Management of Asthma at Primary Care Level
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Senarai Premis Yang Berjaya Mendapat Pensijilan (Mesti)
SENARAI PREMIS YANG BERJAYA MENDAPAT PENSIJILAN (MESTI) BIL NAMA SYARIKAT ALAMAT SYARIKAT NAMA WAKIL SYARIKAT NO TELEFON PRODUK LOT 19, JALAN INDUSTRI, KAWASAN PERINDUSTRIAN, 02000 Tel: 04-9853089 1 IGLOO ICE SDN BHD CHUA SHUI CHWN AIS KUALA PERLIS Faks: 04-9853122 2 RAROSYA ENTERPRISE 42 KAMPUNG BANGGOL SENA KANGAR RAFEDAH BINTI ISMAIL@MUSA 017-5121048 SOS CILI KOMPLEKS GERAK TANI WAWASAN E-1 (MADA) 02700 SIMPANG 3 PPK E-1 SIMPANG EMPAT EMPAT AL-HIDAYAH BT ALIAS 04-9807248 / 012-5883542 MINI POPIA PERLIS LOT 7 & 8, KAWASAN PERINDUSTRIAN MIEL JEJAWI FASA 2, 013-5846717 / 4 HPA INDUSTRIES SDN. BHD. A. ZAKARIA ABU BAKAR / NORASYIKIN KOPI RADIX, RADIX DIET JALAN JEJAWI SEMATANG, 02600 ARAU, PERLIS 019-6330727/049760741 5 SBA FOOD ENTERPRISE AB, JALAN KG SYED OMAR 01000 KANGAR SARIMAH BT ANI 017-5319490 REMPEYEK NO. 5&6, KAW PERINDUSTRIAN RINGAN, JALAN BESAR 02100 6 MEGA DUTAMAS SDN. BHD. TEOH YICK XIANG 017-4128967 COKLAT PADANG BESAR, PERLIS LOT A-5, KAWASAN MIEL, JEJAWI PHASE 1, 02600 JEJAWI, 019-4752188 7 ATLAS EDIBLE ICE SDN BHD LOW BEE BEE Ais tiub & Ais hancur PERLIS. 04-9777388 019-4907826 NO 2, 4 & 6, JALAN MURAI BATU, TAMAN KIM, 02100 PADANG 8 MEGA DUTAMAS SDN. BHD. YAP YUEN SER 04-9492788 COKLAT BESAR, PERLIS 04-9491788(F) 9 TERIAU ENTERPRISE NO 12 A KAMPUNG GUAR UJUNG BATU UTAN AJI 01000 KANGAR JAMINAH BT TERIAH 04-9766071 KACANG BERSALUT 109, LORONG SRI INAI, KAMPUNG JEJAWI DALAM 02600 ARAU 10 FAUZIAH BT ISMAIL FAUZIAH BINTI ISMAIL 017-4614385 REMPEYEK PERLIS LOT 555, JALAN BATAS LINTANG, 02700 SIMPANG EMPAT, 11 PERUSAHAAN PASTA ITIFAQ MOHD TARMIZIE ROMLI 017-5568953 MEE KUNING PERLIS 019-4549889 PERTUBUHAN PELADANG KAWASAN PAYA, KM 4 JALAN KAKI 12 PPK PAYA RAHMAH BT SALAMAT 04-9760280 CIP BUAH-BUAHAN BUKIT, 01000 KANGAR PERLIS 04-9761140 13 SYAFI BAKERY 500, JALAN MASJID KG. -

Tourism and Political Boundaries: Border Markets As Tourist Attractions
Mat Som, Ahmad Puad (First Author) School of Housing, Building & Planning, Universiti Sains Malaysia a h m a d . m at - s o m,.d st rat h . ac. u k. a h m ad p u ad_m at s o m (rJ) ya h o o. c o. u k Mohamed. Badaruddin School of Housing, Building & Planning, Universiti Sains Malaysia badaf(Dusm.my Wong, Kong-Yew Faculty of Economics and Management, Universiti Putra Malaysia kywon gl'r? eco n. upm. edu. m ), Title: Tourism and Political Boundaries: Border Markets as Tourist Attractions Abstract Tourism appears to be an increasingly important industry in many border areas because many tourist destinations exist across boundaries. In many ways, the existence and functions of political boundaries influence the nature of the tourism industry itself and the spatial development of the tourist destinations (Timothy, 1995). Eriksson (1979) further suggests that the level ofattractiveness ofborder areas depends on the natural, social and cultural environment near the border and the degree of freedom or difficulty in crossing it. By conducting in-depth interviews, this study attempts to investigate whether the growth of tourism industry on both sides of Malaysia and Thailand promotes local economy as well as cohesion between the two tourist areas and between communities with dissimilar cultures. The findings argue that the growth of tourism-related activities especially the border market has increased local participation in tourism. But, the degree of involvement tends to decrease over time due to high permeability between two different societies, which allows intrusion of foreign traders into local territories. -

Soil Liquefaction Hazard Assessment Along Shoreline of Peninsular Malaysia
SOIL LIQUEFACTION HAZARD ASSESSMENT ALONG SHORELINE OF PENINSULAR MALAYSIA HUZAIFA BIN HASHIM FACULTY OF ENGINEERING UNIVERSITY OF MALAYA KUALA LUMPUR 2017 SOIL LIQUEFACTION HAZARD ASSESSMENT ALONG SHORELINE OF PENINSULAR MALAYSIA HUZAIFA BIN HASHIM THESIS SUBMITTED IN FULFILMENT OF THE REQUIREMENTS FOR THE DEGREE OF DOCTOR OF PHILOSOPHY FACULTY OF ENGINEERING UNIVERSITY OF MALAYA KUALA LUMPUR 2017 UNIVERSITY OF MALAYA ORIGINAL LITERARY WORK DECLARATION Name of Candidate: HUZAIFA BIN HASHIM Matric No: KHA110047 Name of Degree: DOCTOR OF PHILOSOPHY Title of Project Paper/Research Report/Dissertation/Thesis (―this Work‖): SOIL LIQUEFACTION HAZARD ASSESSMENT ALONG SHORELINE OF PENINSULAR MALAYSIA Field of Study: GEOTECHNICAL ENGINEERING I do solemnly and sincerely declare that: (1) I am the sole author/writer of this Work; (2) This Work is original; (3) Any use of any work in which copyright exists was done by way of fair dealing and for permitted purposes and any excerpt or extract from, or reference to or reproduction of any copyright work has been disclosed expressly and sufficiently and the title of the Work and its authorship have been acknowledged in this Work; (4) I do not have any actual knowledge nor do I ought reasonably to know that the making of this work constitutes an infringement of any copyright work; (5) I hereby assign all and every rights in the copyright to this Work to the University of Malaya (―UM‖), who henceforth shall be owner of the copyright in this Work and that any reproduction or use in any form or by any means whatsoever is prohibited without the written consent of UM having been first had and obtained; (6) I am fully aware that if in the course of making this Work I have infringed any copyright whether intentionally or otherwise, I may be subject to legal action or any other action as may be determined by UM. -

Urban Land Use & Territorial Planning
PRESENTATIONS SPECIAL SESSION 6 SPECIAL SESSION 6: Urban Land Use and Territorial Planning in the Pacific Host Sponsors and Co-organizers SPECIAL SESSION 6: Urban Land Use and Territorial Planning in the Pacific Day 2 (2 July, 2019. Nadi, Republic of Fiji). Organized by: Commonwealth Association of Planners (CAP) Speakers: • Mr. Bryce Julyan, Vice President (NZ-Pacific), Commonwealth Association of Planners • Dr. Wendy Saunders – Senior Social Scientist, GNS Science, New Zealand • Ms. Lesley Hopkins - Technical Director, Beca International Consultants, New Zealand • Dr Azmizam Abdul Rashid, Urbanice, Malaysia This Special Session was hosted by the Commonwealth Association of Planners (CAP). CAP is a major global institution in planning and is playing an increasingly significant role in the worldwide promotion of planning as a fundamental part of governance for sustainable human settlement. CAP currently represents over 40 000 planners from 27 countries throughout the Commonwealth including African, Asian, Australasian and Caribbean countries. Drawing on examples and observations of planners and practitioners from Commonwealth members the session ex- amined urban land use and territorial planning in the context of rapid urbanisation and climate change, and looked at its application in the Pacific Region. The presentations illustrated urban and territorial land use planning projects and tools that are being applied and developed to plan for land use changes in the context of coastal, tropical and island nations facing climate change and urbanisation rates that stretch land and infrastructure resources. Presentations were followed by a panel discussion on the key challenges, and then group discussion on what tools and actions can we use to improve, strengthen plans and planning to achieve sustainable, positive outcomes for our land use and urban areas, whilst acknowledging and responding to climate change by building resilience in our urban settlements. -
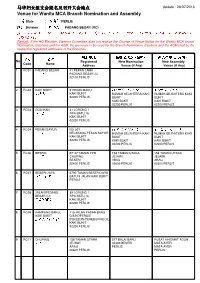
Venue for Wanita MCA Branch Nomination and Assembly 马华妇女
马华妇女组支会提名及召开大会地点 Update : 26/07/2013 Venue for Wanita MCA Branch Nomination and Assembly 州属 State : 玻璃市 PERLIS 区会 Division : 巴冬勿杀 PADANG BESAR (RC ) 注注注:如果总部选举指导委员会没有收到更换提名、大会或选举地点通知,妇女组支会的提名、大会或选举地点必须是该支 会的注册地址。 Remark : If the HQ Elections Steering Committee does not receive the Change of Venue Notice for the Wanita MCA branch Nomination, Elections and the AGM, the premises to be used for the Branch Nomination, Elections and the AGM shall be the respective registered addresses of the Branches. 注册地址 新提名地点(((如有(如有))) 新大会地点(((如有(如有))) 编号 名称 No Registered New Nomination New Assembly Code Name Address Venue (if Any) Venue (if Any) 1 RC01 PADANG BESAR 41 PEKAN LAMA 巴冬勿杀 PADANG BESAR (U) 02100 PERLIS 2 RC02 KAKI BUKIT 5 PEKAN BARU 加基武吉老人院礼堂 加基武吉老人院礼堂 加基武吉 KAKI BUKIT RUMAH SEJAHTERA KAKI RUMAH SEJAHTERA KAKI 02200 PERLIS BUKIT BUKIT KAKI BUKIT KAKI BUKIT 02200 PERLIS 02200 PERLIS 3 RC03 GUA IKAN 31 LORONG 1 拿督公 RPA BATU 16 KAKI BUKIT 02200 PERLIS 4 RC04 PEKAN SAYUR NO 307 加基武吉老人院礼堂 加基武吉老人院礼堂 长江寮 BELAKANG PEKAN SAYOR RUMAH SEJAHTERA KAKI RUMAH SEJAHTERA KAKI KAKI BUKIT BUKIT BUKIT 02200 PERLIS KAKI BUKIT KAKI BUKIT 02200 PERLIS 02200 PERLIS 5 RC06 BESERI EF 47 TAMAN PPB 158 TAMAN UTARA 158 TAMAN UTARA 柏斯里 CHUPING JEJAWI JEJAWI BESERI ARAU ARAU 02400 PERLIS 02600 PERLIS 02600 PERLIS 6 RC07 BESERI JAYA 2790 TAMAN BESERI JAYA 柏斯里再也 BATU 9 JALAN KAKI BUKIT PERLIS 7 RC08 JALAN PEDANG 39 LORONG 1 BESAR (U) RPA BATU 16 巴登勿刹路 KAKI BUKIT 02200 PERLIS 8 RC09 KAMPUNG BARU, 115 JALAN PASAR BARU KAKI BUKIT D/A KOPERASI 加基武吉甘光峇汝 PEKEBUN-PEKEBUN KECIL KAKI -

Map Guide PERLIS English.Pdf
Places of Interest MALAYSIA Perlis 1A 4 8 Situated in the heart of Southeast Asia, Malaysia Known as the Northern Gem, Perlis is the northern gateway to Malaysia. Despite its small size, Perlis is a vibrant destination with a diversity of cultures Thailand has an abundance of attractions that make it a great MAP OF MALAYSIA Sulu and traditions. This tropical paradise boasts pristine PERLIS Sea destination, be it for adventure-lovers, shopping jungles and verdant national parks that are teeming KEDAH enthusiasts or holidaymakers in search of a relaxing with numerous species of birds and wildlife. Malaysia’s KELANTAN vacation. Perlis is flanked by Kedah in the south PENANG sun-drenched islands and beaches are home to a LABUAN SABAH TERENGGANU stunning range of marine life. Its natural wealth is and Thailand (Malaysia’s northern neighbor) in the PERAK north. The state is characterised by sprawling paddy Brunei complemented by magnificent modern landmarks Darussalam plains and picturesque views of the countryside, and heritage buildings. There is something to charm PAHANG South China Sea interspersed with rustic villages, limestone outcrops SELANGOR Celebes every visitor, be it a history-lover, nature-enthusiast, KUALA LUMPUR Sea and serene lakes. Its capital city, PERLIS STATE PARK, WANG KELIAN EMAS KERAJANG DUTY-FREE COMPLEX, PADANG BESAR GALERI DIRAJA (PERLIS ROYAL GALLERY), ARAU sun-seeker or an avid shopper. Explore the length PUTRAJAYA Kangar, is a great destination NEGERI SEMBILAN SARAWAK and breadth of the country to discover the many This 5,000 hectare park is home to Malaysia’s only semi deciduous Located at the northern border of Malaysia, this is one of the most The Royal Gallery showcases an impressive collection of the with delightful orchards and MELAKA White Meranti Gerutu Seasonal Forest, as well as the 500-million state’s royal regalia, portraits, ceremonial court items, ancient attractions of Malaysia! JOHOR popular shopping spots for locals and visitors from around the verdant recreational parks. -

Kuala Lumpur
KUALA LUMPUR 50000 - Kuala Lumpur 50280 - Kuala Lumpur 50010 - Jln Tunku Abd Rahman 50290 - Kuala Lumpur 50020 - Jln Raja Chulan 50300 - Jln Chow Kit 50030 - Setapak 50310 - Kuala Lumpur 50040 - Jln Tun Perak 50320 - Jln Putra 50050 - Lebuh Pasar 50330 - Tmn Permata 50060 - Jln Hang Kasturi 50350 - Jln Raja Laut 50070 - Jln Sultan Hishamudin 50360 - Jln Raja Laut 50080 - KLCC 50370 - Jln Tun Razak 50081 - KLCC 50380 - Jln Parlimen 50082 - KLCC 50390 - Jln Tiong 50083 - KLCC 50400 - Jln Tun Razak 50084 - KLCC 50410 – Brickfields 50085 - KLCC 50420 – Jelatek 50086 - KLCC 50430 - Yap Kuan Seng 50087 - KLCC 50440 - Yap Kuan Seng 50088 - KLCC 50450 - Kia Peng 50089 - KLCC 50460 - Kg Attap 50090 - Kuala Lumpur 50470 – Brickfields 50100 - Jln Chow Kit 50480 - Mont Kiara 50110 - Jln Munshi Abdullah 50490 - Bukit Damansara 50120 - Jln Munshi Abdullah 50500 - Jln Tan Cheng Lock 50130 - Lebuh Ampang 50501 - Kuala Lumpur 50140 - Pertama Kompleks 50502 - Jln Dato Onn 50150 - Jln Hang Jebat 50503 - Kuala Lumpur 50160 - Jln Pahang 50504 - Jln Raja Laut 50170 - Jln Tun Sambathan 50505 - Kuala Lumpur 50180 - Sri Hartamas 50506 - Jln Duta 50190 - Jln TAR 50507 - Jln Damansara 50200 - Bkt Bintang 50508 - Bukit Damansara 50210 - Kuala Lumpur 50510 - Jln Maharajalela 50220 - Jln Sultan Ismail 50511 - Kuala Lumpur 50230 - Jln Sultan Ismail 50512 - Jln Tangsi 50240 - Jln Sultan Ismail 50513 - Kuala Lumpur 50250 - Jln Sultan Ismail 50514 - Jln Cenderasari 50260 - Jln Sultan Ismail 50515 - Jln Dato Onn 50270 - Kuala Lumpur 50517 - Jln Raja Laut 50519 - Jln Perdana -

Kaki Bukit 加基武吉 Perlis Date of Completion: April 2021
UTAR NEW VILLAGE COMMUNITY PROJECT REPORT NAME OF NEW VILLAGE: KAKI BUKIT 加基武吉 PERLIS Project carried out by: Student Name ID Number Course Year / Semester 1. NG YEE HOI YUKI 1704032 BF Y3S3 2. NG YEE WEE 1802980 BF Y3S3 DATE OF COMPLETION: APRIL 2021 KAKI BUKIT ABSTRACT Kaki Bukit is a new village established in 2016, and is not one of the traditional new villages created during the waning days of British rule. This new village is in Perlis, the smallest and northernmost state in Malaysia. The nearest town to this new village is Padang Besar, which is 15 km away. The main attraction in Kaki Bukit is Gua Kelam, the limestone cave that was gouged out during the tin-mining days. The main economic activities in the village are small businesses and agriculture. 2 KAKI BUKIT INTRODUCTION Kaki Bukit is located in Perlis, and 26 kilometres north of the state capital, Kangar. Perlis is the northernmost state in Malaysia and being the smallest, it has no districts. Padang Besar is the nearest town to Kaki Bukit and around 15 kilometres away on the boundary between Malaysia and Thailand. Wang Kelian is also on the border and 8 kilometres away. Because of the geographical factor, this new village is composed of Chinese and Thais (the latter’s population is very low). Its population in 2021 is approximately 1,700. When the village was founded in 2016, it had a population of almost 1800. Over the years, the population decreased by a small number only. Kaki Bukit, literally “foot hill” translated from Bahasa Malaysia, is surrounded by hills. -

SOALAN LAZIM PENYAKIT NOVEL CORONAVIRUS (COVID-19) 15 November 2020
SOALAN LAZIM PENYAKIT NOVEL CORONAVIRUS (COVID-19) 15 November 2020 Soalan 1: Apakah coronavirus? Coronavirus adalah satu keluarga besar virus yang menyebabkan jangkitan saluran pernafasan seperti Severe Acute Respiratory Syndrome (SARS) dan Middle East Respiratory Syndrome-related Coronavirus (MERS-CoV). Coronavirus terbaharu dan menjadi pandemik di seluruh dunia kini dikenali sebagai Novel Coronavirus 2019 (COVID-19). COVID-19 telah mula dikesan di negara China dengan kes pertama disahkan pada 7 Januari 2020 di Wuhan, Hubei, China. Dalam tempoh tiga (3) minggu seterusnya, kes-kes disahkan di Thailand, Nepal, Amerika Syarikat, Korea Selatan, Singapura, Perancis, Vietnam, Malaysia, Australia, Canada, Cambodia, Sri Lanka dan Jerman. Kes pertama di Malaysia disahkan pada 25 Januari 2020. Sehingga kini, penyakit COVID- 19 masih lagi menular di Malaysia. Sejak 20 September 2020, Malaysia sudah memasuki permulaan gelombang ketiga COVID-19 susulan peningkatan mendadak kes jangkitan virus COVID-19. Kementerian Kesihatan Malaysia dan pihak berkuasa terus menjalankan program dan aktiviti kawalan dan pencegahan bagi membendung wabak COVID-19 di Malaysia. Soalan 2: Bagaimanakah novel coronavirus 2019 (COVID-19) merebak? Cara penularan novel coronavirus COVID-19 daripada individu kepada individu yang lain adalah melalui titisan dari hidung atau mulut yang tersebar apabila seseorang yang dijangkiti COVID-19 batuk atau bersin. Titisan ini melekat pada objek dan permukaan di sekelilingnya. Orang lain yang menyentuh objek atau permukaan ini mempunyai risiko mendapat jangkitan COVID-19 apabila beliau menyentuh mata, hidung atau 1 mulutnya selepas menyentuh permukaan/objek yang tercemar. Seseorang itu juga boleh dijangkiti COVID-19 jika mereka berada dekat dengan pesakit COVID-19 yang batuk, bersin atau bercakap dalam jarak yang dekat. -

PERLIS 01000 Padang 1 TABIKA KEMAS BANGUNAN KHAS KG
Bil Nama Alamat Daerah Dun Parlimen Bil. Kelas JALAN SANTAN 01000 KANGAR PERLIS 01000 Padang 1 TABIKA KEMAS BANGUNAN KHAS KG. BONGKOK Perlis Santan 1 KANGAR Besar KG. TEBUK 02700 SIMPANG EMPAT PERLIS 02700 2 TABIKA KEMAS KG TEBUK Perlis Guar Sanji Arau 1 SIMPANG EMPAT 3 TABIKA KEMAS BANGUNAN JKR 01000 KANGAR PERLIS 01000 KANGAR Perlis Kayang Kangar 1 PERUMAHAN TAMAN EMAS JALAN BUKIT KETERI Padang 4 TABIKA KEMAS BANGUNAN KHAS TAMAN EMAS Perlis Beseri 1 02400 BESERI PERLIS 02400 BESERI Besar TABIKA KEMAS BANGUNAN KHAS BATU KG. BATU BERTANGKUP 02500 CHUPING PERLIS Padang 5 Perlis Chuping 1 BERTANGKUP 02500 CHUPING Besar TABIKA KEMAS BANGUNAN KHAS BATU KG. BATU BERTANGKUP 02500 CHUPING PERLIS Padang 6 Perlis Chuping 1 BERTANGKUP 2 02500 CHUPING Besar TABIKA KEMAS BANGUNAN KHAS BEREK POLIS TAMAN SERI AMAN JALAN SIMPANG EMPAT 7 Perlis Kayang Kangar 1 SERIAB 1 01000 KANGAR PERLIS 01000 KANGAR TABIKA KEMAS BANGUNAN KHAS BEREK POLIS TAMAN SERI AMAN JALAN SIMPANG EMPAT 8 Perlis Kayang Kangar 1 SERIAB 2 01000 KANGAR PERLIS 01000 KANGAR TABIKA KEMAS BANGUNAN KHAS FELDA MATA FELDA MATA AYER 02100 PADANG BESAR PERLIS Padang 9 Perlis Titi Tinggi 1 AYER 02100 PADANG BESAR Besar TABIKA KEMAS BANGUNAN KHAS FELDA RIMBA FELDA RIMBA MAS 02100 PADANG BESAR PERLIS Padang 10 Perlis Titi Tinggi 1 MAS 02100 PADANG BESAR Besar KEM UPP02100 PADANG BESAR (U) PERLIS 02100 Padang 11 TABIKA KEMAS BANGUNAN KHAS KEM UPP Perlis Titi Tinggi 1 PADANG BESAR Besar TABIKA KEMAS BANGUNAN KHAS KG BEHOR KG. BEHOR MASJID 01000 KANGAR PERLIS 01000 12 Perlis Kayang Kangar 1 MASJID KANGAR KG. -

Estimation of Drug Users and Injecting Drug Users in Malaysia
WORLD HEALTH ORGANIZATION, WESTERN PACIFIC REGION MINISTRY OF HEALTH MALAYSIA UNIVERSITI UTARA MALAYSIA ESTIMATION OF DRUG USERS AND INJECTING DRUG USERS IN MALAYSIA A study by the Ministry of Health (MOH), Malaysia In collaboration with Universiti Utara Malaysia (UUM) With Technical and Financial Support of World Health Organization (WHO) 1 Estimation of DU and IDU sub-population, MALAYSIA 2003 ACKNOWLEDGEMENTS The research team would like to thank the World Health Organization, Western Pacific Region (WHO-WPRO), specifically Dr Nguyen Thi Thanh THUY for the financial and technical assistance. We also thank Section of Aids/STD, Ministry of Health Malaysia for their technical and coordination support, National Drugs Agency who provided us with the official data, The Royal Malaysian Police, and the Home Minister for their support for the study. We also acknowledge assistance from the Office of the State Secretary, District Offices, local Police stations, JKKK, and NGOs such as PEMADAM and PENGASIH during the data collection phase of the study. We appreciate the overwhelming effort of our researchers, research assistants, enumerators and field workers, especially the recovering drug users who had help us day and night to access to respondents and areas which normally is avoided by the general public. 2 Estimation of DU and IDU sub-population, MALAYSIA 2003 Content Page 1 INTRODUCTION 1 1.1 Malaysian Drug Scenario 1 1.2 Drug Treatment and Rehabilitation program in Malaysia 1 1.3 National Drugs Information 3 1.4 Recommendation of Consensus -

Business Name Business Category Outlet Address State 2 Beradik Sparepart Automotive Kampung Belat, Mukim Rambai, Pendang, Kedah
Business Name Business Category Outlet Address State 2 beradik sparepart Automotive kampung belat, mukim rambai, Pendang, Kedah, Malaysia Kedah 3 BROS CAR SALOON Automotive Alor Setar Kedah Malaysia Kedah 39 Auto Creative Automotive 39 Auto Creative No 101tingkat bawah 215 Jalan Duku 4 Taman Star 05400 Alor Setar Kedah Malaysia Kedah 4 You Car Tinted Acc Automotive Ground floor Jalan Pandan Indah 1 Taman Pandan Indah Lunas Kedah Kedah A&F FUTURE ENTERPRISE Automotive 马来西亚吉打双溪大年 Kedah AAB MOTOR Automotive AAB MOTOR LOT 613 KG KELIBANG 13 Jalan Pandak Mayah 1 Kuah 07000 Langkawi Kedah Malaysia Kedah Aboo Utara Jdm Enterprise Automotive 248JALAN ZAMRUD 8 BANDAR BARU 08000 SUNGAI PETANI Kedah Ah Kieng Motor Automotive NO 168 POKOK SENA MUKIM PULAI BalingKDH - Kedah Kedah AIS KOOL Automotive KOMPLEKS SUKANNO 20Lebuhraya Sultan Abdul Halim Alor Star Alor Setar Malaysia Kedah Alatalat ganti gee heng Automotive 37F 19 Jalan Gangsa Mergong 2 Taman Pelangi Alor Setar Kedah Kedah Along jebat enterprise Automotive no477, lorong panglima, jalan tungku bendahara , Kedah AR Detailing Enterprise Automotive AR Detailing Enterprise F12 Kg Pmtg Damar Laut Lubok Buntar Bandar Baharu Kedah Malaysia Kedah AS Wira Tyre Car Service Automotive No. 4, Batu 1 1/2, Jalan Kuala KedahKedah Kedah ASSORTED TRADING SDN BHD Automotive No4 Seberang Jalan Putra Jalan Putra Bandar Alor Setar Alor Setar Kedah Malaysia Kedah BENGKEL MOTOR INDAH Automotive BENGKEL MOTOR INDAH 291 292 Lorong Perak 14 Kawasan Perusahaan Mergong Ii Alor Setar Kedah Malaysia Kedah Big Star Aircond Ele Automotive Big Star Aircond Electric No1 2 Jalan Senangin Taman Senangin 05150 Alor Setar Kedah Kedah BOON MOTOR ENTERPRISE Automotive NO85A SEBERANG JAYA PUTRA Alor Setar Kedah Malaysia Kedah CCY AUTOMOBILE Automotive 马来西亚吉打亚罗士打邮政编码: Kedah celaru enterprise Automotive Kampung Dato Syed Nahar 07000 Langkawi Kedah Malaysia Kedah CHAN WOEI JENG ENTERPRISE Automotive 95 Jalan Padang Matsirat Taman Berjaya Langkawi Kedah Malaysia Kedah Cheang Motor Sungai Petani Automotive NO.