Quantification of Cells Expressing Mesenchymal Stem Cell Markers in Healthy and Osteoarthritic Synovial Membranes
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Human and Mouse CD Marker Handbook Human and Mouse CD Marker Key Markers - Human Key Markers - Mouse
Welcome to More Choice CD Marker Handbook For more information, please visit: Human bdbiosciences.com/eu/go/humancdmarkers Mouse bdbiosciences.com/eu/go/mousecdmarkers Human and Mouse CD Marker Handbook Human and Mouse CD Marker Key Markers - Human Key Markers - Mouse CD3 CD3 CD (cluster of differentiation) molecules are cell surface markers T Cell CD4 CD4 useful for the identification and characterization of leukocytes. The CD CD8 CD8 nomenclature was developed and is maintained through the HLDA (Human Leukocyte Differentiation Antigens) workshop started in 1982. CD45R/B220 CD19 CD19 The goal is to provide standardization of monoclonal antibodies to B Cell CD20 CD22 (B cell activation marker) human antigens across laboratories. To characterize or “workshop” the antibodies, multiple laboratories carry out blind analyses of antibodies. These results independently validate antibody specificity. CD11c CD11c Dendritic Cell CD123 CD123 While the CD nomenclature has been developed for use with human antigens, it is applied to corresponding mouse antigens as well as antigens from other species. However, the mouse and other species NK Cell CD56 CD335 (NKp46) antibodies are not tested by HLDA. Human CD markers were reviewed by the HLDA. New CD markers Stem Cell/ CD34 CD34 were established at the HLDA9 meeting held in Barcelona in 2010. For Precursor hematopoetic stem cell only hematopoetic stem cell only additional information and CD markers please visit www.hcdm.org. Macrophage/ CD14 CD11b/ Mac-1 Monocyte CD33 Ly-71 (F4/80) CD66b Granulocyte CD66b Gr-1/Ly6G Ly6C CD41 CD41 CD61 (Integrin b3) CD61 Platelet CD9 CD62 CD62P (activated platelets) CD235a CD235a Erythrocyte Ter-119 CD146 MECA-32 CD106 CD146 Endothelial Cell CD31 CD62E (activated endothelial cells) Epithelial Cell CD236 CD326 (EPCAM1) For Research Use Only. -

CD90 Expression Controls Migration and Predicts Dasatinib Response In
Published OnlineFirst September 22, 2017; DOI: 10.1158/1078-0432.CCR-17-1549 Biology of Human Tumors Clinical Cancer Research CD90 Expression Controls Migration and Predicts Dasatinib Response in Glioblastoma Tony Avril1,2, Amandine Etcheverry3, Raphael€ Pineau1, Joanna Obacz1, Gwena ele€ Jegou1,2, Florence Jouan1, Pierre-Jean Le Reste1,4, Masumeh Hatami5, Rivka R. Colen5,6, Brett L. Carlson7, Paul A. Decker7, Jann N. Sarkaria7, Elodie Vauleon 1,2,3, Dan Cristian Chiforeanu8, Anne Clavreul9, Jean Mosser3, Eric Chevet1,2, and Veronique Quillien1,2,3 Abstract Purpose: CD90 (Thy-1) is a glycophosphatidylinositol- migration gene signature and with invasive tumor features. Mod- anchored glycoprotein considered as a surrogate marker for a ulation of CD90 expression in GBM cells dramatically affected variety of stem cells, including glioblastoma (GBM) stem cells their adhesion and migration properties. Moreover, orthotopic (GSC). However, the molecular and cellular functions of CD90 xenografts revealed that CD90 expression induced invasive phe- remain unclear. notypes in vivo. Indeed, CD90 expression led to enhanced SRC and Experimental Design: The function of CD90 in GBM was FAK signaling in our GBM cellular models and GBM patients' addressed using cellular models from immortalized and primary specimens. Pharmacologic inhibition of these signaling nodes GBM lines, in vivo orthotopic mouse models, and GBM specimens' blunted adhesion and migration in CD90-positive cells. Remark- transcriptome associated with MRI features from GBM patients. ably, dasatinib blunted CD90-dependent GBM cell invasion CD90 expression was silenced in U251 and GBM primary cells in vivo and killed CD90high primary GSC lines. and complemented in CD90-negative U87 cells. -

Detection of Cytogenetic Aberrations Both in CD90 (Thy-1)-Positive And
Leukemia (1999) 13, 1770–1775 1999 Stockton Press All rights reserved 0887-6924/99 $15.00 http://www.stockton-press.co.uk/leu Detection of cytogenetic aberrations both in CD90 (Thy-1)-positive and (Thy-1)- negative stem cell (CD34) subfractions of patients with acute and chronic myeloid leukemias C Brendel1, B Mohr1, C Schimmelpfennig1,JMu¨ller1, M Bornha¨user1, M Schmidt1, M Ritter1, G Ehninger1 and A Neubauer2 1Universita¨tsklinikum Carl Gustav Carus, Medizinische Klinik I, Dresden; and 2Universita¨tsklinikum der Philipps-Universita¨t Marburg, Abt. fu¨r Ha¨matologie, Onkologie und Immunologie, Zentrum fu¨r Innere Medizin, Marburg, Germany Acute myeloid leukemia (AML) and chronic myeloid leukemia early stem cells from malignant progenitor cells via distinct (CML) are thought to arise from malignant hematopoietic pro- surface marker molecules is a challenging perspective, since genitor cells representing early and undifferentiated stem cell various improved cell selection methods have been recently clones. In CML there is evidence for a progenitor cell subset 4 free of leukemic clones, depending on the course of the dis- applied. ease. Additionally, it has been suggested that in AML, the early Acute myeloid leukemia is also considered to be an early stem cell compartment (CD34+/90+) does not harbor the malig- stem cell disease with fulminant lethal course if untreated. nant clone. We analyzed white blood cells from leukemia Since only a minority of patients achieve long-term complete patients for the presence of aberrant cells in stem cell subfrac- remission, bone marrow or stem cell transplantation is still the tions. Sixteen patients with CML, six patients with AML, two patients with acute lymphatic leukemia (ALL) and one with treatment of choice if appropriate donor cells are available. -

CD90 Serves As Differential Modulator of Subcutaneous and Visceral
Pan et al. Stem Cell Research & Therapy (2019) 10:355 https://doi.org/10.1186/s13287-019-1459-7 RESEARCH Open Access CD90 serves as differential modulator of subcutaneous and visceral adipose-derived stem cells by regulating AKT activation that influences adipose tissue and metabolic homeostasis Zhenzhen Pan1†, Zixin Zhou1†, Huiying Zhang1, Hui Zhao1,2, Peixuan Song3, Di Wang1, Jilong Yin1, Wanyi Zhao1, Zhaoxiang Xie1, Fuwu Wang4, Yan Li5, Chun Guo1, Faliang Zhu1, Lining Zhang1 and Qun Wang1* Abstract Background: White adipose tissue includes subcutaneous and visceral adipose tissue (SAT and VAT) with different metabolic features. SAT protects from metabolic disorders, while VAT promotes them. The proliferative and adipogenic potentials of adipose-derived stem cells (ADSCs) are critical for maintaining adipose tissue homeostasis through driving adipocyte hyperplasia and inhibiting pathological hypertrophy. However, it remains to be elucidated the critical molecules that regulate different potentials of subcutaneous and visceral ADSCs (S-ADSCs, V- ADSCs) and mediate distinct metabolic properties of SAT and VAT. CD90 is a glycosylphosphatidylinositol-anchored protein on various cells, which is also expressed on ADSCs. However, its expression patterns and differential regulation on S-ADSCs and V-ADSCs remain unclear. Methods: S-ADSCs and V-ADSCs were detected for CD90 expression. Proliferation, colony formation, cell cycle, mitotic clonal expansion, and adipogenic differentiation were assayed in S-ADSCs, V-ADSCs, or CD90-silenced S-ADSCs. Glucose tolerance test and adipocyte hypertrophy were examined in mice after silencing of CD90 in SAT. CD90 expression and its association with CyclinD1 and Leptin were analyzed in adipose tissue from mice and humans. -

T Cells Into Heart +CD8 Expression Reduces Migration of Pathogenic
Abrogation of Functional Selectin-Ligand Expression Reduces Migration of Pathogenic CD8+ T Cells into Heart This information is current as Yi Hong Cai, Angeles Alvarez, Pilar Alcaide, Paurene of September 24, 2021. Duramad, Yaw-Chin Lim, Petr Jarolim, John B. Lowe, Francis W. Luscinskas and Andrew H. Lichtman J Immunol 2006; 176:6568-6575; ; doi: 10.4049/jimmunol.176.11.6568 http://www.jimmunol.org/content/176/11/6568 Downloaded from References This article cites 32 articles, 16 of which you can access for free at: http://www.jimmunol.org/content/176/11/6568.full#ref-list-1 http://www.jimmunol.org/ Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication by guest on September 24, 2021 *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2006 by The American Association of Immunologists All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. The Journal of Immunology Abrogation of Functional Selectin-Ligand Expression Reduces Migration of Pathogenic CD8؉ T Cells into Heart1 Yi Hong Cai,* Angeles Alvarez,* Pilar Alcaide,* Paurene Duramad,* Yaw-Chin Lim,‡ Petr Jarolim,† John B. -

©Ferrata Storti Foundation
Acute Leukemias original paper haematologica 2001; 86:154-161 Impact of CD133 (AC133) and CD90 http://www.haematologica.it/2001_02/0154.htm expression analysis for acute leukemia immunophenotyping CHRISTIAN WUCHTER,* RICHARD RATEI,* GÜNTHER SPAHN,* CLAUDIA SCHOCH,° JOCHEN HARBOTT,# SUSANNE SCHNITTGER,° TORSTEN HAFERLACH,° URSULA CREUTZIG,@ CHRISTIAN SPERLING,* LEONID KARAWAJEW,* WOLF-DIETER LUDWIG* *Dept. of Hematology, Oncology and Tumor Immunology, Robert- Rössle-Clinic, Charité, Humboldt-University of Berlin, °Dept. of Internal Medicine III, Ludwig-Maximilians-University of München, Correspondence: Christian Wuchter, M.D., Robert-Rössle-Clinic, Charité, #Oncogenetic Laboratory, Children’s Hospital, Justus-Liebig-Uni- Humboldt University of Berlin, Lindenberger Weg 80, 13125 Berlin, Ger- versity of Gießen, @Dept. of Hematology-Oncology, University Chil- many. Phone: international +0049-30-94171362 - Fax: international +0049-30-94171308 - E-mail: [email protected] dren's Hospital, Münster, Germany Background and Objectives. AC133 is a novel monoclonal cute leukemias derive from either malignant, antibody (Moab) reacting with a population of imma- transformed, uncommitted multipotent stem cells ture/primitive or granulo-monocytic committed CD34+ve Aor lineage-restricted progenitor cells.1-3 So far, cells. Up to now, only few studies with small numbers of cas- CD34 is the most commonly used antigen to define es have examined AC133 (recently designated CD133) immature hematopoietic progenitor cells.4 In acute expression in acute leukemia. To determine the value of this leukemia immunophenotyping, CD34 is not lineage- Moab for acute leukemia immunophenotyping, we investi- restricted and thus not useful for distinguishing acute gated a large series of leukemic cell samples for their reac- myeloid leukemia (AML) from acute lymphoblastic tivity with Moab AC133. -
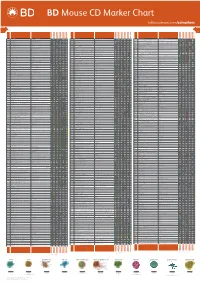
Mouse CD Marker Chart Bdbiosciences.Com/Cdmarkers
BD Mouse CD Marker Chart bdbiosciences.com/cdmarkers 23-12400-01 CD Alternative Name Ligands & Associated Molecules T Cell B Cell Dendritic Cell NK Cell Stem Cell/Precursor Macrophage/Monocyte Granulocyte Platelet Erythrocyte Endothelial Cell Epithelial Cell CD Alternative Name Ligands & Associated Molecules T Cell B Cell Dendritic Cell NK Cell Stem Cell/Precursor Macrophage/Monocyte Granulocyte Platelet Erythrocyte Endothelial Cell Epithelial Cell CD Alternative Name Ligands & Associated Molecules T Cell B Cell Dendritic Cell NK Cell Stem Cell/Precursor Macrophage/Monocyte Granulocyte Platelet Erythrocyte Endothelial Cell Epithelial Cell CD1d CD1.1, CD1.2, Ly-38 Lipid, Glycolipid Ag + + + + + + + + CD104 Integrin b4 Laminin, Plectin + DNAX accessory molecule 1 (DNAM-1), Platelet and T cell CD226 activation antigen 1 (PTA-1), T lineage-specific activation antigen 1 CD112, CD155, LFA-1 + + + + + – + – – CD2 LFA-2, Ly-37, Ly37 CD48, CD58, CD59, CD15 + + + + + CD105 Endoglin TGF-b + + antigen (TLiSA1) Mucin 1 (MUC1, MUC-1), DF3 antigen, H23 antigen, PUM, PEM, CD227 CD54, CD169, Selectins; Grb2, β-Catenin, GSK-3β CD3g CD3g, CD3 g chain, T3g TCR complex + CD106 VCAM-1 VLA-4 + + EMA, Tumor-associated mucin, Episialin + + + + + + Melanotransferrin (MT, MTF1), p97 Melanoma antigen CD3d CD3d, CD3 d chain, T3d TCR complex + CD107a LAMP-1 Collagen, Laminin, Fibronectin + + + CD228 Iron, Plasminogen, pro-UPA (p97, MAP97), Mfi2, gp95 + + CD3e CD3e, CD3 e chain, CD3, T3e TCR complex + + CD107b LAMP-2, LGP-96, LAMP-B + + Lymphocyte antigen 9 (Ly9), -

TGF-Β1 Accelerates the Hepatitis B Virus X-Induced Malignant Transformation of Hepatic Progenitor Cells by Upregulating Mir- 199A-3P
Oncogene (2020) 39:1807–1820 https://doi.org/10.1038/s41388-019-1107-9 ARTICLE TGF-β1 accelerates the hepatitis B virus X-induced malignant transformation of hepatic progenitor cells by upregulating miR- 199a-3p 1,2 3 1 1 1 1 1 Ke-shuai Dong ● Yan Chen ● Guang Yang ● Zhi-bin Liao ● Hong-wei Zhang ● Hui-fang Liang ● Xiao-ping Chen ● Han-hua Dong1 Received: 16 October 2018 / Revised: 29 October 2019 / Accepted: 6 November 2019 / Published online: 18 November 2019 © The Author(s) 2019. This article is published with open access Abstract Increasing evidence has suggested that liver cancer arises partially from transformed hepatic progenitor cells (HPCs). However, the detailed mechanisms underlying HPC transformation are poorly understood. In this study, we provide evidence linking the coexistence of hepatitis B virus X protein (HBx) and transforming growth factor beta 1 (TGF-β1) with miR-199a-3p in the malignant transformation of HPCs. The examination of liver cancer specimens demonstrated that HBx and TGF-β1 expression was positively correlated with epithelial cell adhesion molecule (EpCAM) and cluster of 1234567890();,: 1234567890();,: differentiation 90 (CD90). Importantly, EpCAM and CD90 expression was much higher in the specimens expressing both high HBx and high TGF-β1 than in those with high HBx or high TGF-β1 and the double-low-expression group. HBx and TGF-β1 double-high expression was significantly associated with poor prognosis in primary liver cancer. We also found that HBx and TGF-β1 induced the transformation of HPCs into hepatic cancer stem cells and promoted epithelial–mesenchymal transformation, which was further enhanced by concomitant HBx and TGF-β1 exposure. -

CD System of Surface Molecules
THE CD SYSTEM OF LEUKOCYTE APPENDIX 4A SURFACE MOLECULES Monoclonal Antibodies to Human Cell Surface Antigens APPENDIX 4A Alice Beare,1 Hannes Stockinger,2 Heddy Zola,1 and Ian Nicholson1 1Women’s and Children’s Health Research Institute, Women’s and Children’s Hospital, Adelaide, Australia 2Institute of Immunology, University of Vienna, Vienna ABSTRACT Many of the leukocyte cell surface molecules are known by “CD” numbers. In this Appendix, a short introduction describes the history and the use of CD nomenclature and provides a few key references to enable access to the wider literature. This is followed by a table that lists all human molecules with approved CD names, tabulating alternative names, key structural features, cellular expression, major known functions, and usefulness of the molecules or antibodies against them in research or clinical applications. Curr. Protoc. Immunol. 80:A.4A.1-A.4A.73. C 2008 by John Wiley & Sons, Inc. Keywords: CD nomenclature r HLDA r HCDM r leukocyte marker r human leukocyte differentiation r antigens INTRODUCTION During the last 25 years, large numbers of monoclonal antibodies (MAbs) have been pro- duced that have facilitated the purification and functional characterization of a plethora of leukocyte surface molecules. The antibodies have been even more useful as markers for cell populations, allowing the counting, separation, and functional study of numer- ous subsets of cells of the immune system. A series of international workshops were instrumental in coordinating this development through multi-laboratory “blind” studies of thousands of antibodies. These HLDA (Human Leukocyte Differentiation Antigens) Workshops have, up until now, defined 500 different entities and assigned them cluster of differentiation (CD) designations. -
![Anti-Cd11c Antibody [BU15] (APC) (ARG53761)](https://docslib.b-cdn.net/cover/6543/anti-cd11c-antibody-bu15-apc-arg53761-3626543.webp)
Anti-Cd11c Antibody [BU15] (APC) (ARG53761)
Product datasheet [email protected] ARG53761 Package: 100 tests anti-CD11c antibody [BU15] (APC) Store at: 4°C Summary Product Description APC-conjugated Mouse Monoclonal antibody [BU15] recognizes CD11c Tested Reactivity Hu, Mk Tested Application FACS Specificity The clone BU15 reacts with CD11c (alphaX, p150), a 150 kDa integrin expressed mainly on dendritic cells and tissue macrophages. HLDA III; WS Code M 256 HLDA V; WS Code AS S143 HLDA VI; WS Code AS Ref.6 Host Mouse Clonality Monoclonal Clone BU15 Isotype IgG1 Target Name CD11c Immunogen Dendritic cells of synovial fluid Conjugation APC Alternate Names CD antigen CD11c; Leu M5; CD11C; SLEB6; Integrin alpha-X; Leukocyte adhesion glycoprotein p150,95 alpha chain; Leukocyte adhesion receptor p150,95; CD11 antigen-like family member C Application Instructions Application table Application Dilution FACS 10 µl / 10^6 cells Application Note * The dilutions indicate recommended starting dilutions and the optimal dilutions or concentrations should be determined by the scientist. Calculated Mw 128 kDa Properties Form Liquid Purification Note The purified antibody is conjugated with cross-linked Allophycocyanin (APC) under optimum conditions. The conjugate is purified by size-exclusion chromatography and adjusted for direct use. No reconstitution is necessary. Buffer PBS, 15 mM Sodium azide and 0.2% (w/v) high-grade protease free BSA Preservative 15 mM Sodium azide Stabilizer 0.2% (w/v) high-grade protease free BSA Storage instruction Aliquot and store in the dark at 2-8°C. Keep protected from prolonged exposure to light. Avoid www.arigobio.com 1/2 repeated freeze/thaw cycles. Suggest spin the vial prior to opening. -

Markers and Methods to Verify Mesenchymal Stem Cell Identity, Potency, and Quality Scott Schachtele, Ph.D., Christine Clouser, Ph.D., and Joy Aho, Ph.D
WHITE PAPER Markers and Methods to Verify Mesenchymal Stem Cell Identity, Potency, and Quality Scott Schachtele, Ph.D., Christine Clouser, Ph.D., and Joy Aho, Ph.D. ABSTRACT Mesenchymal stem cells (MSCs) are multipotent cells that are functionally defined by their capacity to self-renew and their ability to differentiate into multiple cell types including adipocytes, chondrocytes, and osteocytes. Translation of MSC-based therapies has been confounded by MSC population heterogeneity as well as non-standardized methods for their definition and characterization. This white paper begins by defining and discussing the evolution of MSC nomenclature. It then provides a detailed description of MSC markers and how they may vary by tissue source and species. Ultimately, this review discusses how to standardize MSC characterization by selecting markers for isolation, characterization, and validation. KEY TOPICS • Defining Mesenchymal Stem Cells • MSC Marker Variation by Species • Established and New MSC Markers • Methods for MSC Identification and Characterization • Methods for MSC Isolation • Media Definitions for MSC Expansion INTRODUCTION Mesenchymal stem cells (MSCs) are multipotent cells that adhere to plastic, have a Box 1. Minimal Experimental Criteria for MSC fibroblast-like morphology, express a specific set of surface antigens, and differentiate into as proposed by the International Society for adipocytes, chondrocytes, and osteocytes.1 Clinically, MSCs are of interest for their ability to Cellular Therapy modulate the immune system as well as their potential to regenerate tissues. However, the translation of MSC-based therapies has been hindered by the heterogeneity of the isolated • Adherence to plastic. cells as well as the lack of standardized methods for their definition and characterization. -

Reconstruction of Human Elastic Cartilage by a CD44 CD90 Stem Cell
Reconstruction of human elastic cartilage by a CD44+ CD90+ stem cell in the ear perichondrium Shinji Kobayashia,b,1, Takanori Takebea,1, Midori Inuia, Sayaka Iwaia, Hiroomi Kana, Yun-Wen Zhenga, Jiro Maegawac, and Hideki Taniguchia,d,2 Departments of aRegenerative Medicine and cPlastic and Reconstructive Surgery, Yokohama City University Graduate School of Medicine, Yokohama, Kanagawa 236-0004, Japan; dAdvanced Medical Research Center, Yokohama City University, Yokohama, Kanagawa 236-0004, Japan; and bDepartment of Plastic and Reconstructive Surgery, Kanagawa Children’s Medical Center, Yokohama 232-8555, Japan Edited by Robert Langer, Massachusetts Institute of Technology, Cambridge, MA, and approved July 14, 2011 (received for review June 16, 2011) Despite the great demands for treating craniofacial injuries or ECM to support 3D structures (18–20). The identification of an abnormalities, effective treatments are currently lacking. One alternative source of stem cells with high chondrogenic potential promising approach involves human elastic cartilage reconstruc- is crucial to realize elastic cartilage regenerative therapy. tion using autologous stem/progenitor populations. Nevertheless, Previous papers have suggested that some of the cells derived definitive evidence of the presence of stem cells in human auricular from rabbit auricular (ear) perichondrium appear to be a stem or progenitor population, on the basis of in vitro multidifferentia- cartilage remains to be established. Here, we demonstrate that – human auricular perichondrium, which can be obtained via a tion assays or label-retaining cell assays (21 23). However, con- minimally invasive approach, harbors a unique cell population, siderable heterogeneities between these studies have precluded definitive evidence of stem cells in elastic cartilage, and the ther- termed as cartilage stem/progenitor cells (CSPCs).