Rodent Models of Depression
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Alpha1a Adrenergic Receptor Influences on Adult Neurogenesis, Cell Fate, Mood, Learning, Memory, Lifespan, and Cancer Incidence Katie Collette
University of North Dakota UND Scholarly Commons Theses and Dissertations Theses, Dissertations, and Senior Projects January 2015 Alpha1a Adrenergic Receptor Influences On Adult Neurogenesis, Cell Fate, Mood, Learning, Memory, Lifespan, And Cancer Incidence Katie Collette Follow this and additional works at: https://commons.und.edu/theses Recommended Citation Collette, Katie, "Alpha1a Adrenergic Receptor Influences On Adult Neurogenesis, Cell Fate, Mood, Learning, Memory, Lifespan, And Cancer Incidence" (2015). Theses and Dissertations. 1757. https://commons.und.edu/theses/1757 This Dissertation is brought to you for free and open access by the Theses, Dissertations, and Senior Projects at UND Scholarly Commons. It has been accepted for inclusion in Theses and Dissertations by an authorized administrator of UND Scholarly Commons. For more information, please contact [email protected]. ALPHA1A ADRENERGIC RECEPTOR INFLUENCES ON ADULT NEUROGENESIS, CELL FATE, MOOD, LEARNING, MEMORY, LIFESPAN, AND CANCER INCIDENCE by Katie M. Collette Bachelor of Science, University of North Dakota, 2010 A Dissertation Submitted to the Graduate Faculty of the University of North Dakota in partial fulfillment of the requirements for the degree of Doctor of Philosophy Grand Forks, North Dakota May 2015 Copyright 2015 Katie Collette ii This thesis, submitted by Katie M. Collette in partial fulfillment of the requirements for the Degree of Doctor of Philosophy from the University of North Dakota, has been read by the Faculty Advisory Committee under whom the work has been done and is hereby approved. __________________________________ Chairperson, Van Doze __________________________________ Holly Brown-Borg __________________________________ Diane Darland __________________________________ James Haselton __________________________________ Joyce Ohm This dissertation meets the standards for appearance, conforms to the style and format requirements of the Graduate School of the University of North Dakota, and is hereby approved. -

Using Tests and Models to Assess Antidepressant-Like Activity in Rodents Ewa Kedzierska1*, Izabela Wach2
DOI: 10.1515/cipms-2016-0013 Curr. Issues Pharm. Med. Sci., Vol. 29, No. 2, Pages 61-65 Current Issues in Pharmacy and Medical Sciences Formerly ANNALES UNIVERSITATIS MARIAE CURIE-SKLODOWSKA, SECTIO DDD, PHARMACIA journal homepage: http://www.curipms.umlub.pl/ Using tests and models to assess antidepressant-like activity in rodents Ewa Kedzierska1*, Izabela Wach2 1 Chair and Department of Pharmacology and Pharmacodynamics, Medical University of Lublin, Chodzki 4A, 20-093 Lublin, Poland 2 Student Research Group at the Chair and Department of Pharmacology and Pharmacodynamics, Medical University of Lublin, Chodzki 4A, 20-093 Lublin, Poland ARTICLE INFO ABSTRACT Received 08 February 2016 In today's world, depression is one of the more prevalent forms of mental illness. According Accepted 10 March 2016 to WHO, about 10%-30% of all women and 7%-15% of all men are afflicted by depression Keywords: at least once in their life-times. Today, depression is assessed to be affecting 350 million depression, people. Regarding this issue, an important challenge for current psychopharmacology animal models, is to develop new, more effective pharmacotherapy and to understand the mechanism atidepressants. of action of known antidepressants. Furthermore, there is the necessity to improve the effectiveness of anti-depression treatment by way of bringing about an understanding of the neurobiology of this illness. In achieving these objectives, animal models of depression can be useful. Yet, presently, all available animal models of depression rely on two principles: the actions of known antidepressants or the responses to stress. In this paper, we present an overview of the most widely used animal tests and models that are employed in assessing antidepressant-like activity in rodents. -

Genetic Regulation of Behavioral and Neuronal Responses to Fluoxetine
Neuropsychopharmacology (2008) 33, 1312–1322 & 2008 Nature Publishing Group All rights reserved 0893-133X/08 $30.00 www.neuropsychopharmacology.org Genetic Regulation of Behavioral and Neuronal Responses to Fluoxetine 1 1 1 1 ,1 Brooke H Miller , Laura E Schultz , Anisha Gulati , Michael D Cameron and Mathew T Pletcher* 1Department of Molecular Therapeutics, The Scripps Research InstituteFScripps Florida, Jupiter, FL, USA Despite widespread use of antidepressants, the factors underlying the behavioral response to antidepressants are unknown. It has been shown that antidepressant treatment promotes the proliferation and survival of neurons in the adult hippocampus via enhanced serotonergic signaling, but it is unclear whether hippocampal neurogenesis is responsible for the behavioral response to antidepressants. Furthermore, a large subpopulation of patients fails to respond to antidepressant treatment due to presumed underlying genetic factors. In the present study, we have used the phenotypic and genotypic variability of inbred mouse strains to show that there is a genetic component to both the behavioral and neuronal effects of chronic fluoxetine treatment, and that this antidepressant induces an increase in hippocampal cell proliferation only in the strains that also show a positive behavioral response to treatment. Furthermore, the behavioral and neuronal responses are associated with an upregulation of genes known to promote neuronal proliferation and survival. These results suggest that inherent genetic predisposition to increased serotonin-induced neurogenesis may be a determinant of antidepressant efficacy. Neuropsychopharmacology (2008) 33, 1312–1322; doi:10.1038/sj.npp.1301497; published online 4 July 2007 Keywords: inbred mouse strains; fluoxetine; tail suspension test; neurogenesis; BrdU; depression INTRODUCTION has, therefore, been hypothesized that increased mono- aminergic transmission is a precursor to molecular and Major depressive disorder (MDD) affects up to 5% of the neural changes that underlie the remission of depression. -
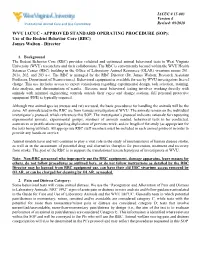
(SOP): Use of the Rodent Behavior Core (RBC) James Walton - Director
IACUC # 15-003 Version 4 Institutional Animal Care and Use Committee Revised: 09/2020 WVU IACUC - APPROVED STANDARD OPERATING PROCEDURE (SOP): Use of the Rodent Behavior Core (RBC) James Walton - Director 1. Background The Rodent Behavior Core (RBC) provides validated and optimized animal behavioral tests to West Virginia University (WVU) researchers and their collaborators. The RBC is conveniently located within the WVU Health Sciences Center (HSC) building in the Office of Laboratory Animal Resources (OLAR) vivarium rooms 201, 201a, 202, and 203 a-c. The RBC is managed by the RBC Director (Dr. James Walton; Research Assistant Professor, Department of Neuroscience). Behavioral equipment is available for use by WVU investigators free of charge. This use includes access to expert consultation regarding experimental design, task selection, training, data analysis, and dissemination of results. Because most behavioral testing involves working directly with animals with minimal engineering controls outside their cages and change stations, full personal protective equipment (PPE) is typically required. Although two animal species (mouse and rat) are used, the basic procedures for handling the animals will be the same. All animals used in the RBC are from various investigators at WVU. The animals remain on the individual investigator’s protocol, which references this SOP. The investigator’s protocol indicates rationale for requesting experimental animals, experimental groups, numbers of animals needed, behavioral tests to be conducted, assurances or justifications regarding duplication of previous work, and/or length of the study (as appropriate for the tests being utilized). All appropriate RBC staff members must be included in each animal protocol in order to provide any hands-on service. -

Evaluation of the Antidepressant Potential of Dextromethorphan
Graduate Theses, Dissertations, and Problem Reports 2015 Evaluation of the antidepressant potential of dextromethorphan Linda Nguyen Follow this and additional works at: https://researchrepository.wvu.edu/etd Recommended Citation Nguyen, Linda, "Evaluation of the antidepressant potential of dextromethorphan" (2015). Graduate Theses, Dissertations, and Problem Reports. 6309. https://researchrepository.wvu.edu/etd/6309 This Dissertation is protected by copyright and/or related rights. It has been brought to you by the The Research Repository @ WVU with permission from the rights-holder(s). You are free to use this Dissertation in any way that is permitted by the copyright and related rights legislation that applies to your use. For other uses you must obtain permission from the rights-holder(s) directly, unless additional rights are indicated by a Creative Commons license in the record and/ or on the work itself. This Dissertation has been accepted for inclusion in WVU Graduate Theses, Dissertations, and Problem Reports collection by an authorized administrator of The Research Repository @ WVU. For more information, please contact [email protected]. Evaluation of the antidepressant potential of dextromethorphan Linda Nguyen A dissertation submitted to the School of Pharmacy at West Virginia University in partial fulfillment of the requirements for the degree of Doctor of Philosophy in Pharmacological and Pharmaceutical Sciences Han-Ting Zhang, M.D./Ph.D., Chair Rae R. Matsumoto, Ph.D. David P. Siderovski, Ph.D. Paola Pergami, M.D./Ph.D. Patrick J. Marshalek, M.D. Department of Behavioral Medicine and Psychiatry Morgantown, West Virginia 2015 Keywords: dextromethorphan, ketamine, imipramine, dextrorphan, depression, antidepressant, sigma-1 receptors, AMPA receptors, BDNF, NGF © 2015 Linda Nguyen ABSTRACT Evaluation of the antidepressant potential of dextromethorphan Linda Nguyen Depression affects more than 350 million people and is the leading cause of disability worldwide. -
Anxiety-Like but Not Despair-Like Behaviors Are Further Aggravated
bioRxiv preprint doi: https://doi.org/10.1101/202283; this version posted October 12, 2017. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Anxiety-like but not despair-like behaviors are further aggravated by chronic mild stress in the early stages of APPswe/PS1dE9 transgenic mice Jun-Ying Gao1,2,#, Ying Chen1,#, Dong-Yuan Su1, Charles Marshall3, and Ming Xiao1,2,* 1 Jiangsu Province Key Laboratory of Neurodegeneration, Nanjing Medical University, Nanjing, Jiangsu, China 2 Key Laboratory for Aging &Disease, Nanjing Medical University, Nanjing, Jiangsu, China 3 Department of Rehabilitation Sciences, University of Kentucky Center for Excellence in Rural Health, Hazard, KY # Equal contributors. * Corresponding author at: Jiangsu Key Laboratory of Neurodegeneration, Nanjing Medical University, No. 101 Longmian Avenue, Nanjing, Jiangsu 211166, China. E-mail address: [email protected] (M. Xiao). 1 bioRxiv preprint doi: https://doi.org/10.1101/202283; this version posted October 12, 2017. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. ABSTRACT Early Alzheimer’s disease (AD) and depression share many symptoms, thus it is very difficult to initially distinguish one from the other. Therefore, characterizing the shared and different biological changes between the two disorders will be helpful in making an early diagnosis and planning treatment. In the present study, 8-week-old APPswe/PS1dE9 transgenic mice received chronic mild stress (CMS) for 8 weeks followed by a series of behavioral, biochemical and pathological analyses. -

Monoaminergic Regulation of Mecp2 Phosphorylation in Mouse Models of Psychiatric Disease
Monoaminergic Regulation of MeCP2 Phosphorylation in Mouse Models of Psychiatric Disease Ashley N. Hutchinson Department of Pharmacology Duke University Date____________________ Approved: ________________________ Anne West, Supervisor ________________________ Marc Caron ________________________ Cynthia Kuhn ________________________ Donald McDonnell ________________________ Theodore Slotkin ________________________ William Wetsel Dissertation submitted in partial fulfillment of the requirements of the degree of Doctor of Philosophy in the Department of Pharmacology and Cancer Biology in the Graduate School of Duke University 2011 ABSTRACT Monoaminergic Regulation of MeCP2 Phosphorylation in Mouse Models of Psychiatric Disease Ashley N. Hutchinson Department of Pharmacology Duke University Date____________________ Approved: ________________________ Anne West, Supervisor ________________________ Marc Caron ________________________ Cynthia Kuhn ________________________ Donald McDonnell ________________________ Theodore Slotkin ________________________ William Wetsel An abstract of a dissertation submitted in partial fulfillment of the requirements of the degree of Doctor of Philosophy in the Department of Pharmacology and Cancer Biology in the Graduate School of Duke University 2011 Copyright by Ashley Hutchinson 2011 ABSTRACT Activation of monoaminergic receptors is essential to the mechanism by which psychostimulants and antidepressants induce changes in behavior. Although these drugs rapidly increase monoaminergic transmission, they need -

Animal Models of Depression: Pros and Cons
Cell and Tissue Research (2019) 377:5–20 https://doi.org/10.1007/s00441-018-2973-0 REVIEW Animal models of depression: pros and cons Jaanus Harro1 Received: 31 August 2018 /Accepted: 23 November 2018 /Published online: 17 December 2018 # Springer-Verlag GmbH Germany, part of Springer Nature 2018 Abstract Animal models of depression are certainly needed but the question in the title has been raised owing to the controversies in the interpretation of the readout in a number of tests, to the perceived lack of progress in the development of novel treatments and to the expressed doubts in whether animal models can offer anything to make a true breakthrough in understanding the neurobi- ology of depression and producing novel drugs against depression. Herewith, it is argued that if anything is wrong with animal models, including those for depression, it is not about the principle of modelling complex human disorder in animals but in the way the tests are selected, conducted and interpreted. Further progress in the study of depression and in developing new treatments, will be supported by animal models of depression if these were more critically targeted to drug screening vs. studies of underlying neurobiology, clearly stratified to vulnerability and pathogenetic models, focused on well-defined endophenotypes and validated for each setting while bearing the existing limits to validation in mind. Animal models of depression need not to rely merely on behavioural readouts but increasingly incorporate neurobiological measures as the understanding of depression as human brain disorder advances. Further developments would be fostered by cross-fertilizinga translational approach that is bidirectional, research on humans making more use of neurobiological findings in animals. -

January 1, 2019 Onwards
2020-APHIS-02021-F Nagelhout, Mark Animal Protection League of NJ 1/28/2020 2/26/2020 Please provide any records and reports of any institution names, institution addresses and depredation control facilities who requested deer depredation control permits in New Jersey from 1/1/2014 - present (Date Range for Record Search: From 01/01/2014 To 01/28/2020) 2020-APHIS-01731-F Cruzado, Manual BALDACCI COFFEE ROASTER LLC 1/10/2020 2/10/2020 Requesting any letter and communication issued by the Department of Agricultural of Puerto Rico and that is recorded in BALDACCI COFFEE ROASTER LLC Compliance Agreement file. The Compliance Agreement is PR-SO-19-0001. 2020-APHIS-01900-F Wiltshire, Molly Schiff Hardin LLP 1/17/2020 2/18/2020 Requesting the following records from the Animal Plant Health Inspection Service regarding the articulated tug-and-barge vessel 1.) Documents requested or received by APHIS regarding the April 1, 2018 anchor strike incident involving the ATB, in which its anchor struck ATC's underwater transmission cables, Enbridge's oil pipeline, or other structures lying on the bottomlands of the Straits of Mackinac (the "Anchor Strike Incident"). 2.) APHIS communications regarding the Anchor Strike Incident, including Incident response, investigation, environmental impacts or remediation efforts. 3.) Video, photos, or data regarding the ATB or the Anchor Strike Incident. 4.) APHIS documents or communications about costs of incident response, investigation, or remediation of the Anchor Strike Incident. 2020-APHIS-01624-F Garvin, Courtney Sandy Parks Attorneys at Law 1/7/2020 2/5/2020 This request is in follow up to FOIA Request 2019-APHIS-06553-F. -

Vmat2heterozygous Mutant Mice Display a Depressive-Like Phenotype
10520 • The Journal of Neuroscience, September 26, 2007 • 27(39):10520–10529 Behavioral/Systems/Cognitive Vmat2 Heterozygous Mutant Mice Display a Depressive-Like Phenotype Masato Fukui,1 Ramona M. Rodriguiz,1 Jiechun Zhou,1 Sara X. Jiang,1 Lindsey E. Phillips,1 Marc G. Caron,2 and William C. Wetsel1,3 1Department of Psychiatry and Behavioral Sciences, Mouse Behavioral and Neuroendocrine Analysis Core Facility, 2Department of Cell Biology, and 3Departments of Cell Biology and Neurobiology, Duke University Medical Center, Durham, North Carolina 27710 The vesicular monoamine transporter 2 (VMAT2) is localized primarily within the CNS and is responsible for transporting monoamines from the cytoplasm into secretory vesicles. Because reserpine (a VMAT inhibitor) can precipitate depressive-like symptoms in humans, we investigated whether Vmat2 heterozygous (HET) mice present with depressive-like behaviors. The mutants showed locomotor and rearing retardation in the open field and appeared anhedonic to 1 and 1.5% sucrose solutions. Immobility times for Vmat2 heterozygotes were prolonged in forced swim and imipramine normalized this behavior. HET animals also showed enhanced immobility in tail sus- ␥ ␣ pension and this response was alleviated by fluoxetine, reboxetine, and bupropion. Stimulated GTP S binding indicated that 2- adrenergic receptors in HET hippocampus were more sensitive to UK 14,304 (5-bromo-N-(4,5-dihydro-1-H-imidazol-2-yl)-6- quinoxalinamine) stimulation than in wild type (WT) mice. In learned helplessness, mice were exposed to a shuttle box for4dorwere given inescapable foot-shocks for the same time period. On day 5, all animals were tested in shock escape. Failure rates and the latency to escape were similar for WT and HET mice that were only pre-exposed to the test apparatus. -

Abstracts of Scientific Presentations 2018 AALAS National Meeting Baltimore, Maryland
Journal of the American Association for Laboratory Animal Science Vol 57, No 5 Copyright 2018 September 2018 by the American Association for Laboratory Animal Science Pages 534–642 Abstracts of Scientific Presentations 2018 AALAS National Meeting Baltimore, Maryland Poster Sessions once approximately every 3 y. The purpose of this in-person training is to review protocol requirements and campus-specific policies and P1 Food for Thought: The Development of Drug-loaded Diets to guidelines that involve survival surgery to assure that quality Improve Both Science and Welfare standards are being met regarding the administration of anesthetics as well as pre-, intra-, and postoperative analgesics. These meetings, held AA Ritchie*, P Clarke, P Collier, A Grabowska by the training and compliance staff members, also provide laboratory personnel with an opportunity to obtain guidance on best practices or Cancer Biology, University of Nottingham, Nottingham, United review any aspects of their protocols that require clarification. Since its Kingdom inception in 2009, this important component of postapproval monitoring has identified multiple instances of significant As an in vivo cancer unit, we grow human tumors in immunodeficient incongruencies between approved protocols and surgical records mice such as CD-1 nude, which may require the addition of hormones reviewed, as well as internal protocol contradictions. The most to promote the growth of prostate and breast tumors. Traditionally, the commonly identified issues are postoperative analgesia not being supplement was delivered by subcutaneous slow-release pellets. administered per protocol (for example, 1 of the multimodal analgesics However, due to supply issues with the 5-α-DHT pellets, we had to is missing, dose intervals and quantities not followed), missing develop another way to provide this hormone. -

Chapter 7: Novelty-Suppressed Feeding in the Mouse
Chapter 7 Novelty-Suppressed Feeding in the Mouse Benjamin Adam Samuels and René Hen Abstract The use of hyponeophagia, in which exposure to a novel environment suppresses feeding behavior, has been used to assess anxiety-related behavior in animals for over seven decades. More recent work has shown that variations of hyponeophagia, such as the novelty-suppressed feeding test, have become effective paradigms for testing treatment with drugs such as anxiolytics and antidepressants. Most interestingly, unlike many other behavioral paradigms, novelty-suppressed feeding is sensitive to chronic, but not acute, antidepressant treatment, which mirrors the effects of antidepressant treatment in human patients. Here we provide a brief historical overview of novelty-suppressed feeding and provide a protocol for running the test with mice. Key words: Anxiety, Depression, Mood, Mouse, Antidepressant, Neurogenesis 1. Background and Historical Overview Novelty-suppressed feeding (hyponeophagia) is a conflict-based test in which an animal that has been deprived of food for a full day faces a choice of approaching and consuming a piece of food in the center of a brightly lit, novel open arena or staying to the side and avoiding the center of this anxiogenic environment. Subjects par- ticipating in this test do not require any previous complex training, are not exposed to painful stimuli, and are usually deprived of food for 24 h, less than an animal would face in a normal foraging situ- ation. The main measure of the test is latency to eat (defined as the amount of time it takes for the animal to enter the center of the arena and bite the food pellet with use of forepaws while sitting on its haunches).