Eye on Cataract™
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Visual Outcomes of Combined Cataract Surgery and Minimally Invasive Glaucoma Surgery
1422 REVIEW/UPDATE Visual outcomes of combined cataract surgery and minimally invasive glaucoma surgery Steven R. Sarkisian Jr, MD, Nathan Radcliffe, MD, Paul Harasymowycz, MD, Steven Vold, MD, Thomas Patrianakos, MD, Amy Zhang, MD, Leon Herndon, MD, Jacob Brubaker, MD, Marlene Moster, MD, Brian Francis, MD, for the ASCRS Glaucoma Clinical Committee Minimally invasive glaucoma surgery (MIGS) has become a reliable on visual outcomes based on the literature and the experience of standard of care for the treatment of glaucoma when combined the ASCRS Glaucoma Clinical Committee. with cataract surgery. This review describes the MIGS procedures J Cataract Refract Surg 2020; 46:1422–1432 Copyright © 2020 Published currently combined with and without cataract surgery with a focus by Wolters Kluwer on behalf of ASCRS and ESCRS inimally invasive (sometimes referred to as mi- and thereby lower IOP. The endoscope consists of a fiber- croinvasive) glaucoma surgery (MIGS) is a pro- optic camera, light source, and laser aiming beam with an Mcedure that lowers intraocular pressure (IOP) 832 nm diode laser. The endoscope probe is introduced into without significantly altering the tissue, allows for rapid the globe via a limbal corneal or pars plana incision. The visual recovery, is moderately effective, and can be com- anterior approach requires inflation of the ciliary sulcus with bined with cataract surgery in a safe and efficient manner.1,2 an ophthalmic viscosurgical device, whereas the posterior This is in contrast to more conventional glaucoma surgery approach uses a pars plana or anterior chamber irrigation (eg, trabeculectomy or large glaucoma drainage device port. Although the anterior approach can be used in a phakic implantation), which requires conjunctival and scleral eye, it is typically performed with cataract extraction as a incisions as well as suturing. -

Ocular Surface Disease: Supplement April 2018 Accurately Diagnose & Effectively Treat Your Surgical Patients
Ocular Surface Disease: Supplement April 2018 Accurately Diagnose & Effectively Treat Your Surgical Patients Supported by an unrestricted educational grant from Ocular Surface Disease: Accurately Diagnose & Effectively Treat Your Surgical Patients Prevalence of Ocular Surface Disease and Its Impact on Surgical Outcomes Accurate diagnosis of dry eye disease is critical before cataract or refractive surgery By Elisabeth M. Messmer, MD ry eye is a common disease, but it may remain EPIDEMIOLOGY OF DRY EYE SYNDROME undetected. If it is not treated before cataract or 1-4 refractive surgery, patients may have suboptimal visual AFTER CATARACT SURGERY outcomes from their procedures. D l Very limited data available, mostly small descriptive/ IMPACT ON CATARACT SURGERY non-randomised studies There are a number of triggering factors for dry eye (Figure 1). l 10-20% of patients: DED induced or worsened after Cataract surgery worsens or causes dry eye in approximately uncomplicated cataract surgery 10% to 20% of patients (Figure 2).1-4 l In all studies: Signs and symptoms of dry eye In a study of 136 patients with a mean age of 71 years who increase after surgery were having cataract surgery, 22% had a prior diagnosis of dry eye that was not treated.5 Thirty-one percent complained l In most studies: gradual improvement of signs and of stinging, burning or other symptoms of dry eye when asked symptoms of dry eye within 3 months about their symptoms, and 41% reported a foreign body l In some studies: signs and symptoms persist > 3 months sensation. When the patients were examined, 77% had corneal staining and 50% had central staining. -
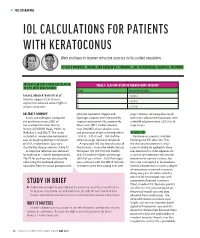
Iol Calculations for Patients with Keratoconus
s THE LITERATURE IOL CALCULATIONS FOR PATIENTS WITH KERATOCONUS Work continues to improve refractive accuracy in this patient population. BY ALICE ROTHWELL, MBCHB, AND ANDREW M.J. TURNBULL, BM, PGCERTMEDED, PGDIPCRS, FRCOPHTH INTRAOCULAR LENS POWER CALCULATION TABLE 1. CLASSIFICATION OF KERATOCONUS SEVERITY IN EYES WITH KERATOCONUS Stage Keratometry Reading Savini G, Abbate R, Hoffer KJ, et al1 1 ≤ 48.00 D Industry support: K.J.H. licenses 2 > 48.00 D registered trademark name Hoffer to various companies 3 > 53.00 D ABSTRACT SUMMARY spherical equivalent. Myopic and stage 1 disease. Accuracy decreased Savini and colleagues compared hyperopic surprises were indicated by with more advanced keratoconus, with the prediction errors (PEs) of negative and positive PEs, respectively. a MedAE of greater than 2.50 D in all five standard formulas: Barrett Mean error (ME), median absolute stage 3 eyes. Universal II (BUII), Haigis, Hoffer Q, error (MedAE), mean absolute error, Holladay 1, and SRK/T. The study and percentage of eyes achieving within DISCUSSION included 41 consecutive keratoconic ±0.50 D, ±0.75 D, and ±1.00 D of the Keratoconus presents multiple eyes undergoing phacoemulsification refractive target were also calculated. challenges to IOL selection. First, and IOL implantation. Eyes were A hyperopic ME was found across all the standard keratometric index classified by disease severity (Table 1). five formulas. Across the whole dataset, cannot reliably be applied to these A subjective refraction was obtained the lowest ME (0.91 D) and MedAE eyes because this index depends on for each eye at 1 month postoperatively. (0.62 D) and the highest percentage a normal ratio between the anterior The PE for each eye was calculated by (36%) of eyes within ±0.50 D of target and posterior corneal surfaces, but subtracting the predicted spherical were achieved with the SRK/T formula. -

Analysis of Human Corneal Igg by Isoelectric Focusing
Investigative Ophthalmology & Visual Science, Vol. 29, No. 10, October 1988 Copyright © Association for Research in Vision and Ophthalmology Analysis of Human Corneal IgG by Isoelectric Focusing J. Clifford Woldrep,* Robin L. Noe,f and R. Doyle Stulringf Parameters which regulate the localization and retention of IgG within the corneal stroma are complex and poorly understood. Although multiple factors are involved, electrostatic interactions between IgG and anionic corneal tissue components, ie, proteoglycans (PG) and glycosaminoglycans (GAG) may regulate the distribution of antibodies within the corneal stroma. Isoelectric focusing (IEF) and blotting analysis of IgG revealed a restricted pi profile for both central and peripheral regions of the normal cornea. Similar analysis of pathological corneas from keratoplasty specimens in Fuchs' dys- trophy and keratoconus reveal a variable IEF profile. In the majority of keratoplasty specimens from patients with corneal edema or graft rejection, there was generally little or no IgG detectable. These results suggest that in edematous corneas where there is altered PG/GAG in the stroma and modified fluid dynamics, there is a concomitant loss of IgG. These findings may have implications for immuno- logic surveillance and protection of the avascular cornea. Invest Ophthalmol Vis Sci 29:1538-1543, 1988 The humoral immune system plays an important the soluble plasma proteins through ionic interac- role in mediating immunologic surveillance and pro- tions. The PGs and GAGs have long been known to -
Management Modalities for Keratoconus an Overview of Noninterventional and Interventional Treatments
REFRACTIVE SURGERY FEATURE STORY EXCLUSIVE ONLINE CONTENT AVAILABLE Management Modalities for Keratoconus An overview of noninterventional and interventional treatments. BY MAZEN M. SINJAB, MD, PHD anagement of keratoconus has advanced TAKE-HOME MESSAGE during the past few years, and surgeons can • When evaluating patients with keratoconus, ask now choose among numerous traditional and them to stop using RGP contact lenses at least 2 modern treatments. Traditional modalities weeks before evaluation to achieve correct Msuch as spectacle correction, contact lenses, penetrating measurement of the corneal shape. keratoplasty (PKP), and conductive keratoplasty (CK) • Interventional management modalities include CK, are still effective; however, demand for the last two has PKP, DALK, ICRSs, CXL, phakic IOLs, or some decreased with the advent of modern alternatives, specifi- combination of these treatments. cally intrastromal corneal ring segments (ICRSs) and cor- • Making the right management decision depends neal collagen crosslinking (CXL). Caution should be used on the patient’s corneal transparency and stress when considering these newer treatment modalities, and lines, age, progression, contact lens tolerance, surgeons should be aware of their indications, contraindi- refractive error, UCVA and BCVA, K-max, corneal cations, conditions, and complications before proceeding thickness, and sex. with treatment. Keratoconus treatments can be divided into two cate- Some patients achieve good vision correction and comfort gories, interventional and noninterventional. In this article, with this strategy. particular attention is given to ICRSs and CXL, as they are Advances in lens designs and materials have increased the the most popular emerging interventional management proportion of keratoconus patients who can be fitted with modalities for keratoconus. -

CAUSES, COMPLICATIONS &TREATMENT of A“RED EYE”
CAUSES, COMPLICATIONS & TREATMENT of a “RED EYE” 8 Most cases of “red eye” seen in general practice are likely to be conjunctivitis or a superficial corneal injury, however, red eye can also indicate a serious eye condition such as acute angle glaucoma, iritis, keratitis or scleritis. Features such as significant pain, photophobia, reduced visual acuity and a unilateral presentation are “red flags” that a sight-threatening condition may be present. In the absence of specialised eye examination equipment, such as a slit lamp, General Practitioners must rely on identifying these key features to know which patients require referral to an Ophthalmologist for further assessment. Is it conjunctivitis or is it something more Iritis is also known as anterior uveitis; posterior uveitis is serious? inflammation of the choroid (choroiditis). Complications include glaucoma, cataract and macular oedema. The most likely cause of a red eye in patients who present to 4. Scleritis is inflammation of the sclera. This is a very rare general practice is conjunctivitis. However, red eye can also be presentation, usually associated with autoimmune a feature of a more serious eye condition, in which a delay in disease, e.g. rheumatoid arthritis. treatment due to a missed diagnosis can result in permanent 5. Penetrating eye injury or embedded foreign body; red visual loss. In addition, the inappropriate use of antibacterial eye is not always a feature topical eye preparations contributes to antimicrobial 6. Acid or alkali burn to the eye resistance. The patient history will usually identify a penetrating eye injury Most general practice clinics will not have access to specialised or chemical burn to the eye, but further assessment may be equipment for eye examination, e.g. -

Scleral Lenses and Eye Health
Scleral Lenses and Eye Health Anatomy and Function of the Human Eye How Scleral Lenses Interact with the Ocular Surface Just as the skin protects the human body, the ocular surface protects the human Scleral lenses are large-diameter lenses designed to vault the cornea and rest on the conjunctival tissue sitting on eye. The ocular surface is made up of the cornea, the conjunctiva, the tear film, top of the sclera. The space between the back surface of the lens and the cornea acts as a fluid reservoir. Scleral and the glands that produce tears, oils, and mucus in the tear film. lenses can range in size from 13mm to 19mm, although larger diameter lenses may be designed for patients with more severe eye conditions. Due to their size, scleral lenses consist SCLERA: The sclera is the white outer wall of the eye. It is SCLERAL LENS made of collagen fibers that are arranged for strength rather of at least two zones: than transmission of light. OPTIC ZONE The optic zone vaults over the cornea CORNEA: The cornea is the front center portion of the outer Cross section of FLUID RESERVOIR wall of the eye. It is made of collagen fibers that are arranged in the eye shows The haptic zone rests on the conjunctiva such a way so that the cornea is clear. The cornea bends light the cornea, overlying the sclera as it enters the eye so that the light is focused on the retina. conjunctiva, and sclera as CORNEA The cornea has a protective surface layer called the epithelium. -

Association Between Visual Field Damage and Corneal Structural
www.nature.com/scientificreports OPEN Association between visual feld damage and corneal structural parameters Alexandru Lavric1*, Valentin Popa1, Hidenori Takahashi2, Rossen M. Hazarbassanov3 & Siamak Yousef4,5 The main goal of this study is to identify the association between corneal shape, elevation, and thickness parameters and visual feld damage using machine learning. A total of 676 eyes from 568 patients from the Jichi Medical University in Japan were included in this study. Corneal topography, pachymetry, and elevation images were obtained using anterior segment optical coherence tomography (OCT) and visual feld tests were collected using standard automated perimetry with 24-2 Swedish Interactive Threshold Algorithm. The association between corneal structural parameters and visual feld damage was investigated using machine learning and evaluated through tenfold cross-validation of the area under the receiver operating characteristic curves (AUC). The average mean deviation was − 8.0 dB and the average central corneal thickness (CCT) was 513.1 µm. Using ensemble machine learning bagged trees classifers, we detected visual feld abnormality from corneal parameters with an AUC of 0.83. Using a tree-based machine learning classifer, we detected four visual feld severity levels from corneal parameters with an AUC of 0.74. Although CCT and corneal hysteresis have long been accepted as predictors of glaucoma development and future visual feld loss, corneal shape and elevation parameters may also predict glaucoma-induced visual functional loss. While intraocular pressure (IOP), age, disc hemorrhage, and optic cup characteristics have been long identifed as classic risk factors for development of primary open-angle glaucoma (POAG)1,2, the Ocular Hypertension Treatment Study (OHTS) suggested central corneal thickness (CCT) as a new risk factor for development of POAG3. -

Contacts Vs. Iols for Congenital Cataract
in Review News commentary and perspectives Contacts vs. IOLs for Congenital Cataract he verdict is in on the issue of optical correction in children who undergo unilateral cataract surgery before age 7 months: Aphakia, corrected with a contact lens, is a better option than an T CONTACT LENS PATIENT. Dr. Lambert examines a 6-year-old intraocular lens (IOL) for 55 others who received an aphakic girl in the IATS trial. This child was prescribed a most of these babies. IOL implant (median VA in contact lens in one eye at 1 month of age and could insert “Primary IOL implan- both groups, 0.90 logMAR her own contact lens by the age 4 years. tation should be reserved [20/159]). for those infants where, in More complications. pillary membranes occurred one normal eye. But the the opinion of the surgeon, However, a significantly 10 times more often in the thing about children is that the cost and handling of greater number of the pseu- pseudophakic eyes. they’re going to live for a a contact lens would be so dophakic eyes required one Scott R. Lambert, MD, very long time, and it is burdensome as to result in or more additional intra- a professor of ophthalmol- important for them to have significant periods of uncor- operative procedures over ogy at Emory University in the best possible visual acu- rected aphakia,” stated the the course of the study (41 Atlanta and the lead inves- ity in their problem eye,” investigators in the Infant patients compared with tigator in the trial, credited he said, particularly in case Aphakia Treatment Study.1 12 in the aphakic group; advocacy by the pediatric anything should happen to Comparable VA. -

Treatment of Stable Keratoconus by Cataract Surgery with Toric IOL Implantation
10.5005/jp-journals-10025-1024 JaimeCASE Levy REPORT et al Treatment of Stable Keratoconus by Cataract Surgery with Toric IOL Implantation Jaime Levy, Anry Pitchkhadze, Tova Lifshitz ABSTRACT implantation in the right eye. On presentation, uncorrected We present the case of a 73-year-old patient who underwent visual acuity (UCVA) was 6/60 OU. Refraction was –0.75 successful phacoemulsification and toric intraocular lens (IOL) –5.0 × 65° OD and –3.25 –4.0 × 98° OS. Nuclear sclerosis implantation to correct high stable astigmatism due to and posterior subcapsular cataract +2 was observed in the keratoconus and cataract. Preoperative refraction was –3.25 – left eye. The posterior segments were unremarkable. 4.0 × 98°. A toric IOL (Acrysof SN60T6) with a spherical power of 16.5 D and a cylinder power of 3.75 D at the IOL plane and Corneal topography performed with Orbscan (Bausch 2.57 D at the corneal plane was implanted and aligned at an and Lomb, Rochester, NY) showed central thinning of 457 axis of 0°. Uncorrected visual acuity improved from 6/60 to microns and positive islands of elevation typical for 6/10. Postoperative best corrected visual acuity was 6/6, 6 months after the operation. In conclusion, phacoemulsification keratoconus in the right eye (Fig. 1). In the left eye a less with toric IOL implantation can be performed in eyes with pronounced inferior cone was observed (Fig. 2), without keratoconus and cataract. any area of significant thinning near the limbus typical for Keywords: Intraocular lens, Toric IOL, Keratoconus, Cataract pellucid marginal degeneration.2 Keratometry (K)-values surgery. -

Distribution of Anterior and Posterior Corneal Astigmatism in Eyes with Keratoconus
Distribution of Anterior and Posterior Corneal Astigmatism in Eyes With Keratoconus MOHAMMAD NADERAN, MOHAMMAD TAHER RAJABI, AND PARVIZ ZARRINBAKHSH PURPOSE: To investigate the magnitude, with-the-rule ERATOCONUS (KC) IS A PROGRESSIVE, USUALLY (WTR) or against-the-rule (ATR) orientation, and vec- bilateral ectatic corneal disorder, characterized by 1,2 tor components (Jackson astigmatic vectors [J0 and J45] K corneal thinning and protrusion. KC starts at and blurring strength) of the anterior and posterior puberty and progresses to the third or fourth decade of corneal astigmatism (ACA and PCA) in patients with life, causing myopia and astigmatism, which results in keratoconus (KC) in a retrospective study, and to try to severe vision distortion and sometimes even blindness.1 find suitable cutoff points for ACA and PCA in an Astigmatism is a refractive error that is mostly caused by attempt to discriminate KC from normal corneas. toricity of the anterior corneal surface leading to visually DESIGN: Retrospective age- and sex-matched case- significant optical aberration. Both the anterior and poste- control study. rior corneal surfaces contribute to the total corneal METHODS: Using the Pentacam images, the aforemen- astigmatism. Recently, the direct and quantitative mea- tioned parameters were compared between 1273 patients surement of the posterior corneal measurements in a with KC and 1035 normal participants. clinical setting has been possible with new imaging tech- RESULTS: The mean magnitude of the ACA and PCA nologies such as slit-scanning, Scheimpflug, or optical was 4.49 ± 2.16 diopter (D) and 0.90 ± 0.43 D, respec- coherence devices.3,4 tively. The dominant astigmatism orientation of the Assessment of the corneal astigmatism plays an impor- ACA was ATR in KC patients and WTR in normal par- tant role in vision correction procedures such as rigid gas- ticipants (P < .001), while for the PCA it was WTR in permeable lens prescription or intraocular lens (IOL) im- KC patients and ATR in normal participants (P < .001). -

Corneal Cross-Linking in Infectious Keratitis David Tabibian1,5*, Cosimo Mazzotta2 and Farhad Hafezi1,3,4
Tabibian et al. Eye and Vision (2016) 3:11 DOI 10.1186/s40662-016-0042-x REVIEW Open Access PACK-CXL: Corneal cross-linking in infectious keratitis David Tabibian1,5*, Cosimo Mazzotta2 and Farhad Hafezi1,3,4 Abstract Background: Corneal cross-linking (CXL) using ultraviolet light-A (UV-A) and riboflavin is a technique developed in the 1990’s to treat corneal ectatic disorders such as keratoconus. It soon became the new gold standard in multiple countries around the world to halt the progression of this disorder, with good long-term outcomes in keratometry reading and visual acuity. The original Dresden treatment protocol was also later on used to stabilize iatrogenic corneal ectasia appearing after laser-assisted in situ keratomileusis (LASIK) and photorefractive keratectomy (PRK). CXL efficiently strengthened the cornea but was also shown to kill most of the keratocytes within the corneal stroma, later on repopulated by those cells. Review: Ultraviolet-light has long been known for its microbicidal effect, and thus CXL postulated to be able to sterilize the cornea from infectious pathogens. This cytotoxic effect led to the first clinical trials using CXL to treat advanced infectious melting corneal keratitis. Patients treated with this technique showed, in the majority of cases, a stabilization of the melting process and were able to avoid emergent à chaud keratoplasty. Following those primary favorable results, CXL was used to treat beginning bacterial keratitis as a first-line treatment without any adjunctive antibiotics with positive results for most patients. In order to distinguish the use of CXL for infectious keratitis treatment from its use for corneal ectatic disorders, a new term was proposed at the 9th CXL congress in Dublin to rename its use in infections as photoactivated chromophore for infectious keratitis -corneal collagen cross-linking (PACK-CXL).