin Money -

5.000 Metros
07_HOM_03_fondo_Layout 2 07/01/2015 10:20 Página 105 CRONOLOGIA DE LOS RECORDS Y MEJORES MARCAS ESPAÑOLAS DE ATLETISMO 5.000 metros 20.00.0 José Quirante F.C.Barcelona Cataluña Barcelona 06-05-1906 Fiesta deportiva. Campo del F.C. Barcelona. Intento de record de 20 minutos. 1. Quirante 5.262 metros, 2. Gil. Esta marca su- pone aproximadamente 19 minutos en los 5.000 metros. Quirante batió su propio record de 5.175, marca que aún no hemos localizado. 18.28.6 José Tovar Castilla Madrid 04-08-1907 Pista del Retiro. 1. Tovar 18.28.6, 2. Jerónimo López 18.33.0, 3. Luis Bernardos 18.44.0, 4. Vicente Manchón 19.34.0, 5. Do- roteo Rodríguez 19.34.4. 17.52.0 José Tovar Castilla Madrid 29-03-1908 Festival de la Sociedad Gimnástica Española. Campo de los Altos del Hipódromo. 1. Tovar 17.52.0, 2. Francisco de Diego 17.53.0, 3. Isidro Aguilar 18.51.0, 4. Morales 19.17.0. 16.49.8 Pedro Prat F.C.Barcelona Cataluña Barcelona 05-07-1914 Concurso olímpico del Sindicato de Periodistas Deportivos. Campo del R.C. Polo. 1. Prat 16.49.8, 2. L. Alcalde 16.51.0, 3. José Erce 16.51.8. 16.43.0 José María Ugalde Jolastokieta Guipúzcoa Alza 31-07-1914 Festival internacional. Campo del Jolastokieta. 1. Lespielle (FRA) 16.33.0, 2. Ugalde 16.43.0, 3. Edmundo Medina, 16.57.0. 16.19.2 Pedro Prat F.C.Barcelona Cataluña Barcelona 11-03-1915 Intento de record al paso para la legua. -

2010 Fukuoka Marathon Statistics by K. Ken Nakamura
2020201020 101010 Fukuoka Marathon Statistical Information Fukuoka Marathon All Time list Performances Time Performers Name Nat Place Date 1 2:05:18 1 Tsegaye Kebede ETH 1 6 Dec 2009 2 2:06:10 Tsegaye Kebede 1 7 Dec 2008 3 2:06:39 2 Samuel Wanjiru KEN 1 2 Dec 2007 4 2:06:50 3 Deriba Merga ETH 2 2 Dec 2007 5 2:06:51 4 Atsushi Fujita JPN 1 3 Dec 2000 6 2:06:52 5 Haile Gebrselassie ETH 1 3 Dec 2006 7 2:07:13 6 Atsushi Sato JPN 3 2 Dec 2007 8 2:07:15 7 Dmytro Barnovskyy UKR 2 3 Dec 2006 9 2:07:19 8 Jaouad Gharib MAR 3 3 Dec 2006 10 2:07:28 9 Josiah Thugwane RSA 1 7 Dec 1997 11 2:07:52 10 Tomoaki Kunichika JPN 1 7 Dec 2003 12 2:07:52 11 Kebede Tekeste ETH 2 6 Dec 2009 13 2:07:54 12 Gezahegne Abera ETH 1 5 Dec 1999 14 2:07:55 13 Mohammed Ouaadi FRA 2 5 Dec 1999 15 2:07:55 14 Toshinari Suwa JPN 2 7 Dec 2003 16 2:07:59 15 Toshinari Takaoka JPN 3 7 Dec 2003 17 2:08:07 16 Toshiyuki Hayata JPN 2 7 Dec 1997 18 2:08:10 17 Antonio Peña ESP 4 7 Dec 2003 19 2:08:18 18 Robert de Castella AUS 1 6 Dec 1981 20 2:08:18 19 Takeyuki Nakayama JPN 1 6 Dec 1987 21 2:08:19 Dmytro Barnovskyy 3 6 Dec 2009 22 2:08:21 20 Hailu Negussie ETH 5 7 Dec 2003 23 2:08:29 Dmytro Barnovskyy 1 4 Dec 2005 24 2:08:36 21 Dereje Tesfaye Gebrehiwot ETH 4 6 Dec 2009 25 2:08:37 22 Tsuyoshi Ogata JPN 6 7 Dec 2003 26 2:08:40 23 Vanderlei de Lima BRA 3 5 Dec 1999 27 2:08:42 24 Jackson Kabiga KEN 1 6 Dec 1998 28 2:08:47 25 Nozomi Saho JPN 3 7 Dec 1997 29 2:08:48 26 Nobuyuki Sato JPN 2 6 Dec 1998 30 2:08:48 27 Tadayuki Ojima JPN 7 7 Dec 2003 31 2:08:49 28 Wataru Okutani JPN 4 3 Dec 2006 32 -

Ethiopian Marathon Hero Coaches Youth Athletes
GRASSROOTS AMBASSADOR The JET Programme Kasama Inari Shrine, a symbol of the city, is included along the route of the annual Kasama Togeinosato Half Ministers and Olympic medalists Marathon. from Ethiopia shown while visiting Japan for the Kasama Togeinosato Ethiopian Marathon Hero Half Marathon held in 2019. Running together with Mekonnen, they established good relationships with Coaches Youth Athletes the people of Kasama. Making people smile wherever he goes, a long-distance running legend from Ethiopia lives and works in a rural Japanese town! bebe Mekonnen, Ethiopian Shrine. The city is also famous for Athletics Federation, made a visit long-distance running its style of porcelain known as there in March 2019, also with the A Each piece of Kasama-ware is characterized by the artist’s hero, won the Tokyo International Kasama-ware. About forty years ago, purpose of coaching students of individuality. They create pieces that are free from tradition Marathon three times, along with an Ethiopian potter fascinated with an athletics class. It was Tulu who Kasama is Japan’s largest producer of chestnuts. and formalities. various other famous races, including the style of pottery moved to the advised Mekonnen to work there the Beijing Marathon and Boston region, which led the long-term as an SEA. She told me that she Marathon. He also competed twice connection with the country that has had been very warmly received by beautiful, and the people are warm Mekonnen-sensei means by saying This strong, kind Ethiopian hero is in the Summer Olympics. This past lasted many years. the people of Kasama, which made and friendly. -

39Th IAAF WORLD CROSS COUNTRY CHAMPIONSHIPS
39th IAAF WORLD CROSS COUNTRY CHAMPIONSHIPS Facts & Figures Facts & Figures ......................................................................................................1 Summary of Past Championships ..........................................................................2 Ages of World Cross Country Champions..............................................................6 Most Appearances..................................................................................................7 Medal Tables – by Athlete ......................................................................................8 Medal Tables – by Country .....................................................................................9 Spain at the World Cross Country Championships...............................................11 Doping cases at the World Cross Country Championships ..................................11 Age Falsifications at the World Cross Country Championships............................11 PUNTA UMBRÍA 2011 ★ FACTS & FIGURES 1 FACTS & FIGURES Some 10,512 athletes from 167 countries have competed in the Ismael Kirui, junior team gold medallist in 1990 at 15 years 32 days. IAAF World Cross Country Championships, with athletes from six Individually, the youngest is Robert Kipchumba, 2000 World Junior countries participating in all 38 editions: Belgium, France, Great Cross Country Champion at 16 years 24 days. Britain & NI (ENG, GBR, NIR, SCO, WAL), Ireland, Spain, and the The youngest competitor is Su Su-Ning of Chinese Taipei who United -

A Brief History of the World Cross Country Championships by Ken Namaura the First 70 Years the World Cross Country Championshi
A Brief History of the World Cross Country Championships By Ken Namaura The first 70 years The World Cross Country Championships, often considered the toughest footraces on the planet, may be more difficult to win than the Olympics or the World Championships in Athletics. The predecessor of the World Cross Country Championships was the International Cross Country Championships, inaugurated in 1903. With only four countries (England, Wales, Scotland and Ireland) initially participating, these championships could hardly be considered “international” during their early years. However, by 1972, when 197 runners from 15 countries competed, the championships had gained international stature. Three great runners — Jack Holden (GBR), the 1950 European marathon champion; Alain Mimoun (FRA), the 1956 Olympic marathon champion; and Gaston Roelants (BEL), the 1964 Olympic 3000mSC champion — each won four individual titles during the days of International Cross Country Championships. In the women’s event, Doris Brown won five straight championships from 1967 to 1971. Many Olympic medalists won the International Cross Country Championships. Jean Bouin (FRA), who won the silver medal at 5000m in the 1912 Olympics, won three championships from 1911, while Mohammed Gommoudi (TUN), who was second at 5000m in the 1968 Olympics won the International Cross Country Championships in the same year. Franjo Mihalic (YUG), Rhadi ben Abdesselem (MAR), and Basil Heatley (GBR), all Olympic marathon silver medalist, won the International Cross Country Championships. However, because participation was generally limited to runners from nations that were members of the International Cross Country Union (ICCU), the championships were not truly “world” in scope. In fact, Emil Zatopek (CZE), 1952 Helsinki triple gold medalist, and Vladimir Kuts (URS), 1956 Melbourne double Olympic champion, never competed at the International Cross Country Championships. -

Victorian Marathon Club Newsletter
VICTORIAN MARATHON CLUB JUNE 1991 Price $ 2- NEWSLETTER ISSN 1030-8717 Lonely ?!? Not in VMC events ! Seen at runs clockwise from above: Fallen Comrades in the Domain. 25km at Albert Park Lake. Women 10km Queen of the Lake at Albert Park. From 10km up to the 42.2km Marathon, the VMC has given the lead for 45 years. Registered by Australia Post Publication No. VBH 0488 VMC NEWSLETTER is published for the information of members of the VICTORIAN MARATHON CLUB MELBOURNE INC. and is part of the Annual Membership Fee. It is issued quarterly: AUTUMN (March), WINTER (June), SPRING (September), SUMMER (December). ALL RUNNERS are invited to contribute letters, results, p h o t o s , comments, criti cisms, etc. to the EDITOR, 1 Golding Street, CANTERBURY 3126, Victoria. PLEASE NOTE that material submitted for publication is preferred to be typed single-spaced and not exceeding 1.5 pages of A4 sheets, ideally less than 1 page. Articles MUST BE accompanied by name and address of the contributor, together with his or her signature. The Author of such article shall retain full responsibility for its contents. DEADLINE PC® COPY is the 1st day of the month preceding the month of publication. Earlier copy is preferred to ease pressure on editing and printing schedules. INTERSTATE LINES OF (XfrMUNICATIONS. VICTORIAN MARATHON CLUB MELBOURNE INC. P.O.BOX 12234, A ’BECKETT ST, MELB 3000 FAX: Mon, Wed, Fri 7.30pn-9.30pm (03) 499-3069 AA: Neil KING, P.O.Box 254, MOONEE PONDS 3039 (03) 370-7555 NSW AA: Alan BATCHELOR, P.O.Box N101, Grosvenor St, SYDNEY 2001 (02) 241-3538 VAA: Sharon STEWART, Olympic Park, Swan St, MELBOURNE 3002 (03)428 8195/8049 QAA: Reg BRANDIS, QE2 Stadium, Kessels Rd, NATHAN 4111 (07) 343-5653 AA-SA: Kath EDWARDS, P.O.Box 57, KENSINGTON PARK 5068 (08) 332-8022 AA-WA: CHRIS STANTON, P.O.Box 208, WEMBLEY 6014 (09) 387-5599 AAA-TAS: Wayne MASON, DOMAIN ATHLETIC CENTRE, 7001 (002) 34-9551 ACT AA: JOHN HARDING P.O.Box 35, BELC0NNEN 2616 (062) 53-1150H NT AA: Greg ADAMS, P.O.Box 105, SANDERSON N.T. -

The BG News April 17, 1990
Bowling Green State University ScholarWorks@BGSU BG News (Student Newspaper) University Publications 4-17-1990 The BG News April 17, 1990 Bowling Green State University Follow this and additional works at: https://scholarworks.bgsu.edu/bg-news Recommended Citation Bowling Green State University, "The BG News April 17, 1990" (1990). BG News (Student Newspaper). 5073. https://scholarworks.bgsu.edu/bg-news/5073 This work is licensed under a Creative Commons Attribution-Noncommercial-No Derivative Works 4.0 License. This Article is brought to you for free and open access by the University Publications at ScholarWorks@BGSU. It has been accepted for inclusion in BG News (Student Newspaper) by an authorized administrator of ScholarWorks@BGSU. FALCONS WIN AGAIN Dickinson's late inning home run breaks open close game; 13-7 victory over Defiance a tune-up for today's games with Kent.. .see Sports p.9 The Nation ys Best College Newspaper Weather Tuesday Vol.72 Issue 113 April 17,1990 Bowling Green, Ohio High 40e The BG News Low 20° BRIEFLY New building approved by Matt MigheU eral fees. increase of the $21 fee students are currently paying CAMPUS staff writer The students are in favor of the new facility, but 51 for the recreation center per semester, making the percent of those polled said they always are able to semesterly fee about $36 each semester. find space for their desired activity. The state will be footing two-thirds of the building's Chinese speaker: Sun Final design for the new University intramu- The building will be used primarily for intramural maintenance costs, leaving an additional $7.31 per Tianyi, president of the Xi'an Foreign ral/field house facility gained unanimous approval activities and physical education classes, but also semester to be added to general fees.