Download Preprint
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

VEEP Episode #410 “Election Night” Teleplay By
VEEP Episode #410 “Election Night” Teleplay by: Simon Blackwell & Tony Roche Story by: Armando Iannucci, Simon Blackwell & Tony Roche AS BROADCAST SCRIPT May 26, 2015 VEEP As Broadcast Script Episode #410 01:00:17 [HBO ENTERTAINMENT OPENING LOGO] INT. HOTEL SUITE BEDROOM – NIGHT. President Meyer is sitting on the edge of the bed staring out the window. Kent knocks as he enters. KENT East coast polls are closing, ma’am. Tom knocks as he enters. TOM Ma’am? History’s calling, and it won’t go to voicemail. Gary knocks as he enters. GARY Hey. You okay, ma’am? PRESIDENT MEYER Oh, I’d love one, Gary. Thank you. GARY Okay, I’ll get, I’ll get you one. PRESIDENT MEYER Well, I’ve asked America if she wants me to be her president. Now she’s gonna give us her answer. (clears throat) GARY America doesn’t just love you, ma’am, she is in love with you. (chuckles) PRESIDENT MEYER (chuckles) Daily Transcription 1 5/26/2015 VEEP EPISODE #410 MIKE (OS) We’ve lost Kentucky! 01:00:53 [MUSIC IN] [OPENING SEQUENCE] EXT. TV STUDIO – NIGHT. Establishing shot. Election Night 7:15 pm DAN (VO) I assume you reached out to... INT. TV STUDIO HAIR AND MAKE-UP ROOM – NIGHT. Dan and Amy are seated at dressing mirrors. DAN ...the O’Brien camp. You taking a meeting with Charlotte or with Kim? AMY No, I, I haven’t contacted the O’Brien team. DAN Amy, if he wins, our lobbying stock is gonna droop like a chimp’s tits. -

Saluting Service and Sacrifice
MOVIES: Bill & Ted return as MLB middle-aged dads Page 21 Hall of Famer Tom Seaver, heart and soul of the ’69 MUSIC: The Killers ‘Miracle Mets,’ dies at 75 still exploring Page 32 Back page TRAVEL: DIY cruises keep dreams afloat Page 28 stripes.com Volume 79, No. 100 ©SS 2020 FRIDAY, SEPTEMBER 4, 2020 $1.00 PACIFIC U.S. ARMY/AP Sgt. Maj. Thomas Payne, shown as a sergeant first class in 2012, will receive the Medal of Honor for his actions during a daring 2015 raid that rescued 70 hostages set to be executed by Islamic State militants. Soldier will get Medal of Honor for Iraq rescue Saluting BY JAMES LAPORTA Associated Press DELRAY BEACH, Fla. — An American soldier who helped res- service and cue about 70 hostages set to be executed by Islamic State mili- tants in Iraq has been approved to receive the Medal of Honor for actions during a daring 2015 raid, The Associated Press has learned. sacrifice Sgt. Maj. Thomas “Patrick” Payne, a Ranger assigned to the U.S. Army’s Special Operations Command, will receive the U.S. military’s highest honor for valor in combat in a White House cer- Scaled-down ceremony marking 75th anniversary of WWII’s emony set to be held on the 19th anniversary of the Sept. 11, 2001 terrorist attacks. end reflects on a generation’s toil to turn ‘peril into peace’ The medal approval was con- firmed by two Defense Depart- BY WYATT OLSON U.S. sailors aboard On Wednesday, only a dozen veterans of the ment officials who spoke on Stars and Stripes the USS Michael war were on the fantail of that ship in Pearl condition of anonymity because Murphy stand at Harbor, Hawaii, to witness a commemoration HONOLULU — Seventy-five years ago, they weren’t authorized to speak attention while marking the 75th anniversary of the war’s 900 bombers and fighters filled the sky above passing the Battleship on the record. -

Netflix and the Development of the Internet Television Network
Syracuse University SURFACE Dissertations - ALL SURFACE May 2016 Netflix and the Development of the Internet Television Network Laura Osur Syracuse University Follow this and additional works at: https://surface.syr.edu/etd Part of the Social and Behavioral Sciences Commons Recommended Citation Osur, Laura, "Netflix and the Development of the Internet Television Network" (2016). Dissertations - ALL. 448. https://surface.syr.edu/etd/448 This Dissertation is brought to you for free and open access by the SURFACE at SURFACE. It has been accepted for inclusion in Dissertations - ALL by an authorized administrator of SURFACE. For more information, please contact [email protected]. Abstract When Netflix launched in April 1998, Internet video was in its infancy. Eighteen years later, Netflix has developed into the first truly global Internet TV network. Many books have been written about the five broadcast networks – NBC, CBS, ABC, Fox, and the CW – and many about the major cable networks – HBO, CNN, MTV, Nickelodeon, just to name a few – and this is the fitting time to undertake a detailed analysis of how Netflix, as the preeminent Internet TV networks, has come to be. This book, then, combines historical, industrial, and textual analysis to investigate, contextualize, and historicize Netflix's development as an Internet TV network. The book is split into four chapters. The first explores the ways in which Netflix's development during its early years a DVD-by-mail company – 1998-2007, a period I am calling "Netflix as Rental Company" – lay the foundations for the company's future iterations and successes. During this period, Netflix adapted DVD distribution to the Internet, revolutionizing the way viewers receive, watch, and choose content, and built a brand reputation on consumer-centric innovation. -

Repartitie Aferenta Trimestrului I - 2019 - Straini DACIN SARA
Repartitie aferenta trimestrului I - 2019 - straini DACIN SARA TITLU TITLU ORIGINAL AN TARA R1 R2 R3 R4 R5 R6 R7 R8 S1 S2 S3 S4 S5 S6 S7 S8 13 13 2010 US Gela Babluani Gela Babluani Greg Pruss - Gregory Pruss Roland Emmerich - VG Roland Emmerich - VG 2012 2012 2009 US BILD KUNST Harald Kloser BILD KUNST 007: Coordonata Skyfall Skyfall 2012 GB/US Sam Mendes - ALCS Neal Purvis - ALCS Robert Wade - ALCS John Logan - ALCS 007: partea lui de consolare Quantum of Solace 2008 GB/US Marc Forster Neal Purvis - ALCS Robert Wade - ALCS Paul Haggis - ALCS 007: Viitorul e in mainile lui - 007 si Imperiul zilei de maine Tomorrow Never Dies 1997 GB/US Roger Spottiswoode Bruce Feirstein - ALCS Roland Emmerich - VG Roland Emmerich - VG 10 000 HR 10 000 BC 2008 US BILD KUNST Harlad Kloser BILD KUNST 1000 post Terra After Earth 2013 US M. Night Shyamalan Gary Whitta M. Night Shyamalan Binbir Gece - season 1, episode 1001 de nopti (ep.001) 1 2006 TR Kudret Sabanci - SETEM Yildiz Tunc Murat Lutfu Mehmet Bilal Ethem Yekta Binbir Gece - season 1, episode 1001 de nopti (ep.002) 2 2006 TR Kudret Sabanci - SETEM Yildiz Tunc Murat Lutfu Mehmet Bilal Ethem Yekta Binbir Gece - season 1, episode 1001 de nopti (ep.003) 3 2006 TR Kudret Sabanci - SETEM Yildiz Tunc Murat Lutfu Mehmet Bilal Ethem Yekta Binbir Gece - season 1, episode 1001 de nopti (ep.004) 4 2006 TR Kudret Sabanci - SETEM Yildiz Tunc Murat Lutfu Mehmet Bilal Ethem Yekta Binbir Gece - season 1, episode 1001 de nopti (ep.005) 5 2006 TR Kudret Sabanci - SETEM Yildiz Tunc Murat Lutfu Mehmet Bilal Ethem Yekta -

BEST PICTURE O up Director Actor in a Leading Role ACTRESS in a Leading Role Actor in a Supporting Role ACTRESS in a Supporting
Up–to–the–minute Oscar news and wrap-up on vulture.com 2010 OSCAR PooL BALLOT BEST PICTURE FOreiGN LANGuaGE FilM DOcuMENtarY Feature Avatar Ajami Burma VJ Anders Østergaard and Lise Lense-Møller The Blind Side Israel | Directed by Scandar Copti and Yaron Shani The Cove Louie Psihoyos and Fisher Stevens District 9 The Milk of Sorrow (La Teta Asustada) Food, Inc. Robert Kenner and Elise Pearlstein Peru | Directed by Claudia Llosa An Education The Most Dangerous Man in America: A Prophet (Un Prophète) The Hurt Locker Daniel Ellsberg and the Pentagon Papers France | Directed by Jacques Audiard Judith Ehrlich and Rick Goldsmith Inglourious Basterds The Secret in Their Eyes (El Secreto de Sus Ojos) Which Way Home Rebecca Cammisa Precious Argentina | Directed by Juan José Campanella A Serious Man The White Ribbon (Das Weisse Band) DOcuMENtarY SHOrt SubJect Up Germany | Directed by Michael Haneke China’s Unnatural Disaster: The Tears of Up in the Air Sichuan Province Jon Alpert and Matthew O’Neill OriGINal SCOre The Last Campaign of Governor Booth Gardner DirectOR Avatar James Horner Daniel Junge and Henry Ansbacher James Cameron Avatar Fantastic Mr. Fox Alexandre Desplat The Last Truck: Closing of a GM Plant Kathryn Bigelow The Hurt Locker The Hurt Locker Marco Beltrami and Buck Sanders Steven Bognar and Julia Reichert Quentin Tarantino Inglourious Basterds Sherlock Holmes Hans Zimmer Music by Prudence Roger Ross Williams and Lee Daniels Precious Up Michael Giacchino Elinor Burkett Jason Reitman Up in the Air Rabbit à la Berlin Bartek Konopka and Anna Wydra OriGINal SONG ActOR IN A LeadiNG ROle The Princess and the Frog “Almost There” ANIMated SHOrt FilM Jeff Bridges Crazy Heart Music and Lyric by Randy Newman French Roast Fabrice O. -
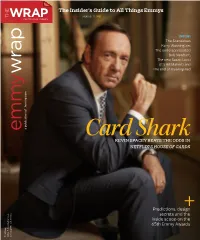
The Insider's Guide to All Things Emmys
The Insider’s Guide to All Things Emmys DOWN TO THE WIRE | AUGUST 12, 2013 COVERING HOLLYWOOD INSIDE: The Scandalous Kerry Washington, The underappreciated Bob Newhart, The new Susan Lucci (it's Bill Maher!) and The end of Breaking Bad a publication of thewrap.com of a publication Card Shark KEVIN SPACEY BEATS THE ODDS IN NETFLIX'S HOUSE OF CARDS Predictions, design+ secrets and the inside scoop on the 65th Emmy Awards TheWrap 2855 S. Barrington Ave. Los Angeles, CA 90064 CONGRATULATIONS TO ALL OUR 110 NOMINATIONS! 2013 PRIMETIME EMMY ® N O M I N E E S ! BEHIND THE CANDELABRA PHIL SPECTOR GAME OF THRONES® BOARDWALK EMPIRE® GIRLSSM REAL TIME WITH MEA MAXIMA CULPA: CROSSFIRE HURRICANE Jerry Weintraub Productions in association with Levinson/Fontana Productions in association with Bighead, Littlehead, Television 360, Startling Leverage, Closest to the Hole Productions, Apatow Productions and I am Jenni Konner BILL MAHER SILENCE IN THE Tremolo Productions, Milkwood Films, Eagle ® ® HBO Films HBO Films Television and Generator Productions in association Sikelia Productions and Cold Front Productions Productions in association with HBO Entertainment Bill Maher Productions and Brad Grey Television HOUSE OF GOD Rock Entertainment and the Rolling Stones in ® with HBO Entertainment in association with HBO Entertainment ® association with HBO Documentary Films OUTSTANDING MINISERIES OR MOVIE OUTSTANDING MINISERIES OR MOVIE OUTSTANDING COMEDY SERIES in association with HBO Entertainment HBO Documentary Films in association with Jerry Weintraub, Executive Producer; Barry Levinson, David Mamet, Executive Producers; OUTSTANDING DRAMA SERIES SUPPORTING ACTOR IN A DRAMA SERIES Judd Apatow, Jenni Konner, Lena Dunham, OUTSTANDING VARIETY SERIES Jigsaw Productions, Wider Film Projects and OUTSTANDING DOCUMENTARY OR NONFICTION Gregory Jacobs, Susan Ekins, Michael Polaire, Michael Hausman, Produced by David Benio , D.B. -

Star Channels, March 21
staradvertiser.com MARCH 21 - 27, 2021 FAMILY MATTERS Now that the kids are a bit older, Paul (Martin Freeman) and Ally (Daisy Haggard) face new parenting challenges in Season 2 of Breeders. This season, 13-year-old Luke (Alex Eastwood) struggles with increasing anxiety, while 10-year-old Ava (Eve Prenelle) is growing more independent. Premiering Monday, March 22, on FX. Enjoy original songs performed by up and coming local artists. Hosted by Jake ShimabukuroZg]Ûef^]Zm¶ũe^ehl Mele A‘e new soundstage, Studio 1122. A SHOWCASE FOR HAWAI¶I’S SUNDAY, MARCH 28, 7PM olelo.org olelo.org ASPIRING ARTISTS CHANNEL 53 | olelo.org/53 590242_MeleAePremiere_2_withJake_F.indd 1 3/3/21 3:19 PM ON THE COVER | BREEDERS Father doesn’t know best Martin Freeman’s of the show’s creators. The actor claims he had about “the parental paradox that you’d happily been inspired to create the show after having die for your children but quite often also want to ‘Breeders’ returns to FX a dream about yelling at his children. He ex- kill them.” In the first season, Paul and Ally dealt plained the premise in an interview with Variety with the very real pressures of modern-day par- By Kyla Brewer when the first season of “Breeders” premiered enting while trying to stay connected romanti- TV Media in March 2020. cally, work full time and maintain their sanity, “It doesn’t tip over into being actually trau- which, as just about any parent can attest, is no n the early days of television, TV dads always matic, but it should ring bells as far as the small feat. -
Stockport's Super Cinema and Variety Theatre
SPRING/ SUMMER 2020 Stockport’s Super Cinema and Variety Theatre MERSEY SQUARE BOX OFFICE: 0161 477 7779 STOCKPORT GROUP BOOKINGS: 0843 208 1495 CHESHIRE. SK1 1SP WWW.STOCKPORTPLAZA.CO.UK TED DOAN General Manager On October 7th 1932 a vision was born in Stockport as the doors opened on a sumptuous Art Deco Super Cinema and Variety Theatre that would shine as the regional home for the very best in Big Screen and Live Stage Entertainment, Events and Fine Dining here in the very heart of Stockport and almost 90 years later we raise the curtain on yet another season featuring the very best in every style of event for you, your family and friends to enjoy. From cinematic presentations of the greatest silver screen offerings of classic, modern and satellite broadcasts through to a sensational mix of the very best in live entertainment in our main auditorium and the intimate Green Room performance lounge, I believe we definitely have something for everybody in this brochure that you are holding today. As well as being your perfect entertainment venue, the Plaza Café retains its title as ‘The Talk of The North’ with a wonderful menu prepared for you from 10am until 4pm on Mondays to Saturdays offering you the chance to enjoy a delightful indulgence in the very best of art deco surroundings. The Plaza has hosted beautiful weddings, receptions, private events and conferences throughout her years serving her community therefore please do not hesitate to get in touch with me if I can make your special event even more special! From our Festive Pantomime DICK WHITTINGTON starring BRIAN CAPRON with BRADLEY THOMPSON which runs from Friday 4th December 2020 to Sunday 10th January 2021 through our live stage and big screen presentations to our Easter Pantomime MOTHER GOOSE, there is most definitely something for everyone to enjoy this season. -

By Steve Pond
The Insider’s Guide to All Things Emmys EMMY A publication of The Wrap News TheWrap 2855 S. Barrington Ave. Los Angeles, CA 90064 BACK COVER FRONT COVER INSIDE FRONT COVER INSIDE BACK COVER The Insider’s Guide to All Things Emmys DOWN TO THE WIRE | JULY 28, 2014 EMMYA publication of The Wrap News Shane Smith: The Vice Founder Chats About Reinventing TV Journalism Tim Molloy’s Predictions: Who Will Win, Who Should Win Steve Pond’s Burning Questions About Emmy's Future Backstage Confidential: Politics, Pranks and Personalities at the Telecast A Golden Year The Emmys Salute a Classic Time for Great Television Plus: Kerry Washington, James Cameron, Colin Hanks, Minnie Driver and the Wide World of TV, from Silicon Valley to Downton Abbey TheWrap 2855 S. Barrington Ave. Los Angeles, CA 90064 CONGRAT ULATIONS CONGRATULATIO® TO ALL OUR 2014 PRIME TIME EMMY N O M I N E E S ! ® OUTSTANDING SOUND EDITING FOR A SERIES OUTSTANDING LEAD ACTRESS IN A COMEDY SERIES OUTSTANDING COSTUMES FOR A SERIES SARAH SILVERMAN: THE NORMAL HEART TREME Tim Kimmel, Supervising Sound Editor; Jed M. Dodge, Julia Louis-Dreyfus as Vice President Selina Meyer John Dunn, Lisa Padovani, Costume Designers; HBO Films® in association with Plan B Entertainment, HBO Entertainment in association with Supervising Dialogue Editor; Tim Hands, Supervising ADR Editor; Joseph La Corte, Costume Supervisor; “New York Sour” WE ARE MIRACLES OUTSTANDING SUPPORTING ACTRESS IN A COMEDY SERIES Blumhouse and Ryan Murphy Productions Blown Deadline Productions Paula Fairfi eld, Sound Designer; David Klotz, Music Editor; Anna Chlumsky as Amy Brookheimer OUTSTANDING HAIRSTYLING FOR A SINGLE-CAMERA SERIES HBO Entertainment in association with Funny or Die Bradley C. -

Nomination Press Release
Brad Walsh, Executive Producer Outstanding Comedy Series Jeff Morton, Co-Executive Producer The Big Bang Theory • CBS • Chuck Lorre Jeffery Richman, Co-Executive Producer Productions, Inc. in association with Warner Abraham Higginbotham, Co-Executive Producer Bros. Television Cindy Chupack, Co-Executive Producer Chuck Lorre, Executive Producer Chris Smirnoff, Producer Bill Prady, Executive Producer Steven Molaro, Executive Producer 30 Rock • NBC • Broadway Video, Little Dave Goetsch, Co-Executive Producer Stranger, Inc. in association with Universal Television Eric Kaplan, Co-Executive Producer Lorne Michaels, Executive Producer Jim Reynolds, Co-Executive Producer Tina Fey, Executive Producer Peter Chakos, Supervising Producer Robert Carlock, Executive Producer Steve Holland, Supervising Producer Marci Klein, Executive Producer Maria Ferrari, Producer David Miner, Executive Producer Faye Oshima Belyeu, Produced By Jeff Richmond, Executive Producer Curb Your Enthusiasm • HBO • HBO John Riggi, Executive Producer Entertainment Ron Weiner, Co-Executive Producer Larry David, Executive Producer Matt Hubbard, Co-Executive Producer Jeff Garlin, Executive Producer Kay Cannon, Supervising Producer Gavin Polone, Executive Producer Vali Chandrasekaran, Supervising Producer Alec Berg, Executive Producer Josh Siegal, Supervising Producer David Mandel, Executive Producer Dylan Morgan, Supervising Producer Jeff Schaffer, Executive Producer Luke Del Tredici, Supervising Producer Larry Charles, Executive Producer Jerry Kupfer, Producer Tim Gibbons, Executive -

Embargoed Until 8:35Am Pt on July 16, 2015
EMBARGOED UNTIL 8:35AM PT ON JULY 16, 2015 67th EMMY® AWARDS NOMINATIONS For Programs Airing June 1, 2014 – May 31, 2015 Los Angeles, CA, July 16, 2015– Nominations for the 67th Emmy® Awards were announced today by the Television Academy in a ceremony hosted by Television Academy Chairman and CEO Bruce Rosenblum along with Uzo Aduba from the Netflix series Orange Is The New Black and Cat Deeley, the host of FOX’s So You Think You Can Dance. "This was truly a remarkable year in television,” said Rosenblum. “From the 40th Anniversary of Saturday Night Live, to David Letterman’s retirement and the conclusion of Mad Men, television’s creativity, influence and impact continue to grow and have never been stronger. From broadcast, to cable to digital services, our industry is producing more quality television than ever before. Television is the pre-eminent entertainment platform with extraordinarily rich and varied storytelling. The work of our members dominates the cultural discussion and ignites the passion of viewers around the world. All of us at the Academy are proud to be honoring the very best in television.” This year’s Drama and Comedy Series nominees included newcomers as well as returning programs to the Emmy competition: Transparent and UnBreakaBle Kimmy Schmidt in the Outstanding Comedy Series category and Better Call Saul in the Outstanding Drama Series competition. Additionally, Parks And Recreation returns to vie for Outstanding Comedy Series while Homeland is back in the running for Outstanding Drama Series. Orange Is The New Black is nominated for its second consecutive season, but in the drama category, following an Academy- sanctioned switch from last year’s comedy nomination. -

SATURDAY, FEBRUARY 1, 2014 Edison Ballroom 240 West 47Th Street • NYC
The Writers Guild of America, East Presents SATURDAY, FEBRUARY 1, 2014 Edison Ballroom 240 West 47th Street • NYC FEBRUARY 1, 2014 EDISON BALLROOM 1 2 The 66th Annual Writers Guild Awards SATURDAY, FEBRUARY 1, 2014 • EDISON BALLROOM • NEW YORK CITY Officers Lowell Peterson Michael Winship: President Executive Director Jeremy Pikser: Vice President Bob Schneider: Secretary–Treasurer Ruth Gallo Assistant Executive Director Council Members John Auerbach Marsha Seeman Henry Bean Assistant Executive Director Walter Bernstein Sue “Bee” Brown Awards Committee Arthur Daley Bonnie Datt, Chair Bonnie Datt Ann B. Cohen Terry George Gail Lee Gina Gionfriddo John Marshall Susan Kim Allan Neuwirth Jenny Lumet Danielle Paige Patrick Mason Courtney Simon Zhubin Parang Richard Vetere Phil Pilato Bernardo Ruiz Ted Schreiber Dana Weissman Lara Shapiro Director of Programs Courtney Simon Duane Tollison Nancy Hathorne Richard Vetere Events Coordinator Jason Gordon Director of Communications PKPR Red Carpet 3 DRAMA SERIES MAD MEN Written by Matthew Weiner André Jacquemetton Maria Jacquemetton Janet Leahy Semi Chellas Erin Levy Lisa Albert Michael Saltzman Tom Smuts Jonathan Igla Jason Grote Carly Wray CONGRATULATIONS TO OUR WRITERS GUILD AWARDS NOMINEES DRAMA SERIES BREAKING BAD Written by Vince Gilligan Sam Catlin Peter Gould George Mastras Thomas Schnauz Moira Walley-Beckett Gennifer Hutchison EPISODIC DRAMA “BURIED” Written by Thomas Schnauz “CONFESSIONS” Written by Gennifer Hutchison “GRANITE STATE” Written by Peter Gould © 2014 AMC Network Entertainment LLC. All rights reserved. AMC 3752 BRIAN S. Version: BLACK AND WRITERS GUILD OF AMERICA WHITE AD FULL PAGE NO BLEED 150 N/A 4.5"W X 7.5"H REVISED 1/10/14 client and prod special info: # A-004 job#1537F artistBRIAN S.